Abstract
Background
Glenoid defects can be addressed traditionally by asymmetric reaming or by bone-preserving correction to a more lateral joint line by bone or metal augmented baseplates in reverse shoulder arthroplasties. While there is more evidence in literature regarding the outcome and complications of Bony Increased Offset Reversed Shoulder Arthroplasty (BIO-RSA), there is minimal reported experience with the outcome after metal glenoid augments. The aim of this study was to determine whether a metal augment can correct the glenoid deformity in an anatomic manner.
Methods
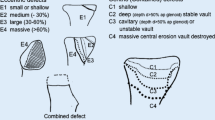
Glenoid morphology and deformity were determined in 50 patients with Walch type B1, B2, D and Favard type E0–E3 glenoid defects using preoperative radiographic and computed tomography (CT) analysis. All patients received a preoperative planning CT with 3D planning, and measurements of glenoid inclination (in 3 planes proximal, middle, distal), reversed shoulder arthroplasty angle (RSA) and glenoid version were obtained. All patients had a pathologic inclination in the coronal or frontal planes of > 10°. Above the threshold of 10° pathological glenoid version or inclination metal hemi-augments of 10°, 20°, or 30° were used which allow an individual 360° augment positioning according to the patient glenoid deformity.
Results
The mean preoperative numbers of the glenoid version demonstrate that most glenoids were in retroversion and superior inclination. In total 2410° wedges, 1820° wedges and 8 30° wedges were used. In the majority of cases, the wedge was positioned posteriorly and/or cranially between 10:00 and 12:00 o’clock, which allows a correction in a 3D manner of the glenoid inclination and version. The mean RSA angle could be corrected from 22.76 ± 6.06 to 0.19° ± 2.7 (p < 0.0001). The highest retroversion of the glenoid is evidenced in the proximal section and it could be corrected from − 23.32° ± 4.56 to − 6.74° ± 7.75 (p < 0.0001) and in the middle section from − 18.93° ± 3.35 to − 7.66° ± 5.28 (p < 0.0001). A mean sphere bone overhang distance (SBOD) of 5.70 ± 2.04 mm was found in order to avoid or minimize relevant scapular notching.
Conclusion
By using a new 360° metal-augmented baseplate, the preoperative pathological inclination and retroversion can be corrected without medialization of the joint line. Future clinical results will show whether this bone-preserving procedure improves also the clinical outcomes as compared to asymmetric medialized reaming or wedged BIO-RSA.
Level of evidence
Level IV, Case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glenoid defects and glenoid dysplasia can be addressed and corrected by bone or metal augmentation, in order to achieve an effective and accurate lateral and distal prosthetic center of rotation in reversed shoulder arthroplasty. Patients with rotator cuff arthropathy, rheumatoid arthritis of the shoulder, and revision surgery of an anatomic or RSA represent a possibility to preserve shoulder joint function despite missing of rotator cuff [1, 2].
To overcome the weakness or lack of rotator cuff muscles, Grammont stated two important biomechanical principles: (1) medialization of the center of rotation and (2) lowering the humerus [1, 2]. These principles increased the tension on the deltoid muscle, which improves the mechanical advantage on the shoulder elevation, and at the same time reducing the torque on the glenoid component.
An important aspect to be considered is that glenoid defects affect the center of rotation of the shoulder, since the implantation of the baseplate could ream a large amount of bone and therefore the center of rotation could be medialized. In bone defects such as Walch type B or C glenoid, a asymmetric reaming with medialized center of rotation and results in more bone loss but stable sitting of a standard baseplate. This technique has proven to be an alternative without correction of deformity can also lead to good midterm results as shown by Mc Farland et al. However, the detailed amount of deformity corrections remained unclear and some violation of subchondral bone may occur [3].
On the other hand, studies have shown that medialization of the center of rotation may result in multiple complications, for instance, scapula notching, reduced internal rotation due to anterior impingement, reduced abduction due to acromial impingement, and prothesis dislocation due to decreased soft-tissue tension [4]. In this context the use of metallic hemi-wedges may prevent a medialized joint line and results in a lateralized baseplate and sphere position [5].
