Abstract
Introduction
Revision total knee arthroplasty (RTKA) has been increasing continuously. The results of RTKA still remain unsatisfactory. Failure patterns and risk factors in RTKA were thoroughly analyzed, with periprosthetic joint infections (PJI) and aseptic loosening remaining at the forefront of re-revision (ReRTKA) causes. While there is evidence that stem profile impacts the revisability of cemented implants, its association with the modes of RTKA failure is unknown.
Methods
50 consecutive ReRTKA performed in a single orthopedic center during 2016–2017 were retrospectively analyzed. The cases were stratified according to age, sex, number of preexisting revisions, fixation technique, stem design and causes of re-revision. All explanted implants with conical vs. cylindrical stem profiles were compared.
Results
Mean age was 67 ± 11.5, and 54% were females. 72% of the cases had ≥ 3 previous revisions. 88% were full-cemented, 3% hybrid and 9% press-fit stems. 36% of the RTKA had conical, 58% cylindrical and 6% combined stem profiles. 92% of the RTKA components were removed. Removal causes were: PJI (52.2%), aseptic loosening (34.8%), implant malposition (9.8%), painful knee (1.1%) and instability (2.2%). While the overall RTKA failure patterns were equally distributed between conical and cylindrical stems, subgroup analysis of only cemented ReRTKA revealed a higher incidence of aseptic loosening within cylindrical stem profiles (46.7% vs. 25.7%, P = 0.05).
Conclusion
Stem profile may have an impact on the process of aseptic loosening in cemented non-metaphyseal engaging RTKA, with cylindrical designs tending to worse outcomes than conical designs. Large cohort studies could provide more clarity on current observation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Data from national arthroplasty registries and the current available literature indicate an increasing incidence of revision total knee arthroplasty (RTKA) and with it of re-revisions (ReRTKA) worldwide [1,2,3,4,5,6,7,8,9]. This trend poses a great challenge for the present and an even greater burden for the future healthcare and economic system [10,11,12].
With RTKA failure rates ranging between 10–30%, the RTKA outcomes are still unsatisfactory [13,14,15,16,17,18,19,20,21,22,23,24]. The two most common causes of ReRTKA remain the periprosthetic joint infection (PJI) (21–46%), followed by aseptic loosening (20–30.5%) [14, 15, 19, 20, 24, 25]. Thus, the importance of identifying and preventing potential risk factors of RTKA failure becomes even greater.
Stem design seems to play an important role not only in the primary stability of RTKA implants [26], but also in the revisability of ReRTKA and, therefore, in their overall outcomes. Conical stem profile is a macroscopic design property defined by its angle and proportion of the conical part within a stem length (Table 1). Conical stem designs are associated with a significantly easier removal than cylindrical stems in the setting of well-fixed cemented RTKA stem extensions [27, 28]. As far as our experience goes, we can only confirm this observation, as increased morbidity is often linked to revisions of well-fixed cylindrical long stems, where often an extended osteotomy is necessary to facilitate controllable component removal. Although existing data from the domain of revision total hip arthroplasty suggest that conical stems are associated with better implant osteointegration rates than cylindrical stems in complex revision cases [29], no literature exists so far, in terms of evaluating the impact of conical stem profile on the failure patterns in revision total knee arthroplasty implants.
The purpose of the current study was to perform an observational analysis of the RTKA failure modes that have led to ReRTKA and compare the causes of implant removal between conical and cylindrical stem profiles. Relevant factors such as anchoring technique of the stem (full-cemented, press-fit, hybrid), metaphyseal fixation (cones/sleeves) and the case complexity (number of previous revisions) were taken into account. Lastly, a thorough review of the exiting literature on the outcomes of stemmed RTKA implants after (a) complex primary and (b) revision cases was conducted in “Discussion” to serve as benchmark for our findings and to facilitate the understanding of its background.
Methods
Ethical approval from the local Institutional Review Board was granted. A single-center retrospective epidemiological analysis was initiated in an orthopedic teaching hospital.
All consecutive ReRTKA with implant removal that took place between 2016 and 2017 including constrained and semi-constrained implant revisions were recruited. Demographic data were collected using the institutional database. All RTKA failure patterns requiring implant removal were identified.
Exclusion criteria were re-revisions with only spacer exchange/removal or liner exchange, isolated patella revisions, explantation of implants that did not possess a stem extension or revisions due to malignancies. Lastly, RTKA reimplantations in the context of a two-stage exchange were also not considered in this study.
