Abstract
Purpose
The primary goal of this study is to compare clinical outcomes, complication rate, and survivorship in octogenarians who underwent total knee arthroplasty (TKA) or unicompartmental knee arthroplasty (UKA) by performing a matched cohort analysis.
Methods
We analyzed 75 medial UKAs performed by a single experienced surgeon. The included cases were matched with 75 TKAs performed during the same study period. Potential TKA matches used identical exclusion criteria. UKAs were age-, gender-, and body mass index (BMI)-matched at the rate of 1 UKA to 1 TKA from our departmental database. Clinical evaluation included the visual analog scale for pain, range of motion (ROM—flexion and extension), Knee Society Score (KSS), and Oxford Knee Score (OKS). Each patient was clinically evaluated on the day before the surgery (T0) and at two follow-ups at least 12 months (T1) and 24 months (T2) after the surgery. For the survivorship, revision was defined as failure of the implant (periprosthetic joint infection, periprosthetic fracture, or aseptic loosening), and survival was based on implant revision or patient death. Undesirable clinical developments that were not present at baseline or that increased in severity after treatment were classified as adverse events.
Results
The mean age at the time of the surgery was 82.1 ± 1.9 years for UKA and 81.5 ± 1.8 years for TKA (p = 0.06). The two groups differed in regard to surgical time (UKA 44.9 ± 7.2 min; TKA 54.4 ± 11.3 min; p < 0.001); furthermore, the UKA group showed better function (ROM; flexion and extension) than the TKA group at each follow-up time point (p < 0.05). Both groups reported a significant improvement in all clinical scores (KSS and OKS) when compared with their preoperative status (p < 0.05), while no differences were found between the groups at each follow-up (p > 0.05). The UKA group reported 7 (9.3%) failures, while TKA reported 6 failures. There were no survival differences between the groups (T1: p = 0.2; T2: p = 0.5). Overall complication rate was 6% in the UKA group versus 9.75% in TKA (p = 0.2).
Conclusion
The UKA and TKA patients had similar clinical outcomes, post-operative range of motion, and survivorship in octogenarians with medial knee osteoarthritis, with comparable complication rate. Both the surgical procedures may be considered in this patient population, but further long-term follow-up is needed.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) can represent an alternative to total knee arthroplasty (TKA) for older patients (aged 80 years and older) with medial unicompartmental osteoarthritis (OA) of the knee [10]. Following TKA, older patients may have higher rates of medical and surgical complications than younger patients (< 65 years) due to more associated comorbidities and a lower tolerance for hemodynamic alterations [30]. UKA has been proven to have less problems than TKA when carried out on carefully chosen patients to restore knee kinematics and overall function more effectively [20, 31], and it is also less expensive [34, 36]. Historically, the implementation of UKA has been diminished by concerns about mechanical loosening and the necessity for revision [25]. With implant survivability currently averaging between 95 and 98% at 3 years [24], computer-navigated and robot-assisted surgeries, together with a better implant design, may have contributed to recent improvements in the UKA results. The age of 80 years has been identified as a significant threshold at which patients deserve additional evaluation and may have a higher risk of developing adverse outcomes for surgeries including spinal fusion, total shoulder arthroplasty, and revision total hip arthroplasty [4, 5, 12, 41]. More medical comorbidities, a reduced cardiac reserve, and greater difficulties in maintaining balance are common in older patients [44, 45]. To address the constraints brought on by their knee-joint arthritic pain, patients are prone to opt for partial and whole knee-joint arthroplasty, as it allows them to live longer and keep a high level of function and independence [9, 10]. Despite these advantages, UKA has been documented in literature to have higher revision rates than TKA; however, these results are often observed in younger patients (< 65 years) who may be more active, but the results may not apply to patients aged 80 years and older with potentially lower activity levels and life expectancy [15, 17, 42]. For example, according to the Kozinn and Scott criteria, the best candidates for cemented UKA were patients older than 60 years of age who are less physically active [23]. However, literature comparing UKA with TKA in a population of patients aged 80 years and older with isolated medial compartment OA is still scarce with conflicting results [15, 17, 42]. Thus, the primary goal of this study is to compare clinical outcomes and survivorship in UKA versus those in TKA in patients with isolated medial compartment OA and who are aged 80 years and older by performing a matched pair analysis.