To avoid or to compensate such risks, glenoid augmentation can be achieved with bone or metal augmentation [6,7,8,9,10]. By both methods, a more lateralized center of rotation of the reverse prosthesis can be achieved as well as a bone preservation on the high side of the deformity. The low side of the deformity can be augmented by the wedged baseplate or the wedged bone block to allow a deformity correction in an anatomical manner.
While there is more evidence the literature regarding the degree of deformity correction, outcomes and complications of wedged BIO-RSA, there is minimal evidence reported with the deformity correction and outcome after trabecular metal augment.
The aim of this study was to determine whether a metal augment can correct the deformity towards an anatomic manner. A threshold of 10 degree of pathological glenoid version or inclination was defined to correct the deformity. Hemi-wedge glenoid base plates of 10°, 20° or 30° augments were used, which can be implanted and positioned 360° freely with regard to the orientation of the wedge depending on the deformity.
Material and methods
Study design and patient selection
A retrospective review of prospectively collected data was performed in 50 patients that had undergone primary RSA by the first authors (T.G., J.W. and L.N) between August 2020 and July 2022 at our institution (Orthopädische Klinik Paulinenhilfe Stuttgart) with a metal augmented base plate (Comprehensive Reverse Shoulder System Augmented Baseplate; Zimmer Biomet; Warsaw, Indiana, USA).
The following inclusion criteria were used: (1) all adults with skeletal maturity; exceeding a threshold of pathologic angular dimension of inclination in the coronal planes of > 10° (2) and version in the axial planes of > 10° (3) all RSA with a metal augmented baseplate (4) primary osteoarthritis and consented to be included in the study. Patients with pre-operative acquired or congenital acromial abnormalities such as os acromiale or stress fractures were excluded from this study.
Glenoid morphology and deformity were determined in all patients using preoperative radiographic and CT scan analysis of the affected shoulder and entire scapula, in order to classify the glenoid morphology according to the Walch [11] and Favard [12] classification. All patients received preoperative planning, CT scan (0.5-mm slices) with 3D planning (Signature One Planner; Zimmer Biomet; Warsaw, Indiana, USA).
Shoulder radiograph and CT scan were obtained for all patients at final follow-up and determined the postoperative achieved glenoid inclination (°; β angle) [13], RSA angle [12] and version (°; distal, middle, and proximal) [14]; in addition, Acromio-Humeral (AH) distance (mm), scapulo-humeral index (SCI; %) [15], were also determined. The sphere bone overhang distance (SBOD, mm)[16] was measured to estimate the scapular notching, which was rated on the anteroposterior scapular radiograph according to the system of Sirveaux et al. [17]. Radiographic studies were evaluated by two independent reviewers (experienced orthopedic surgeons), and the data were analyzed by calculating intraclass correlation coefficients (ICCs). We found excellent agreement between the two observers (ICC 0.98).
The ethics commission (Ethikkommission der Landesaerztekammer Baden-Wuerttemberg Germany, F-2022-005) approved all procedures, and the study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008 [18].
Surgical technique
All surgeries were performed using the Comprehensive Reverse Shoulder System (Zimmer Biomet; Warsaw, Indiana, USA). The procedure was carried out under general anesthesia with an interscalene catheter block in beach chair position. A standard deltopectoral approach was performed, with detachment of any remaining sub-scapularis and tenodesis of the long head of biceps. First, the asymmetric high side of the glenoid was reamed with a 25 mm reamer (approximately 50% of the glenoid surface) followed by a half-open second reamer of the lower sitting 50% of the bone deficient glenoid. A metal augmented glenoid base plate with a hemi-wedge of 10°, 20° or 30° was used. All base plates were placed with the maximum hemi-wedge in the zone of greatest defect, according to our preoperative planning. The sphere asymmetric guide allows for optimal offset sitting of the a 36 or 41 mm sphere at a desired offset of at least 4 mm caudal glenoid overhang. To ensure that the deltoid was appropriately tensioned and the implant was properly positioned, we (1) looked for stable prosthesis position (two fingers allowed between inlay and humeral tray) during application of axial traction on the arm, (2) ensured stability throughout a full range of motion, and (3) palpated for tension in the conjoint tendon and deltoid muscle after trial reduction [1]. The humeral stem was cementless and in < 90% a short stem, with a total neck-shaft angle of 147.5°.
