Abstract
Introduction
The prime requisites of a good digital arthrodesis are a painless and stable union in a proper position. Arthrodesis of the distal interphalangeal joint of the fingers is not without potential complications including nonunion, malunion, and deep tissue infections. The Shark Screw® is a human, cortical bone allograft for osteosynthesis and an alternative to metal or bioabsorbable devices in orthopedics and trauma surgery. The primary hypothesis is that the fusion and complication rate, using the Shark Screw®, is at least similar to those reported in the literature, using metal or bioabsorbable screws.
Material and methods
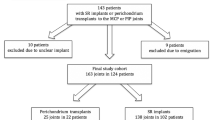
This retrospective cohort study analyzes the fusion and complication rate and the patient satisfaction of distal interphalangeal joint arthrodesis of 27 fingers with the human allogeneic cortical bone screw. Complications, Disabilities of Arm, Shoulder, and Hand Questionnaire (Quick-DASH) score and Michigan Hand Outcomes Questionnaire (MHQ) score, grip and pinch strength and fusion angle were investigated.
Results
The mean follow-up was 23 months. At 6 weeks after surgery, fusion was obtained for all fingers. There was no surgical complication that required revision surgery. An average fusion angle of 13.6° ± 10.7° was measured. VAS pain score decreased significantly from 6.9 before surgery to 0.14 after surgery. The Quick-DASH score decreased from 10.7 to 7.8. The MHQ score improved in all sub-scores.
Conclusion
The complication rates, using the Shark Screw® for DIP joint arthrodesis, are lower compared to the results reported in the literature for other surgical techniques. Complications related to the human allograft cortical bone screw itself were not observed. The bone screw is completely remodeled into the host bone and further hardware removal is not necessary.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal interphalangeal (DIP) joint arthrodesis is usually performed to relieve pain, correct deformity, or stabilize a dysfunctional joint. Causes for such symptoms include acute traumatic or post-traumatic condition, osteoarthritis, and rheumatoid arthritis [1].
The Shark Screw® is a human cortical bone allograft for the fixation of fractures, osteotomies, and arthrodesis. It is an alternative to metal or bioabsorbable devices in orthopedics and trauma surgery [2,3,4,5]. The safety of human allogeneic, sterilized bone transplants regarding disease transmission, biological tolerance, potential graft rejection, and allo-sensitization is well known, since allogeneic bone transplants (e.g., bone chips, bone blocks) are widely used in regenerative, maxillofacial and orthopedic surgery [6,7,8,9]. Besides the fixation function, due to its design as a set screw, the Shark Screw® exhibits osteoconductive properties promoting the ingrowth of blood vessels and bone cells [2, 8, 10]. The bone material, the human allogeneic cortical bone screw consists off, is completely remodeled into the patients bone. There is no need of hardware removal.
Flexion of the finger is important for the grip and pinch strength achieved after surgery [11]. A stable and pain-free DIPJ is necessary to guarantee the important functions of the finger.
There is insufficient evidence to support any particular technique [12, 13]. In most cases, successful fusion of the DIPJ improves the function and appearance of the digit with acceptable morbidity [13, 15]. Non-fusion-rate was 11% in patients with advanced osteoarthritis [16] and 15–0% in patients treated with K-wires [13]. DIPJ arthrodesis of the fingers is not without potential complications including nonunion, malunion, and deep tissue infections [18], chronic regional pain syndrome, and hypersensitivity. Stern et al. [19] evaluated the complications of different surgical techniques (crossed Kirschner pins, interfragmentary wire, longitudinal Kirschner pin and Herbert screw) and described 20% major complications and 16% minor complications [19].
The primary hypothesis of this retrospective study of DIPJ arthrodesis of 27 fingers in 21 patients is that the fusion rate, using the Shark Screw®, is at least similar to fusion rates reported in the literature achieved with metal or bioabsorbable screws. The secondary hypothesis is that the complication rate is not higher compared to other techniques. The advantage of complete bone integration without any hardware remnants will be shown.
Patients and methods
Patient data
For this study, a positive ethic vote was received (EK21-150-VK). 27 fingers in 21 patients with degenerative arthrosis were identified and included. Primary osteoarthrosis was the only indication for inclusion and other indications were exclusion criteria. The index finger was operated in 13 cases, the middle in 7, the ring finger in 3, and the small finger in 4 cases.