Materials and methods
The institutional review board approval was received to retrospectively review 90 medial UKAs consecutively performed by a single experienced surgeon. In total, 15 UKAs were excluded for the following reasons: 4 cases had previous osteotomies, 3 had rheumatoid arthritis, and 8 did not have a minimum 2-years follow-up.
The remaining 75 medial UKAs were matched with 75 TKAs performed during the same study period. Potential TKA matches used identical exclusion criteria. UKAs were age-, gender-, and body mass index-matched at a rate of 1 UKA to 1 TKA from our departmental database.
Inclusion criteria were a minimum 24-month follow-up, UKA or TKA performed by a single surgeon, and completion of follow-up evaluations.
Exclusion criteria were follow-up less than 24 months, revision surgery, rheumatoid arthritis, fixed varus deformity, previous osteotomy, or flexion deformity > 15°. Inclusion criteria for the TKA cohort were primary and traumatic isolated medial OA that met the criteria of UKA, but, for which, TKA was elected.
The primary indication was severe OA, with at least Kellgren–Lawrence grade 3 or post-traumatic arthritis only in the medial compartment [22]. In all patients, the anterior cruciate ligament and the medial and lateral collateral ligaments were functionally intact, the varus deformity was manually correctable, and there was no evidence of OA in the lateral compartment [43]. OA of the patellofemoral joint was not considered to be a contraindication, unless there was a deep eburnation or bone grooving on the medial facet of the patella (Outerbridge grade IV) [38].
All the procedures involving human participants in this study followed the ethical standards of the institutional and/or national research committee, as well as the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study followed the STROBE checklist for cohort studies [8]. Finally, informed consent was obtained from all the participants.
Surgical procedure and clinical protocol
UKA
All UKAs were performed with the same minimally invasive surgical approach and were mobile bearing using the Oxford Microplasty instrumentation (Zimmer-Biomet, Warsaw, Indiana, USA). All the patients were placed supine on a standard operating table after administering spinal anesthesia. A tourniquet was applied to the proximal thigh on the operative side and inflated to 300 mm Hg. The operative leg was placed in a thigh support, with the hip flexed to approximately 30° and the leg hanging. A midline incision was made, followed by a small medial parapatellar incision. The patella was not subluxed to avoid damage to the synovial reflections of the suprapatellar pouch. The margins of the medial tibial condyle were exposed and cleared ensuring that too much soft tissue is released. The medial meniscus was removed. Osteophytes were removed from the tibia, femur, and intercondylar notch. A routine inspection of the patellofemoral and lateral compartments was conducted to ensure that each patient had isolated medial knee OA. The anterior cruciate ligament (ACL) was also intact in all patients. First, the tibial cut was made sagittally as close to the ACL insertion as possible. However, precautions were taken not to cut the ACL fibers. The saw was placed parallel to the anatomical axis of the tibia and not tilted medially, laterally, anteriorly, or posteriorly. Then, the femoral cuts were made using the intramedullary guide [28].
TKA
The same surgeon performed all the TKAs with a standard medial parapatellar approach and without patellar eversion. Tibial resection was performed with an extramedullary guide, and distal femoral resection was performed with an intramedullary guide. All the patients received a cemented, posterior-stabilized implant (Vanguard; Zimmer-Biomet, Warsaw, IN). Intraoperatively, the patella was not resurfaced, and patelloplasty was routinely performed for all the patients, which included the removal of osteophytes, smoothing of the patellar articular surface, and denervation of the peripheral patellar using electrocautery [14].
The surgical time was defined as the time from the incision to closure. Both the patient groups followed the same rehabilitation protocol, which involved passive mobilization on the day of the surgery. On post-operative day 1, patients started active progressive mobilization of the joint and performed assisted walking with a walker or two crutches. Gradually, patients increased their weight and continued with isometric muscle toning exercises [19].