Statistical analysis
Descriptive statistics, including means and standard deviations, were reported for demographic data and outcome variables. Comparisons between different measurements had a normal distribution and therefore were analyzed for significance using the unpaired Student t test. The level of statistical significance was set at p < 0.05. Statistical analysis was performed with SPSS 18.0 software (SPSS Inc., Chicago, IL, USA).
Source of funding
A funding from Zimmer Biomet was applied to follow-up patients.
Results
A total of 48 patients (50 shoulders) who had undergone a reverse shoulder arthroplasty with a metal augmented glenoid met our inclusion criteria and were enrolled in the study. The majority of patients were male (n = 26; 52%). The mean age was 69 ± 12.65 (42–90) years.
The average postoperative follow-up was 6 months (1–23 months) with a minimum of 1-month follow-up. Patient demographics, pre-operative diagnosis and glenoid morphology (Walch and Favard classification) are presented in Table 1.
There were no scapular stress fractures in our study group during short term follow up.
Individual correction of each glenoid deformity
In the majority of cases the wedge was positioned posteriorly and cranially between 10:00 and 12:00 o’clock. A total of 24 (48%) 10° wedges, 18 (36%) 20° wedges and 8 (16%) 30° wedges were used.
For a better understanding of the individual correction of each deformity, we have divided the total study population of patients with deformities into three groups.
Patients presenting with global deformity (total study population, group I)
Preoperative and postoperative correction data for all patients 48 patients (50 shoulders) are presented in Table 2.
Scapular notching was not observed in our patients and relevant perioperative complications were not observed.
Patients with a predominantly glenoid retroversion (> 20°; group 2)
Preoperative and postoperative correction data for 20 patients (20 shoulders) with a glenoid retroversion greater than 20° are presented in Table 3.
The number of female and male patients was equal. The mean age was 67 ± 12 (42–86) years. The predominant side operated was right (12 (60%)). In the majority of cases the wedge was positioned posteriorly and cranially at 10:30 o’clock. A total of 7 (35%) 10° wedges, 6 (30%) 20° wedges and 7 (35%) 30° wedges were used.
Scapular notching was not observed in our patients and relevant perioperative complications were not observed.
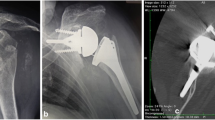
Figures 1 and 2 show the preoperative and postoperative retroversion. Figure 3 shows the preoperative planning image using Signature One Planner.
Patients with a predominantly cranial glenoid dysplasia (group III)
Preoperative and postoperative correction data for 17 patients (17 shoulders) with a cranial glenoid dysplasia are presented in Table 4.
The majority of patients were female (n = 10; 59%). The mean age was 71 ± 13 (42–90) years. The predominant side operated was right (12 (70.59%)). In all cases the wedge was positioned cranially at 12:00 o'clock to correct the inclination. A total of 12 (70.59%) 10° wedges and 5 (29.41%) 20° wedges were used.
Relevant perioperative complications were not observed.
Figures 4 and 5 show the preoperative and postoperative RSA angle. Figure 6 shows the preoperative planning image using Signature One Planner. Figure 7 shows the postoperative SBOD.
Discussion
The objective of the current study was to analyze pre- and postoperative shoulder radiographs and CT scans to determine the correction of a glenoid deformity in RSA using a metal augmented hemi-wedge baseplate. We measured pre- and postoperative glenoid version, inclination, distalisation and lateralization to evaluate the 360-degree correction potential of the preoperative deformity.
Preoperatively, we classified the glenoid deformity according to the Walch [11] and Favard classifications [4, 13]. While the optimum method for correcting superior glenoid inclination in RSA is debatable, it is crucial to rectify it to a neutral position (RSA angle 0°) and thereby avoid the superior baseplate tilt [19, 20]. For the measurement of the glenoid inclination (RSA angle), the supraspinatus fossa line is a consistent reference line due to this sclerotic line is visible on true AP shoulder radiographs and CT scans. In addition, from a biomechanical perspective, the supraspinatus fossa line points the course of action of the rotator cuff muscles [21]. The goal of preoperative planning in RSA should therefore be to achieve an RSA angle measurement of 0°, which means that the baseplate should be implanted in neutral inclination in relation to the supraspinatus fossa line. In such a scenario, the trajectories of the other cuff muscles are orthogonal and potentially more efficient [12, 21,22,23].