The primary outcome was the union rate, which was defined by the first author using common radiological criteria (signs of osseus union in the X-ray) and by a pain-free pinch grip 6 weeks after surgery. Fusion angles were measured on lateral radiographs. Age, profession, sex, dominant hand, operated hand, follow-up time, VAS pain score, Quick-DASH and MHQ score (pre-/post-surgery), grip and pinch strength for the operated and untreated hand, and patient satisfaction (1 = not satisfied, 2 = partly satisfied, 3 = satisfied, 4 = totally satisfied) were recorded. Grip strength and pinch strength were measured using the Jamar hand and finger dynamometer (Jamar, Hydraulic pinch gauge 52603, SEAHAN, Republic of Korea). In detail, to measure the crush grip strength, the hand dynamometer (Jamar, Hydraulic hand dynamometer SH5001) was used. For all subjects, the hand dynamometer was set at the hand hold level 2 out of 5. The patient had to sit in a stable position holding the forearm horizontal, the elbow flexed at 90°, and the wrist in a neutral position. First, the pinch grip strength was measured by squeezing the operated finger against the thumb with the finger dynamometer plates in between. The patients were instructed to apply their maximum strength for at least 3 s. The measured value of three repeating cycles of the finger with the fused DIP joint including the finger of the opposite hand was recorded. The patients had a 1 min break between each measurement. After a 5 min break, the crush grip strength was measured in the same way applying full power by clenching the hand into a fist while holding the hand dynamometer. Out of three repeated cycles, an average value was calculated for the operated and opposite fingers and hands.
Surgical procedure
The surgical procedure was done under local anesthesia and using a finger tourniquet. An H-shaped skin incision on the dorsal side of the DIP joint was made. Subsequently, the tendon was cut longitudinally to expose the joint. Osteophytes were removed with a rongeur. Then any cartilage from the proximal and distal joint surfaces was removed and the 1.2 mm K-wire was used to achieve the desired fusion angle of the DIP joint under fluoroscopic guidance. Concerning the fusion angle, pinch grip finger function and cosmetic aspects were considered. After that, a small skin incision at the tip of the finger was performed, where a drill was introduced. Guided by the K-wire, the appropriate drill hole and the thread of a diameter of 3mm was done. Then the thread cutter and K-wire were removed. After lavage of the drill hole with NaCl solution, the Shark-Screw® (3.5 mm diameter and 35 mm length, Surgebright GmbH, Lichtenberg, Austria) was introduced (Figs. 1 and 2). This screw dimensions were sufficient for all DIP joints in all patients treated with this technique. Joint position and placement of the screw were checked again with the image intensifier. After that, the head of the screw was shortened to bone level. Tendons were adapted again with two resorbable sutures and the skin was closed with non-resorbable single stitch sutures (Fig. 3). After surgery, a thin finger bandage and a custom-made finger sleeve was applied for 6 weeks.
Postsurgical rehabilitation
The bandage was changed 2 weeks after surgery, and stitches removed. The same plastic finger sleeve was tightened up and used for the next 4 weeks. 6 weeks after surgery, an X-ray was taken, the finger sleeve was removed, and the patient was allowed to use his finger in daily life. The patient had three to five visits at our occupational therapists within the postoperative period of 6 weeks after removal of the stitches focusing on skin and scar care and mobilizing the neighbor joints.
Statistics
Statistics were calculated with the program Origin Pro (OriginPro, Version 2022. OriginLab Corporation, Northampton, MA, USA). Because of non-normal distribution (analyzed with Kolmogorov–Smirnov test) for most of the data, Kruskal–Wallis–ANOVA was used for calculating statistically significant differences. Because there is only one study arm and all patients showed osseous union on the final X-ray, there was no power calculation to observe significant differences for unions. For VAS, Quick-DASH, and MHQ score before and after surgery, power was calculated and only when a power of > 0.8 was observed, significant differences were shown. Statistical significance was considered at a p value of < 0.05.
Results
Patient demographics are described in Table 1.
Mean follow-up was 23 ± 9 months (Table 2). In two patients, minor complications were observed: one had a prolonged swelling and redness of the scar, and the other patient was cosmetically unsatisfied with the obtained fusion angle. A reduced fist clench with a fingertip hollow hand (FKHH) distance of more than 2 cm due to degenerative joint problems of the neighbor joints of the involved finger was recorded in two patients. Major complications like fractures of the implant or bone, pseudoarthrosis, superficial or deep infections, or skin problems were not observed in our cohort. Patient satisfaction was high (3.9, 4 = totally satisfied). All patients would repeat the surgery (Table 2).