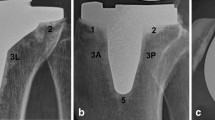
All RTKA stems were stratified according to their profile in (1) conical (Co), (2) cylindrical (Cy) and (3) conical–cylindrical or cylindrical–conical combined designs (Combi). The angles of the conical stem profile were measured using the 2D preoperative planning software MediCAD® orthopedic solution (MediCAD Hectec GmbH, Altdorf/Landshut, Germany) (Fig. 1a–h).
a–h Measurements of the conical stem profile of some established RTKA systems using the preoperative planning software MediCAD® orthopedic, German version. Red color: conical part of the stem, green color: cylindrical part of the stem. a ENDO-Model SL cemented (LINK), b MUTARS GenuX cemented (Implantcast), c Enduro cemented (Aesculap), d Columbus cemented (Aesculap), e M.B.T. Revision Tibia Tray cemented (DePuy), f NexGen LCCK cemented (Zimmer), g RT-PLUS Monobloc cemented (Smith & Nephew), h RT-PLUS Modular cemented and cementless (Smith & Nephew). CAVE: Measurements may vary from the original manufacturer’s values
The fixation techniques of the stems were divided into (1) full-cemented, (2) cementless and (3) hybrid. The numbers of previous RTKA performed in each case until index surgery were noticed and quantified in: one previous (1R), two previous (2R), three previous (3R) and more than three previous revisions (> 3R). The removed femoral and tibial components including their corresponding stem extensions and the presence or not of a metaphyseal fixation were separately analyzed.
The obtained data were then compared between RTKA implants with (1) conical stems and (2) cylindrical stems. A subgroup analysis including only full-cemented stems was also conducted to improve sample homogeneity.
The software IBM SPSS Statistics (Version 25) was used to carry out statistical analyses. For differences between groups, the non-parametric two-sided Mann Whitney U-test or Kruskal Wallis test were performed. The Chi-Square test was used to compare frequencies.
Results
A total of 50 ReRTKA cases (100 components, respectively) with stem revision were included in the study. All demographics and epidemiological data collected are summarized as follows (Table 2). The mean age of the patients was 67 ± 11.5 years and 54% were females. From the revised RTKA implants, 18 (36%) had conical stems, 29 (58%) cylindrical stems and 3 (6%) combined stem designs. 88% of the stems revised were full cemented and 12% cementless or hybrid (only metaphysis cemented). 72% of the cases were complex ReRTKA with three or more previous revisions.
A total of 92 of the 100 components included in the study (92%) were explanted, 51% of which were on the femoral side and 49% on the tibial side of the joint. Within all removed components, there was 1 (1.1%) metaphyseal cone on the femoral side and 12 (13%) sleeves (6 femoral, 6 tibial), all of which were combined with cementless/hybrid stem fixation. 35 out of 36 (97.2%) conical stems vs. 52 out of 58 (89.7%) cylindrical stems and 5 out of 6 (83.3%) combined design stems were removed during index ReRTKA.
The comparative analysis between conical and cylindrical stem revisions showed a good sample homogeneity with no statistical differences in revision complexity and the other demographic and epidemiological parameters included in the study.
The RTKA failure patterns of all 92 removed components in this cohort, sorted in descending order, were as follows: 52.2% PJI (47.8% on well-fixed implants and 4.4% on loose implants), 34.8% aseptic loosening, 9.8% implant malposition, 1.1% painful knee and 2.2% instability. Incidence comparison of the ReRTKA causes that led to implant removal between the two groups (Co vs. Cy stems) revealed an equal distribution of all RTKA failure patterns between the two stem designs with no statistical differences.
After extracting all cementless and hybrid stem fixation techniques and implants with metaphyseal fixations (cone/sleeves), to improve sample homogeneity, a subgroup analysis involving only cemented stems was conducted (Table 3). All conical stems (36/36) vs. 86.2% (50/58) of cylindrical stems were cemented. 35 out of 36 (97.2%) cemented conical stems vs. 45 out of 50 (90%) cemented cylindrical stems were explanted during index ReRTKA. The RTKA failure patterns of all 82 removed cemented components were as follows: 54.9% PJI, 36.6% aseptic loosening, 6.1% implant malposition, 0% painful knee and 2.4% instability. While there were no statistical differences in the incidences of PJI, malposition and instability between conical and cylindrical stem revisions, aseptic loosening occurred significantly more often in the full-cemented cylindrical stems (P = 0.05) when compared with conical stem profiles (Fig. 2).