Clinical evaluation
Demographic data, including age, sex, and BMI data on the side of operation and surgical time were collected. All the clinical assessments were performed by two independent clinicians who were not involved in the index surgery. The clinical evaluation entailed the visual analog scale (VAS) [40] for pain and range of motion (ROM—flexion and extension), which was assessed using a digital inclinometer that is the most accurate method of knee-angle measurement [16]. Patient-reported outcome measurements (PROMs), including the Knee Society Score (KSS) and Oxford Knee Score (OKS) [11, 32], were measured. Each patient was clinically evaluated on the day before the surgery (T0) and at two consecutive follow-ups at least 1 year (T1) and 2 years (T2) after the surgery.
Survivorship
Revision was defined as failure of the implant (periprosthetic joint infection [PJI], periprosthetic fracture, or aseptic loosening), and survival was based on implant revision or patient death. Patient deaths were confirmed by contacting relatives. PJI was diagnosed according to the New Definition for Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society [33]. Periprosthetic fracture was defined as tibia or femur fractures occurring within 15 cm from the joint line or 5 cm from the endomedullary stem, if present [2]. Patients were classified as having aseptic loosening, if they had symptoms including pain, instability, or swelling; had radiographic evidence of loosening; and did not meet the definition for PJI [6].
Complications and adverse events
Undesirable clinical developments that were not present at baseline or that increased in severity after the treatment were classified as Adverse Events. Major complications included deep infection of implant, vascular injury, myocardial infarction, fast atrial fibrillation, stroke, pulmonary embolism, and cardiac arrest. Minor complications included superficial wound infection, acute retention of urine, deep vein thrombosis, pneumonia, and urinary tract infection [18].
Statistical analysis
An estimated sample of 130 subjects, 65 for each group, was required to compare the VAS for pain between UKA and TKA with a two-sided Wilcoxon–Mann‒Whitney test, assuming a mean difference of 3 points, a standard deviation of 1.5 for both groups, 5% alpha, and 95% power. Given the same parameters, this sample also had 99% power to detect a pre–post difference using a Wilcoxon signed-rank test, assuming a correlation of 0.30 between measurements. Additional subjects were recruited to ensure statistical significance in case of adverse events.
Summary statistics were presented as the means and standard deviation (SD) or absolute frequencies and percentages. Having tested the distribution of continuous variables, a Student’s t-test or chi-square test for categorical variables was performed to assess preoperative differences between the UKA and TKA groups. To test score differences between the groups, a Student’s t-test was used to evaluate intergroup differences at each follow-up. Second, to assess differences in time in each group for each score, a linear mixed model was performed, since it takes into account correlations among repeated measures and tests the covariance structure. Autoregressive compound symmetry, with either homogeneous or heterogeneous variances, and unstructured covariance structures were tested. The best covariance structure was evaluated for each score using the likelihood-ratio test and Akaike information criterion. Bonferroni adjustment was applied for multiple comparisons. The Cox regression model was performed using failure as an independent variable and group as a covariate. All the tests were two sided, and p < 0.05 was considered statistically significant. Statistical analyses were conducted in R version 4.1.1 [35].
Results
Demographics
The mean age at surgery was 82.1 ± 1.9 years for UKA and 81.5 ± 1.8 years for TKA (p = 0.06); there were 59 female patients (78.7%) in the UKA group and 55 (72.9%) female patients in the TKA group (p = 0.45). The TKA group had a longer follow-up time than UKA (p < 0.001). Detailed results are reported in Table 1.
Group comparison
The two groups differed in regard to surgical time (UKA: 44.9 ± 7.2 min; TKA: 54.4 ± 11.3 min; p < 0.001); furthermore, the UKA group showed better function (ROM; flexion and extension) than TKA at each follow-up time point (p < 0.05). Both the groups reported a significant improvement in all clinical scores (KSS and OKS) when compared with their preoperative status (p < 0.05), while no differences were found between the two groups at each follow-up (p > 0.05) (Table 2).