Various techniques have been proposed to correct the superior glenoid inclination by performing a RSA [20, 24]. A 2016 Nebraska study demonstrated that neither the subchondral smile reaming technique nor the 10° cannulated guide pin technique are reliable methods for correcting superior glenoid tilt [25].
Possibly not all glenoid defects may require deformity correction. This is supported by reports from McFarland et al. Here a medialized center of rotation with asymmetric reaming was chosen for best possible baseplate positioning, which however does not necessarily lead to a sufficient deformity correction and may lead to a violation of the subchondral bone [3]. However, in order to correct a large amount of superior inclination or retroversion, it may require reaming out a large amount of native bone, potentially endangering the bone mass and too much medializing the glenoid component, as well as the center of rotation, which can lead to prosthetic instability, scapular notching, glenoid loosening and reduced mobility [8, 26, 27]. To prevent this, there are three reliable surgical options that can be used: (1) inferiorly inclined bone graft as wedged BIO-RSA [27], (2) patient-specific baseplate or (3) metal superior augmented baseplate [5].
Therefore, in our surgical practice, our preference is the use of a metal augmented hemi-wedge baseplate once a threshold of 10° of pathological glenoid version or inclination is exceeded. This hemi-wedge baseplate allows a correction in at least 2 planes in combination with a bone preserving reaming-technique. In particular, the convenience of this technique combines the adaptability to individually reconstruct defects not only of the glenoid inclination but also of the version, as well as the better adaptation of the baseplate without graft compression like in the BIO-RSA [27,28,29]. In our hands this technique is not time-consuming in the OR after a learning curve, nor it is associated with extensively higher implant expense, and does avoid the need for a bone integration of a wedged bone block.
To correct preoperative deformity, a 3D planning system is mandatory, to allow a perfect positioning of the augmented baseplate. We use the Signature™ ONE surgical planning software[30] (Zimmer Biomet, Warsaw, Indiana, USA) which provides a 3D image-based approach to preoperative visualization, surgical planning and patient-specific guide creation, based on each patient´s unique anatomy, to anticipate the direction and size of the metallic augmentation.
The results show that the mean preoperative RSA angle in our total cohort in our study was 19.8° ± 7.37 (2.3–32.7), which clearly shows an increased superior inclination. The mean preoperative results of the glenoid version calculation demonstrate that most of the glenoids were in retroversion. The highest retroversion of the glenoid is evidenced in the proximal section (− 11.7 ± 11.44 (− 32.1 ± 14.4)), in accordance with prevision measurements [31]. Anatomically the reduction of the retroversion at the middle of the glenoid is the demonstration of the spiral twist of the glenoid (− 9.41 ± 9.19 (− 24.6 to 6.7)), and so on at the distal section (− 6.61 ± 8.11 (− 24.1 to 10.2)). Postoperative after the implantation of a metallic augmented hemi-wedge basis plate we were able, first, to anatomically correct the RSA angle to 0.56° ± 2.89 (− 5.6 to 5.5) and, second, the glenoid retroversion in the proximal section to − 7.46 ± 5.92 (− 20.4 to 2.5), as well as in the middle section to − 7.86 ± 5.75 (− 20.4 to 2.2). This is due to the fact that our metallic augmented basis plates were positioned between 10 and 12 o’clock; we can demonstrate that it has been possible to make a 3D correction particularly in the proximal and middle glenoid section.
The results further demonstrate that in our group with a retroversion greater than 20° at the proximal third we were able to correct combined both the retroversion as well as the inclination in that we positioned the metallic augment posteriorly and cranially (10:30 o’clock). There was a statistical significance (p < 0.05) in the correction of these deformity on the RSA angle from 16°, the glenoid version at the proximal third from 23°, at the middle third from 19° and at the distal third from 13.81 to 0.08°, − 7.87°, − 7.03° and 7.98°, respectively. These data clearly demonstrate that by adjustment of the wedge at the 10:30 o’clock, we were able to correct the version to the largest degree on the upper third of the glenoid, rather than on the distal part of the glenoid. In our group 3, in patients with a cranial glenoid dysplasia we were able to statistical significant (p < 0.0001) reconstruct the RSA angle from 22.76° ± 6.06 (12.1–32.7) to 0.19° ± 2.7 (− 5.6 to 5.1). In this group were predominantly a dysplasia Favard Type E1 which with its concentric erosion presents a risk of a superior baseplate tilt and therefore a challenge to achieve an anatomically reconstruction. Because of the positioning of the metallic augmented base plate at 12:00 o’clock, the glenoid version was not affected by the augment.