a, b Comparison of failure patterns of the RTKA components removed between Co and Cy stem profiles for a all RTKA implants included in the study (cemented and press-fit stems) and b only cemented stems. The values above the bars represent the level of significance as assessed by the Chi square test. *Significance at the 0.05 level
Discussion
Main findings of the study
The main finding of this study is the association found between aseptic loosening and stem profile in failed cemented RTKA implants. While there was an equal distribution of all RTKA failure patterns observed between conical and cylindrical stem profiles in our initial cohort of 50 ReRTKA cases, with PJI remaining the most common failure reason, followed by aseptic loosening, a subgroup analysis of failed RTKA components with only full-cemented stems revealed a higher incidence of aseptic loosening in implants with cylindrical stems when compared to those with conical stem profiles reaching statistical significance (46.7% vs. 25.7%, P = 0.05).
The role of stem in RTKA implant fixation
The role of stems in the primary and secondary stability of constrained implants is well known. It supports implant fixation by improving the distribution of shear loads, especially when epi-/metaphyseal bony defects > 5 mm are involved. It reduces the stresses on the bone–cement interface [30,31,32] and on the stem–condyle junction, which may otherwise lead to trunnion failure especially when no additional metaphyseal support coexists. Thus, based on the concept of the three fixation zones in RTKA [33], the use of cones [34, 35] or sleeves [36,37,38] in combination with a stem extension is becoming even more popular, as it shows improved clinical outcomes and lower rates of aseptic loosening [39,40,41]. Furthermore, offset stems can be useful in preventing component impingement and malalignment, as seen with straight diaphyseal-engaging cementless stems on bones with deformities [42].
Cement fixation in RTKA has various advantages [21, 32, 43,44,45,46,47]. It compensates incongruences of the cancellous bone and increases the contact surface to the implant, providing a more homogeneous load distribution [48]. It is for that reason, and at same time due to the excellent long-term results, that many surgeons traditionally advocate cemented stem fixation [49,50,51,52,53,54]. Nevertheless, there are also some drawbacks and pitfalls to consider, such as that of a progressive resorption below the tibial component that may occasionally occur, or the challenging revision of cemented voluminous cylindrical stems that are still well-fixed during their removal. Previous studies pointed out that short cemented stems with a conical profile angle of at least 0.5° may be for this reason preferable [27, 28, 55].
The mechanical properties of a stem design in RTKA involves several features, each one of them playing a decisive role in the biomechanics and anchoring mechanism of RTKA implants.
-
(1)
Surface roughness
Depending on the values of implant surface roughness, cement adhesion and abrasion properties can differ [56, 57]. Smoothly polished stems are most commonly used in cemented fixation. Although they can depict micromotions within the intact cement sheath, no damage of interface occurs. On the other hand, stems with a rough surface provide a stronger bond with the cement; however, a microscopic undercutting that takes place within the cement–implant interface may lead to an earlier stem migration and, inevitably, to failure of the cement integrity and implant loosening. The cutoff values of implant surface roughness, above which a significant increase of loosening risk may occur, is yet undefined and difficult to examine. Thus, various satin to matte manufactured stem extensions are commonly used for both, cemented and cementless fixation techniques.
-
(2)
Cross-sectional design
The cross-sectional design of cemented tibial short stems in primary TKA appears to have an impact on the surrounding bone density. In a prospective study of 20 cemented TKA, cylindrical stems revealed in a follow-up (FU) of 7 years more heterogeneous BMD changes beneath the tibial component compared to cruciform stems. The most density decrease was observed on the medial side. This was postulated as a risk for component migration [58]. Stem extensions with flutes and pronounced corners are commonly used in press-fit fixations to engage cortical bone and provide a higher resistance against torsional loads equal to those observed in daily activities [59, 60]. In cases of cemented fixation, the pronounced corners produce higher peak stresses on the surrounding cement, which may, subsequently, increase the risk of breakage of the cement mantle and lead to early loosening. Thus, rounded and scalloped stem designs have become the standard [61].