Failures and death
The UKA group reported 7 (9.3%) failures, of which one was during the first year and 6 before the 24-month follow-up point. The TKA group reported six failures, of which four were during the first year and two before the 24-months follow-up. All the deceased patients died for reasons not related to the arthroplasty, as confirmed over phone calls by relatives.
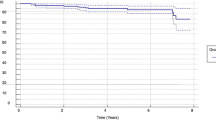
There were no survival differences between the groups (T1: p = 0.2; T2: p = 0.5). Failure details are reported in Table 3.
Complications
In total, two patients (41.5%) in the UKA group suffered from major complications and three from the control TKA group (2.25%; p = 0.7). Overall complication rate was 6% in the UKA group versus 9.75% in TKA (p = 0.2). Minor complication rates were 4.5% versus 7.5% (UKA versus TKA; p = 0.3). All complications, major and minor, are charted in Table 4.
Discussion
There have been limited studies comparing UKA and TKA in octogenarians [31, 37]. Our study found that both UKA and TKA in this patient population improved patient function as measured by PROMs, with decreased pain in both the patient cohorts and similar rates of failure, deaths, and complications.
In our study, patients who underwent UKAs showed a slightly but significantly shorter surgical time than those who underwent TKAs (UKA 45.0 ± 7.4 min; TKA 53.3 ± 10.8 min), and these findings can play a crucial role in treating older patients with systematic diseases.
Morcos et al. [27] evaluated the influence of operating time on complications and readmission within 30 days of TKA, concluding that an operating time of 90 min or more may be associated with an increase in the chances of 30-day complications and readmissions following TKA. Similarly, Cregar et al. [7] revealed a positive correlation between increased operative times and short-term post-operative complication rates after UKA. Thus, for the older patient population with increased comorbidities in this study, shorter operative time may be beneficial for outcomes and decreasing complications.
In this study, both the types of implants showed significant improvements in all the clinical scores, which is consistent with the literature where PROMs were not significantly different between UKA and TKA.
Often, elderly patients have a more sedentary lifestyle and less functional demand for knee arthroplasty than younger patients, which may reduce the risk of aseptic loosening. Although, according to the literature, TKA survivorship is greater than UKA, our data suggest that UKA may be considered an appropriate option for this patient population, since there was no difference in survivorship between the groups. This corresponds with some studies comparing UKA and TKA survivorship in patients older than 75 years. The study by Siman et al. [37] found almost no difference in 5-years survivorship estimates for UKA (98.3%) and TKA (98.8%).
Ode et al. [31] performed a retrospective control study comparing complication rates in elderly patients receiving UKA with those receiving TKA. At a mean, follow-up was 32 months for UKA and 34 months for TKA. The complication rate was significantly lower with UKA (6.7% versus 25.6%), with no early mortality. Similarly, satisfaction rates were identical: 96% and 97%. Implant survivorship was also identical.
In recent years, several articles have analyzed the outcomes of prostheses (both UKA and TKA) in patients over 80 years of age with satisfactory results, as in our study. Trigueros-Larrea et al. [42] conducted a retrospective observational study in octogenarians comparing preoperative and post-operative KSS, Knee Society Function Score (KSFS), extension and flexion, and radiologic alignment. The mean patient survival was 67.4 months. Patients ≥ 80 years achieved clinical improvement after TKA. Comorbidities, not age, were found to be the burden for surgery in older patients. Goh et al. [15] analyzed the results of UKA in the extreme elderly (≥ 80 years) by comparing the functional and perioperative outcomes between octogenarians and age-appropriate controls undergoing UKA. With the exception of poorer Short Form-12 physical scores in octogenarians at 2 years (p = 0.03), there was no difference in final post-operative scores between the groups. The rates of complications, reoperations, readmissions, and emergency room visits were also similar. The 5-years survivorship was 97% in the control group and 93% in the octogenarian group (p = 0.15).
Moore et al. [26] used a large national surgical database to examine 30-days post-operative adverse events after UKA in octogenarians compared with those in non-octogenarians. The authors found a statistically significant increase in several adverse events within 30 days of the surgery for patients aged > 80 years when compared with patients < 80 years, namely, UKA in octogenarians was associated with significantly increased odds of short-term mortality, urinary tract infection, transfusion, prolonged hospital stay, and readmission.