Another important aspect by the glenoid positioning is attempted to avoid a scapular notching by both lateralization and by inferiorizing the glenoid base plate. Notching is hypothesized to be secondary to the contact between the polyethylene on lay tray and the bone just inferior and medial to the base plate. Further bone loss occurs as a result of this direct contact and results in polyethylene debris particles that can lead to additional bone loss and possible aseptic loosening of the glenoid or humeral component [17, 32,33,34,35].
A recent study from the Mayo clinic showed that a SBOD below 2.35 mm is a strong predictor for a greater notching grade [16]. In our study, scapular notching was not observed, what is strongly supported by our postoperative SBOD of 5.32 mm ± 1.99 (2.6–10.8).
There are few more reports of correction of glenoid dysplasia by metal augments or wedged BIO-RSA. Boileau et al. reported an considerably improvement of the RSA angle from preoperative numbers of 28° to 8.6°, and an improvement of the glenoid version from − 12.1° to − 4.7° postoperatively after wedged BIO-RSA [8]. Similarly, Kirsch et al. reported an improved version from 28° to 16° after usage of an metallic implant, and an improved β-angle from 67° to 81° postoperatively, respectively [36].
In the last year there has been increasing interest in metal augments in order to correct deformities and to prevent medialization of the joint line. Zhou et al. described very recently the use of metallic hemi-wedges similar to ours and showed that they were able to prevent a medialized joint line resulting in a lateralized baseplate and sphere position [5].
Eventually, these newer bone preserving techniques including the usage of the presented hemi-wedge need to be compared with the good mid-term results after usage of a standard baseplate without bone grafting or augments as proposed [3]. Therefore, it is mandatory to collect such long term clinical and radiographic data to evaluate the benefits of deformity correction by bone and metal augments compared to current standard techniques without correction.
Limitations
First, our patient population includes only patients with Osteoarthrosis. However, in our database there were some fractures or the proximal humerus, which were indicated to RSA. Second, our study was only based on radiographic images, and in consequence it does not include patient-reported outcome measures. Therefore, the final valuation whether metallic augments are beneficial is dependent on the clinical long-term outcome and revision rates. Third, our metallic augmented base plate hat fixed 10°, 20° or 30, which limited our judgement to more closely achieve an anatomical result. The current study results were not able to show the degree of bone preservation by the use of a wedged glenoid. We need to address this important aspect in further volumetric measurements.
Conclusion
Using a new 360-degree metal-augmented hemi-baseplate, the preoperative pathological inclination and retroversion can be corrected in a combined and/or individually reliable way. Future clinical long-term results will show whether this will lead to even improved clinical outcomes compared to wedged BIO-RSA or standard baseplates without deformity correction.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J shoulder Elb Surg. 14(1 Suppl S):147S-161S
Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16(1):65–68
McFarland EG, Huri G, Hyun YS, Petersen SA, Uma SM, Investigation (2016) Reverse total shoulder arthroplasty without bone-grafting for severe glenoid bone loss in patients with osteoarthritis and intact rotator cuff Edward. J Bone Jt Surg. 98-A(21):1801–1807
Lévigne C, Garret J, Boileau P, Alami G, Favard L, Walch G (2011) Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res 469(9):2512–2520