Radiographs were performed before surgery (Fig. 4A), 6 weeks (Fig. 4B), and at least 6 months after surgery (Fig. 4C). Fluoroscopy was only performed during surgery.
Concerning the fusion angle, we informed the patients that a flexion angle between 10° (index finger) and 40° (little finger, [12, 13]) in the fused DIP joint is necessary to obtain the best pinch grip strength, but the final decision about the fusion angle was with the patient as described by other studies [13]. Factors like preoperative axis of the DIP joint, bone defects, or inaccuracy regarding the drilling and fixation with the screw implant led to deviations of the strived fusion angle. The obtained fusion angle was on average 13.6° ± 10.7°. VAS and MHQ values were statistically significantly improved after surgery (Table 3).
Grip strength of the operated hand and pinch grip strength of the operated finger were similar to the non-treated hand or fingers of the contralateral side (Table 4). Grip strength of male and female patients differed, but did not reach statistical significance.
Discussion
The most important finding of this study was that fusion was achieved in all 27 fingers of 21 patients after 6 weeks using the human, allogeneic cortical bone screw. In DIP arthrodesis, others report time to fusion between 8 and 11 weeks, using headless compression screws [15, 20, 21], reverse fix nails [22], and nitinol intramedullary fixation implants.[18]. Fusion was reported between 82 and 96% [12,13,14,15,16,17,18, 20, 22,23,24,25,26] for different fusion techniques. Stern et al. concluded that inadequate bone stock, inadequate bone resection, premature pin or screw removal, and infection had severe influence on bony healing and thus on the fusion [19]. They further state that no single technique has gained universal popularity for small-joint arthrodesis, and the arthrodesis technique did not determine whether union occurred [19]. The use of the human allogeneic cortical bone screws for arthrodesis can provide biological bridging of the arthrodesisgap, a stable fixation of the fused joint and must not be removed in case of septic complications [5]. Since the Shark Screw® is a set screw with a thread pitch of 0.6 mm, it is absolutely rotation stable. The thread design complies with the biomechanical and physical laws of a set screw, where rotational stability is mandatory. In our study, all arthrodesis were fused after 6 weeks.
The mean follow-up was nearly 2 years and was described between 10 month and 3 years by others [22, 23, 25, 27].
There were no infections, bone healing problems, Shark Screw® failure during or after surgery, and revision surgery in our patient cohort. Others report an infection rate of 4.5% [28] or 7% [15] and hardware failures and hardware removal [12].
In our study, the mean postoperative fusion angle of all DIP joints was 13.6° ± 10.7°. Auzias et al. published an average fusion angle measured on lateral X-rays of 9.3° (3°–19°) [17], which is similar to our findings. Furthermore, they described that in fingers with a 10° offset implant, the postoperative fusion angle was 10.7°(0–19°) and it was 5.6° (3°–11°) with straight implants [17]. In our study, except for one patient, all others obtained the planed and preferred fusion angle depending on functional and esthetic considerations (Table 2).
Grip strength of the dominant hand was for men 40–47 kg and for women 25–28 kg depending on the age group [29, 30]. Grip strength of the operated hand in our study was on average 29 kg and was similar to that in other reports.[29,30,31]. Gugger et al. [32] reported a grip strength of 21.2 kg post-surgery, which equals 69% of the untreated side. Liu et al. reported also a lower grip strength, 26.4 kg, post-surgery [33]. A grip strength of 91–96% of the untreated side is supported by others [11, 31]. In our patient cohort, the grip strength was 96% of the untreated side and not related to the fusion angle. Song et al. described a pinch power of 75% of the untreated side [21], while we obtained a pinch power between 87 and 100% of the untreated side. A pinch strength of 5.5 kg was reported for the index finger by Liu et al. [33] and was higher than the one we recorded for the untreated hand (4.5 kg).