Recently, D’Ambrosi et al. [10] compared clinical difference and survivorship between fixed and mobile bearing in octogenarians, finding no difference in patient-reported outcome measures, ROM, implant positioning, and survivorship.
The same authors analyzed survivorship and functional results in individuals aged 80 years and over who underwent TKA with cruciate-retaining (CR) or posterior-stabilized (PS) implants. The clinical trial demonstrated that CR and PS TKA had similar clinical outcomes in octogenarians with regard to knee function, post-operative knee pain, and other complications [9].
However, our patients demonstrated some slight difference in ROM between the two groups. This finding was also observed by other studies. In the 15-year results of a prospective randomized controlled trial by Newman et al. [29], UKA achieved higher degrees of flexion than TKA, and this was maintained at the 15-years follow-up. In contrast, in our cohort, we found higher flexion at the 2-years follow-up in the TKA group (UKA 117.59 ± 3.97; TKA 119.33 ± 4.07), which may not be clinically significant.
Both the groups reported a similar number of failures throughout the follow-up period. There were no revisions in the UKA group until one year after surgery, which is comparable to the findings in the literature. A recent study by Carlson et al. [3] demonstrated that the peak of failure after Oxford UKA occurred within three years, with a second peak at seven years. Ekthiari et al. [13] reported that survivorship at 1, 5, 10, and 15 years was 97.2%, 90.5%, 83.5%, and 81.9%, respectively, for patients who underwent UKA surgery for medial knee OA. The most common mode of failure for UKA is OA progression, but it should be taken into consideration that octogenarian patients may not have a long enough life expectancy for this longer-term failure to occur [39]. In our patient population, no patients failed due to secondary OA progression within two years. Most of TKA group failures were observed within one year of follow-up; historically, studies comparing failures and revisions in TKA and UKA patients have demonstrated a trend for greater revisions in UKA patients than in TKA patients. In the study by Arirachakaran et al. [1], the rate of revision in the UKA group was 3.2 times higher than that in the TKA group. In long-term studies, TKA has established a survivorship of 92–100%. In a large retrospective database analysis comparing UKA to TKA, Kaplan‒Meier survivorship at 5 and 10 years was 98% and 95%, respectively, for TKA and 95% and 90%, respectively, for UKA. Horikawa et al. [21] reported a cumulative revision rate greater for UKA (7%) than that for TKA (4%), and Kaplan‒Meier survivorship at 10 years was 84% for UKA and 92% for TKA. It is important to note that some of these studies included all the patients undergoing UKA, and these findings may not apply to older patients.
Our study had several limitations. First, this study was conducted at a single institution and may not be applicable to other patient populations. Second, it was a retrospective study of prospectively collected data with a potential inherent selection bias. Moreover, multiplane laxity measurements were not considered in our study as part of the clinical evaluation. Finally, this study only evaluated short-term follow-up of two years, and further long-term studies are needed to assess differences between these patient cohorts.
Conclusion
UKA and TKA patients had similar clinical outcomes, post-operative range of motion, and survivorship in octogenarians with medial knee OA with a comparable complication rate. Both surgical procedures may be considered in this patient population, but further long-term follow-up is needed.
Availability of data and materials
Raw data have been submitted as supplementary material to the Journal.