Zhou Y, English RTR, Van Niekerk M, Hirner M (2022) Reverse shoulder arthroplasty with metallic augments to preserve bone and restore joint line in patients with glenoid bone loss. Semin Arthroplast JSES 32(4):824–833. https://doi.org/10.1053/j.sart.2022.05.001
Bauer S, Corbaz J, Athwal GS, Walch G, Blakeney WG (2021) Lateralization in reverse shoulder arthroplasty. J Clin Med 10(22):1–14
Dimock R, Fathi Elabd M, Imam M, Middleton M, Godenèche A, Ali NA (2021) Bony increased-offset reverse shoulder arthroplasty: a meta-analysis of the available evidence. Shoulder Elb 13(1):18–27
Boileau P, Moineau G, Roussanne Y, O’Shea K (2017) Bony Increased Offset-Reversed Shoulder Arthroplasty (BIO-RSA). JBJS Essent Surg Tech 7(4):e37
Werthel J-D, Walch G, Vegehan E, Deransart P, Sanchez-Sotelo J, Valenti P (2019) Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int Orthop 43(10):2349–2360
Harman M, Frankle M, Vasey M, Banks S (2005) Initial glenoid component fixation in “reverse” total shoulder arthroplasty: a biomechanical evaluation. J Shoulder Elb Surg. 14(1 Suppl S):162S-167S
Walch G, Badet R, Boulahia A, Khoury A (1999) Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty 14(6):756–760
Boileau P, Gauci MO, Wagner ER, Clowez G, Chaoui J, Chelli M et al (2019) The reverse shoulder arthroplasty angle: a new measurement of glenoid inclination for reverse shoulder arthroplasty. J Shoulder Elb Surg 28(7):1281–1290
Maurer A, Fucentese SF, Pfirrmann CWA, Wirth SH, Djahangiri A, Jost B et al (2012) Assessment of glenoid inclination on routine clinical radiographs and computed tomography examinations of the shoulder. J Shoulder Elb Surg 21(8):1096–1103. https://doi.org/10.1016/j.jse.2011.07.010
Fulin P, Kysilko M, Pokorny D, Padr R, Kasprikova N, Landor I et al (2017) Study of the variability of scapular inclination and the glenoid version—considerations for preoperative planning: clinical-radiological study. BMC Musculoskelet Disord 18(1):1–8. https://doi.org/10.1186/s12891-016-1381-4
Domos P, Checchia CS, Walch G (2018) Walch B0 glenoid: pre-osteoarthritic posterior subluxation of the humeral head. J Shoulder Elb Surg 27(1):181–188
Duethman NC, Aibinder WR, Nguyen NTV, Sanchez-Sotelo J (2020) The influence of glenoid component position on scapular notching: a detailed radiographic analysis at midterm follow-up. JSES Int 4(1):144–150. https://doi.org/10.1016/j.jses.2019.11.004
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Jt Surg Br. 86(3):388–395
World Medical Association. Declaration of Helsinki. Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects. [Internet]. 2008. https://www.wma.net/wp-content/uploads/2018/07/DoH-Oct2008.pdf
Favard L, Berhouet J, Walch G, Chaoui J, Lévigne C (2017) Superior glenoid inclination and glenoid bone loss. Orthopade 46(12):1015–1021. https://doi.org/10.1007/s00132-017-3496-1
Laver L, Garrigues GE (2014) Avoiding superior tilt in reverse shoulder arthroplasty: a review of the literature and technical recommendations. J shoulder Elb Surg 23(10):1582–1590
Van Haver A, Heylen S, Vuylsteke K, Declercq G, Verborgt O (2016) Reliability analysis of glenoid component inclination measurements on postoperative radiographs and computed tomography-based 3D models in total and reversed shoulder arthroplasty patients. J Shoulder Elb Surg 25(4):632–640. https://doi.org/10.1016/j.jse.2015.09.003
Konrad GG, Markmiller M, Jolly JT, Ruter AE, Sudkamp NP, McMahon PJ et al (2006) Decreasing glenoid inclination improves function in shoulders with simulated massive rotator cuff tears. Clin Biomech. 21(9):942–949. https://doi.org/10.1016/j.clinbiomech.2006.04.013
Kandemir U, Allaire RB, Jolly JT, Debski RE, McMahon PJ (2006) The relationship between the orientation of the glenoid and tears of the rotator cuff. J Bone Jt Surg Ser B 88(8):1105–1109
Nicholson GP, Strauss EJ, Sherman SL. Scapular Notching: Recognition and Strategies to Minimize Clinical Impact. Clin Orthop Relat Res [Internet]. 2011;469(9). https://journals.lww.com/clinorthop/Fulltext/2011/09000/Scapular_Notching__Recognition_and_Strategies_to.18.aspx