There is a potential risk to penetrate or burst the cortical bone of the distal phalanx with a screw of a bigger diameter than the phalanx, especially in little or very small fingers. Due to the fact that the Shark Screw® consists of human cortical bone, small bone defects or cracks of the cortical bone will be bridged with the screw itself and biological healing would not be disturbed. Extensive shortening of the finger, as described for other techniques [13], can be prevented in cases of reduced bone contact in the arthrodesis gap, because the cortical bone screw ensures a stable structure which supports further bone healing to obtain a solid arthrodesis. These might be unique advantages of the human, allogeneic cortical bone screw and could reduce the risk of incomplete bone healing in such cases.
Our patient cohort was older than described in most other studies [17, 18, 22,23,24,25,26,27], and as reported more female than male patients were treated [24, 27]. The pre- and postoperative VAS and MHQ improved as described elsewhere [16,17,18, 23, 25, 27, 33]. Additionally, there was a trend to better Quick-DASH post-surgery. Patient satisfaction is generally high after this procedure and was 3.9 in our analyses and 4 ± 1 in the study of Trumble et al. [34].
No attention to allergies, such as nickel [25], has to be given, when using the human, allogeneic cortical bone screw. This avoids a particle-induced aseptic implant loosening [25]. No inflammatory infiltrates were observed 10 weeks after implantation of the cortical bone screw for treating a hallux rigidus [10].
Strength of the study
The strength of the study is that no pseudarthrosis was recorded in all evaluated patients, regardless of the finger treated and the indication of the surgery. Cases with insufficient bone stock due to defects or incomplete adaptation of the arthrodesis gap seem to benefit from the biological properties of the screw itself concerning bony consolidation. In the interest of the patient, clinical practice should change to this new technique, resulting in normal bone after arthrodesis.
Limitations of the study
Limitations of the study such as a small number of patients and a single surgeon treatment are evident. Another limitation is that there is just one study arm and no control group.
In conclusion, the human, allogeneic cortical bone screw (Shark Screw®) offers an option for DIPJ arthrodesis. Complication rates seems to be lower, compared to conventional metallic or biodegradable magnesium implants because implant-associated side effects could be completely avoided. 6 weeks post-surgery, all patients of our series had complete fusion of the DIP joint. The bone screw transforms into original bone starting at the moment of implantation and is completely remodeled within 6–12 months. A unique advantage of the Shark Screw® seems to be the fact that bone defects of the cortical bone or reduced adaptation of the fusion site can be bridged with the screw. They heal stably without consequences by transforming into the host bone structure. The introduced bone screw works like a biological guiding structure and supports the bone healing by itself. Further investigations concerning the defect size, which can be bridged with the Shark Screw®, to get stable biological bone healing, have to be done. Another benefit is that the bone healing itself is not affected by the implant, and thus no complications are expected related to the implant und further hardware removal is avoided. All these advantages could potentially decrease the cost for the social security system.
Data availability
All data recorded are presented in the manuscript. Additional information can be obtained from the corresponding author on request.
References
Heinonen A, Leppänen O, Huhtala H, Karjalainen T, Jokihaara J (2020) Factors influencing bone union in finger distal interphalangeal and thumb interphalangeal joint arthrodesis. J Hand Surg Asian Pac 25:184–191. https://doi.org/10.1142/s2424835520500216
Pastl K, Schimetta W (2021) The application of an allogeneic bone screw for osteosynthesis in hand and foot surgery: a case series. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03880-6