References
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25:799–806
Canton G, Ratti C, Fattori R, Hoxhaj B, Murena L (2017) Periprosthetic knee fractures. A review of epidemiology, risk factors, diagnosis, management and outcome. Acta Biomed 88:118–128
Carlson SW, Lu Y, Sierra RJ (2022) Minimum 10-year survivorship of mobile-bearing unicompartmental arthroplasty: single surgeon, north American non-designer consecutive series. J Arthroplasty 37:S88–S93
Carney J, Gerlach E, Plantz MA, Cantrell C, Swiatek PR, Marx JS, Marra G (2021) Short-term outcomes after total shoulder arthroplasty in octogenarians: a matched analysis. Cureus 13:e16441
Chen M, Jia P, Feng F, Tang H (2022) A novel minimally invasive technique of inter-spinal distraction fusion surgery for single-level lumbar spinal stenosis in octogenarians: a retrospective cohort study. J Orthop Surg Res 17:100
Cherian JJ, Jauregui JJ, Banerjee S, Pierce T, Mont MA (2015) What host factors affect aseptic loosening after THA and TKA? Clin Orthop Relat Res 473:2700–2709
Cregar WM, Goodloe JB, Lu Y, Gerlinger TL (2021) Increased operative time impacts rates of short-term complications after unicompartmental knee arthroplasty. J Arthroplasty 36:488–494
Cuschieri S (2019) The STROBE guidelines. Saudi J Anaesth 13:S31–S34
D’Ambrosi R, Menon PH, Salunke A, Mariani I, Palminteri G, Basile G, Ursino N, Mangiavini L, Hantes M (2022) Octogenarians are the new sexagenarians: cruciate-retaining total knee arthroplasty is not inferior to posterior-stabilized arthroplasty in octogenarian patients. J Clin Med 11:3795
D’Ambrosi R, Valli F, Nuara A, Mariani I, Di Feo F, Ursino N, Formica M, Mangiavini L, Hantes M, Migliorini F (2023) No difference in mobile and fixed bearing partial knee arthroplasty in octogenarians: a clinical trial. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-023-03537-7. (Epub ahead of print)
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Di Matteo V, Di Pilla M, La Camera F, Morenghi E, Grappiolo G, Loppini M (2023) Perioperative complications after hip and knee revision arthroplasty in the over 80 years old population: a retrospective observational case-control study. J Clin Med 12:2186
Ekhtiari S, Bozzo A, Madden K, Winemaker MJ, Adili A, Wood TJ (2021) Unicompartmental knee arthroplasty: survivorship and risk factors for revision: a population-based cohort study with minimum 10-year follow-up. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.21.00346
Faris PM, Ritter MA, Davis KE, Priscu HM (2015) Ten-year outcome comparison of the anatomical graduated component and vanguard total knee arthroplasty systems. J Arthroplasty 30:1733–1735
Goh GS, Corvi JJ, Grace TR, Eralp I, Small I, Lonner JH (2021) Octogenarians undergoing medial unicompartmental knee arthroplasty have similar patient-reported outcomes as their younger counterparts. J Arthroplasty 36:3656–3661
Hancock GE, Hepworth T, Wembridge K (2018) Accuracy and reliability of knee goniometry methods. J Exp Orthop 5:46
Haughton DN, Wheelton AN, McLauchlan GJ (2021) Revision knee arthroplasty: Can good outcomes be achieved at lower volumes? Knee 30:63–69
Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, Lonner JH (2013) Complications of total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Relat Res 471:215–220
Henderson KG, Wallis JA, Snowdon DA (2018) Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis. Physiotherapy 104:25–35
Ho JC, Stitzlein RN, Green CJ, Stoner T, Froimson MI (2016) Return to sports activity following UKA and TKA. J Knee Surg 29:254–259
Horikawa A, Miyakoshi N, Shimada Y, Kodama H (2015) Comparison of clinical outcomes between total knee arthroplasty and unicompartmental knee arthroplasty for osteoarthritis of the knee: a retrospective analysis of preoperative and postoperative results. J Orthop Surg Res 10:168
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474(8):1886–1893
Kozinn SC, Scott RD (1988) Surgical treatment of unicompartmental degenerative arthritis of the knee. Rheum Dis Clin North Am 14:545–564
Maritan G, Franceschi G, Nardacchione R, Furlan E, Mariani I, Ursino N, D’Ambrosi R (2023) Similar survivorship at the 5-year follow-up comparing robotic-assisted and conventional lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 31:1063–1071