Dilisio MF, Warner JJP, Walch G (2016) Accuracy of the subchondral smile and surface referencing techniques in reverse shoulder arthroplasty. Orthopedics 39(4):e615–e620
Boileau P, Morin-Salvo N, Gauci M-O, Seeto BL, Chalmers PN, Holzer N et al (2017) Angled BIO-RSA: a solution for the management of glenoid bone loss and erosion. J Shoulder Elb Surg 26(12):2133–2142. https://doi.org/10.1016/j.jse.2017.05.024
Boileau P, Moineau G, Roussanne Y, O’Shea K (2011) Bony increased-offset reversed shoulder arthroplasty minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 469(9):2558–2567
Wright TW, Roche CP, Wright L, Flurin P-H, Crosby LA, Zuckerman JD (2015) Reverse shoulder arthroplasty augments for glenoid wear. Comparison of posterior augments to superior augments. Bull Hosp Jt Dis. 73(Suppl 1):S124–S128
Martin EJ, Duquin TR, Ehrensberger MT (2021) Reverse total shoulder arthroplasty baseplate stability in superior bone loss with augmented implant. J Shoulder Elb Arthroplast 5:247154922110206
Guide B. Signature TM ONE Planner
Samim M, Virk M, Mai D, Munawar K, Zuckerman J, Gyftopoulos S (2019) Multilevel glenoid morphology and retroversion assessment in Walch B2 and B3 types. Skeletal Radiol 48(6):907–914. https://doi.org/10.1007/s00256-018-3095-1
Nam D, Kepler CK, Nho SJ, Craig EV, Warren RF, Wright TM (2010) Observations on retrieved humeral polyethylene components from reverse total shoulder arthroplasty. J Shoulder Elb Surg 19(7):1003–1012. https://doi.org/10.1016/j.jse.2010.05.014
Roche CP, Marczuk Y, Wright TW, Flurin PH, Grey S, Jones R et al (2013) Scapular notching and osteophyte formation after reverse shoulder replacement: radiological analysis of implant position in male and female patients. Bone Jt J. 95B(4):530–535
Roche C, Flurin P-H, Wright T, Crosby LA, Mauldin M, Zuckerman JD (2009) An evaluation of the relationships between reverse shoulder design parameters and range of motion, impingement, and stability. J Shoulder Elb Surg 18(5):734–741. https://doi.org/10.1016/j.jse.2008.12.008
Sadoghi P, Leithner A, Vavken P, Hölzer A, Hochreiter J, Weber G et al (2011) Infraglenoidal scapular notching in reverse total shoulder replacement: a prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord. https://doi.org/10.1186/1471-2474-12-101
Kirsch JM, Patel M, Singh A, Lazarus MD, Williams GR, Namdari S (2021) Early clinical and radiographic outcomes of an augmented baseplate in reverse shoulder arthroplasty for glenohumeral arthritis with glenoid deformity. J Shoulder Elb Surg. 30(7 Supplement):S123–S130
Funding
The study was funded by Zimmer Biomet.
Author information
Authors and Affiliations
Contributions
Conceptualization, TG, LN and BU; Formal analysis, LN and SS; Investigation, LN and TG; Methodology and Supervision, LN, TG and JW; Writing—original draft, LN and TG and BU; writing—review and editing, TG, LN, MB, AZ and BU. All authors have approved the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
TG is a paid lecturer by Zimmer Biomet. There are no potential competing interests of any other Author or Co-Author.
Consent for publisher
The content of the manuscript has not been published or submitted for publication elsewhere.
Ethical approval
We confirm that all methods were performed in accordance with the relevant guidelines and regulations. The patients gave written informed consent for participation. The study was conducted according to the guidelines of the Declaration of Helsinki. The ethics commission of the Landesaerztekammer Baden-Wuerttemberg, Germany, approved all procedures (F-2022-005).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guehring, T., Navas, L., Westrich, J. et al. Analysis and 3D correction of glenoid dysplasia with metal hemi-wedge base plate augment: short-term radiographic outcomes. Arch Orthop Trauma Surg 143, 4763–4772 (2023). https://doi.org/10.1007/s00402-023-04781-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04781-6