Amann P, Bock P (2022) Clinical and radiological results after use of a human bone graft (Shark Screw®) in TMT II/+II arthrodesis. Foot Ankle Orthop. https://doi.org/10.1177/2473011421s00077
Huber T, Hofstätter SG, Fiala R, Hartenbach F, Breuer R, Rath B (2022) The application of an allogenic bone screw for stabilization of a modified chevron osteotomy: a prospective analysis. J Clin Med 11:1384
Hanslik-Schnabel B, Flöry D, Borchert GH, Schanda JE (2022) Clinical and radiologic outcome of first metatarsophalangeal joint arthrodesis using a human allogeneic cortical bone screw. Foot Ankle Orthopaedics 7:24730114221112944. https://doi.org/10.1177/24730114221112944
Pruss A, Perka C, Degenhardt P, Maronna U, Büttner-Janz K, Paul B, Müller K, Klumpp C, Bruck JC, Von Versen R (2002) Clinical efficacy and compatibility of allogeneic avital tissue transplants sterilized with a peracetic acid/ethanol mixture. Cell Tissue Bank 3:235–243. https://doi.org/10.1023/a:1024697515420
Gomes KU, Carlini JL, Biron C, Rapoport A, Dedivitis RA (2008) Use of allogeneic bone graft in maxillary reconstruction for installation of dental implants. J Oral Maxillofac Surg 66:2335–2338. https://doi.org/10.1016/j.joms.2008.06.006
Greenwald AS, Boden SD, Goldberg VM, Khan Y, Laurencin CT, Rosier RN (2001) Bone-graft substitutes: facts, fictions, and applications. J Bone Joint Surg Am 83:98–103. https://doi.org/10.2106/00004623-200100022-00007
Delloye C, Cornu O, Druez V, Barbier O (2007) Bone allografts: what they can offer and what they cannot. J Bone Jt Surg 89:574–579. https://doi.org/10.1302/0301-620x.89b5.19039
Brcic I, Pastl K, Plank H, Igrec J, Schanda JE, Pastl E, Werner M (2021) Incorporation of an allogenic cortical bone graft following arthrodesis of the first metatarsophalangeal joint in a patient with Hallux Rigidus. Life (Basel). https://doi.org/10.3390/life11060473
Beecher SM, O’Briain DE, Ng JP, Murphy E, O’Sullivan ME (2017) Arthrodesis of little finger distal interphalangeal joint in flexion to regain sporting ability. J Hand Surg Asian Pac 22:83–87. https://doi.org/10.1142/s0218810417500149
Dickson DR, Mehta SS, Nuttall D, Ng CY (2014) A systematic review of distal interphalangeal joint arthrodesis. J Hand Microsurg 6:74–84. https://doi.org/10.1007/s12593-014-0163-1
Vonderlind HC, Eisenschenk A, Strüwer J, Millrose M (2021) Die Arthrodese des Fingerendgelenkes: eine Literaturanalyse. Handchir Mikrochir Plast Chir 54:5–20. https://doi.org/10.1055/a-1560-2677
Millrose M, Gesslein M, Ittermann T, Kim S, Vonderlind HC, Ruettermann M (2022) Arthrodesis of the proximal interphalangeal joint of the finger—a systematic review. EFORT Open Rev 7:49–58. https://doi.org/10.1530/eor-21-0102
Brutus JP, Palmer AK, Mosher JF, Harley BJ, Loftus JB (2006) Use of a headless compressive screw for distal interphalangeal joint arthrodesis in digits: clinical outcome and review of complications. J Hand Surg Am 31:85–89. https://doi.org/10.1016/j.jhsa.2005.09.009
De Almeida YK, Athlani L, Dap F, Dautel G (2019) Distal interphalangeal joint arthrodesis using the X-Fuse(®) implant: a retrospective study of 54 fingers with 24 months’ follow-up. Hand Surg Rehabil 38:186–190. https://doi.org/10.1016/j.hansur.2019.01.001
Auzias P, Delarue R, Strouk G, Guerre E, Limousin M, Fontaine C, Aumar A (2019) Distal interphalangeal joint arthrodesis with the intramedullary Lync(®) implant: prospective study of 22 cases. Hand Surg Rehabil 38:114–120. https://doi.org/10.1016/j.hansur.2019.01.004
Seitz WH Jr, Marbella ME (2013) Distal interphalangeal joint arthrodesis using nitinol intramedullary fixation implants: X-fuse implants for DIP arthrodesis. Tech Hand Up Extrem Surg 17:169–172. https://doi.org/10.1097/BTH.0b013e31829ba688
Stern PJ, Fulton DB (1992) Distal interphalangeal joint arthrodesis: an analysis of complications. J Hand Surg Am 17:1139–1145. https://doi.org/10.1016/s0363-5023(09)91081-4
Iwamoto T, Matsumura N, Sato K, Momohara S, Toyama Y, Nakamura T (2013) An obliquely placed headless compression screw for distal interphalangeal joint arthrodesis. J Hand Surg Am 38:2360–2364. https://doi.org/10.1016/j.jhsa.2013.09.026