Mittal A, Meshram P, Kim WH, Kim TK (2020) Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol 21:15
Moore HG, Schneble CA, Kahan JB, Grauer JN, Rubin LE (2022) Unicompartmental knee arthroplasty in octogenarians: a national database analysis including over 700 octogenarians. Arthroplast Today 15:55–60
Morcos MW, Nowak L, Schemitsch E (2021) Prolonged surgical time increases the odds of complications following total knee arthroplasty. Can J Surg 64:E273–E279
Murray DW, Parkinson RW (2018) Usage of unicompartmental knee arthroplasty. Bone Joint J 100-B:432–435
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br 91:52–57
O’Neill CN, Gowd AK, Waterman BR, Kates SL, Patel NK (2022) Significant reduction in short-term complications following unicompartmental versus total knee arthroplasty: a propensity score matched analysis. J Arthroplasty 37:2014–2019
Ode Q, Gaillard R, Batailler C, Herry Y, Neyret P, Servien E, Lustig S (2018) Fewer complications after UKA than TKA in patients over 85 years of age: a case-control study. Orthop Traumatol Surg Res 104:955–959
Odum SM, Fehring TK, Knee Society Crosswalk Writing Group (2017) Can original knee society scores be used to estimate new 2011 knee society scores? Clin Orthop Relat Res 475:160–167
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992–2994
Peersman G, Jak W, Vandenlangenbergh T, Jans C, Cartier P, Fennema P (2014) Cost-effectiveness of unicondylar versus total knee arthroplasty: a Markov model analysis. Knee 21:S37-42
R Core Team (2017) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Shankar S, Tetreault MW, Jegier BJ, Andersson GB, Della Valle CJ (2016) A cost comparison of unicompartmental and total knee arthroplasty. Knee 23:1016–1019
Siman H, Kamath AF, Carrillo N, Harmsen WS, Pagnano MW, Sierra RJ (2017) Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: comparable reoperation, revision, and complication rates. J Arthroplasty 32:1792–1797
Slattery C, Kweon CY (2018) Classifications in brief: outerbridge classification of chondral lesions. Clin Orthop Relat Res 476:2101–2104
Tay ML, McGlashan SR, Monk AP, Young SW (2022) Revision indications for medial unicompartmental knee arthroplasty: a systematic review. Arch Orthop Trauma Surg 142:301–314
Thong ISK, Jensen MP, Miró J, Tan G (2018) The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain 18:99–107
Toro G, Bothorel H, Saffarini M, Jacquot L, Chouteau J, Rollier JC (2019) Uncemented total hip arthroplasty in octogenarian and nonagenarian patients. Eur J Orthop Surg Traumatol 29:103–110
Trigueros-Larrea JM, Gonzalez-Bedia MA, Lomo-Garrote JM, Martin-de la Cal O, Martin-Ferrero MA (2021) Total knee arthroplasty in octogenarians: should we still be so restrictive? Geriatrics (Basel) 6:67
Tyagi V, Farooq M (2017) Unicompartmental Knee Arthroplasty: Indications, Outcomes, and Complications. Conn Med 81:87–90
Varghese PP, Chen C, Gordon AM, Magruder ML, Vakharia RM, Erez O, Razi AE (2022) Complications, readmission rates, and in-hospital lengths-of-stay in octogenarian vs. non-octogenarians following total knee arthroplasty: an analysis of over 1.7 million patients. Knee 35:213–219
Yohe N, Weisberg MD, Ciminero M, Mannino A, Erez O, Saleh A (2020) Complications and readmissions after total hip replacement in octogenarians and nonagenarians. Geriatr Orthop Surg Rehabil 11:2151459320940959
Acknowledgements
This study was supported and funded by the Italian Ministry of Health – “Ricerca Corrente”
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. None.
Author information
Authors and Affiliations
Contributions
All authors contributed equally.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Permission for the study was obtained from the local ethical committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
All authors consent to the publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
D’Ambrosi, R., Ursino, C., Mariani, I. et al. Clinical outcomes, complications, and survivorship for unicompartmental knee arthroplasty versus total knee arthroplasty in patients aged 80 years and older with isolated medial knee osteoarthritis: a matched cohort analysis. Arch Orthop Trauma Surg 143, 6371–6379 (2023). https://doi.org/10.1007/s00402-023-04916-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04916-9