Song JH, Lee JY, Chung YG, Park IJ (2012) Distal interphalangeal joint arthrodesis with a headless compression screw: morphometric and functional analyses. Arch Orthop Trauma Surg 132:663–669. https://doi.org/10.1007/s00402-011-1413-3
Matsumoto T, Nakamura I, Miura A, Momoyama G, Ito K (2013) Distal interphalangeal joint arthrodesis with the reverse fix nail. J Hand Surg Am 38:1301–1306. https://doi.org/10.1016/j.jhsa.2013.01.017
Ameline T, Bégot V, Ardouin L, Hulet C, Hanouz N (2015) Arthrodesis of thumb interphalangeal and finger distal interphalangeal joints using the intramedullary X-Fuse(®) implant: retrospective analysis of 38 cases. Chir Main 34:67–72. https://doi.org/10.1016/j.main.2015.01.002
Kocak E, Carruthers KH, Kobus RJ (2011) Distal interphalangeal joint arthrodesis with the Herbert headless compression screw: outcomes and complications in 64 consecutively treated joints. Hand (N Y) 6:56–59. https://doi.org/10.1007/s11552-010-9295-3
Jakubek M, Enzendorfer M, Fiala R, Trieb K (2017) Interphalangeal arthrodesis using an intramedullary nitinol implant: a prospective study. Eklem Hastalik Cerrahisi 28:87–91. https://doi.org/10.5606/ehc.2017.52924
Spies CK, Hohendorff B, Löw S, Müller LP, Oppermann J, Hahn P, Unglaub F (2017) Arthrodesis of the distal interphalangeal joint using the headless compression screw. Oper Orthop Traumatol 29:374–384. https://doi.org/10.1007/s00064-017-0507-7
Villani F, Uribe-Echevarria B, Vaienti L (2012) Distal interphalangeal joint arthrodesis for degenerative osteoarthritis with compression screw: results in 102 digits. J Hand Surg Am 37:1330–1334. https://doi.org/10.1016/j.jhsa.2012.02.048
Fulton D, Balazy M, McGiff JC, Quilley J (1996) Possible contribution of platelet cyclooxygenase to the renal vascular action of 5,6-epoxyeicosatrienoic acid. J Pharmacol Exp Ther 277:1195–1199
Kodama R, Muraki S, Oka H, Iidaka T, Teraguchi M, Kagotani R, Asai Y, Yoshida M, Morizaki Y, Tanaka S et al (2016) Prevalence of hand osteoarthritis and its relationship to hand pain and grip strength in Japan: the third survey of the ROAD study. Mod Rheumatol 26:767–773. https://doi.org/10.3109/14397595.2015.1130673
Melamed E, Polatsch DB, Beldner S, Melone CP Jr (2014) Simulated distal interphalangeal joint fusion of the index and middle fingers in 0° and 20° of flexion: a comparison of grip strength and dexterity. J Hand Surg Am 39:1986–1991. https://doi.org/10.1016/j.jhsa.2014.06.021
Mühldorfer M, Hohendorff B, Prommersberger KJ, van Schoonhoven J (2009) Medium-term results after radioscapholunate fusion for post-traumatic osteoarthritis of the wrist. Handchir Mikrochir Plast Chir 41:148–155. https://doi.org/10.1055/s-0029-1202841
Gugger Y, Mühldorfer M, Prommersberger KJ, van Schoonhoven J (2015) Stabilization of the distal radioulnar joint according to Adams: clinical, and radiological results. Handchir Mikrochir Plast Chir 47:297–303. https://doi.org/10.1055/s-0035-1559721
Liu YJ, Ding XH, Ji X, Jiao HS, Ren SQ, Zhang HX (2021) Y-Shaped tendon graft-a technique in the reconstruction of posttraumatic chronic boutonniere deformity. J Hand Surg Am 46(712):e711-712.e716. https://doi.org/10.1016/j.jhsa.2021.01.003
Trumble TE, Heaton DJ (2017) Outcomes of surface replacement proximal interphalangeal joint arthroplasty through a volar approach: a prospective study. Hand (NY) 12:290–296. https://doi.org/10.1177/1558944716662020
Funding
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
CK designed the study and performed the surgery; CK, CR, RP, DS, and CA processed the data; GHB did the statistics and wrote the manuscript; all authors revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krasny, C., Radda, C., Polke, R. et al. A human, allogeneic cortical bone screw for distal interphalangeal joint (DIP) arthrodesis: a retrospective cohort study with at least 10 months follow-up. Arch Orthop Trauma Surg 143, 4557–4564 (2023). https://doi.org/10.1007/s00402-023-04785-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04785-2