-
(3)
Size (length and diameter)
Lee et al. [62] examined 65 press-fit semi-constrained knee prostheses, the impact of stem design (length and diameter) and the canal filling ratio (CFR) on the incidence of aseptic loosening. In an FU of 24 months, the incidence rates of aseptic loosening were equal for the femoral and tibial components. A CFR of > 0.85 was associated with reduced rates of aseptic loosening. They suggested either a CFR > 0.85 or a > 0.70 with > 4.3 cm stem engagement, tibial, and > 2 cm stem engagement, femoral. While, in hybrid or cementless fixation techniques maximal canal filling of press-fit stems is advocated [63], biomechanical studies have shown that equal primary stability can be achieved also via metaphyseal cemented stems [64]. However, according to recent studies on cemented short stems, a femoral canal wider than 19 mm inner diameter at 20 cm proximal to the joint line was linked to higher rates of aseptic loosening after cemented rotating hinge RTKA implants [39, 65, 66]. Finally, well-fixed cemented voluminous cylindrical stems are associated with an increased index of surgical invasiveness when revised und should be possibly avoided, especially if a potential re-revision is highly suspected (e.g. increased risk for infection recurrence) [28, 55].
-
(4)
Conical stem profile
According to recent data, cemented conical stems can be more easily removed than cylindrical shaft extensions and, therefore, may be associated with reduced invasiveness and surgery time during exchange procedures [27, 28].
Regarding stem fixation mechanism, cylindrical press-fit stems require a shorter engagement length than conical stems to achieve primary stability [26]. Nevertheless, stem engagement of less than 4 cm is associated with a higher risk of implant loosening [54, 67] and shaft pain due to peak stresses at the tip of the stem may result. Thus, tightly implanted diaphyseal press-fit stems can lead to end of stem pain and poor patient satisfaction [32, 43,44,45,46,47]. In a recent retrospective study of 20 cemented TKA, cylindrical stems revealed heterogeneous epiphyseal BMD decreases, which was postulated as a risk factor for component migration [58]. While cylindrical stems are commonly used with press-fit or hybrid fixation techniques and short conical stems with cemented fixation methods, it is not infrequent that orthopedic surgeons are confronted with revisions of cemented cylindrical stems or stem designs that possess in most parts of stem length a cylindrical profile (Fig. 3a, b).
The role of stem design in RTKA outcomes: a comparative review of the literature
Despite the existing literature upon stem design in RTKA so far, there is still not much evidence dealing with the impact of stem profile on failure patterns of RTKA and its association with aseptic loosening.
A comprehensive overview of the literature to assess survival rates and incidences of aseptic loosening and PJI with particular focus on the conical profile of RTKA stems (Co vs. Cy designs) was conducted to serve as benchmark and to facilitate a better understanding of our observations. A total of 106 studies including both, solely revisions (n = 67) (Table 4) and complex primary TKA cases (± revisions) (n = 39) (Table 5), have been reviewed and filtered as shown in the flowchart (Fig. 4a, b).
a, b Literature analysis: a process flowchart of the included studies for (left) solely revisions and (right) primary TKA (± revisions), divided according to stem profile (conical vs. cylindrical) and fixation technique of the stem (cemented or cementless). b Summary of overall outcomes separating TKA from RTKA, and Co from Cy stem profiles. Use of cement on stems and metaphyseal fixation (cones/sleeves) are noted in percentage
In the solely RTKA publication group (1985–2021), 8623 cases (involving 971 infections) were included. In 41 of 67 (61.2%) studies, a metaphyseal fixation (cones and sleeves) was used in variable frequencies, mostly combined with cementless cylindrical stems. An overall of 33 ± 42% of stems were cemented (Co 100% vs. Cy 11.6%). The mean FU time in years was 5.2 ± 7.7 (1.5–10.5). Comparing the data selected between Co vs. Cy stems after excluding studies with undefined implants, no differences in overall outcomes could be detected. With similar 10-year survival rates of 85.9 ± 15.3% (75–96.7%) for Co and 88.9 ± 5.6% (81–97.8%) for Cy, the incidences of aseptic loosening and PJI were identical for both, Co: 5.1 ± 6.3% (0–20%) vs. Cy: 3.5 ± 5% (0–26%) and Co: 4.3 ± 3.5% (0–12%) vs. Cy: 5.7 ± 4.1% (0–16%), respectively. Equal relations of outcomes were observed also in the comparison of the RTKA implants in primary ± revision group (Fig. 4a, b).
Comparing the literature data presented with our findings, a lower overall incidence of aseptic loosening and PJI was obviously noticeable. This can be attributed to a cohort inhomogeneity (TKA vs. RTKA, risk factors and complexity of cases, number or previous revisions, septic vs. aseptic, use of metaphyseal fixation, FU time, implant design and fixation technique, missing values, study design, industry influence, etc.) that leads to a wide discrepancy of outcomes that range from excellent [36, 40, 55, 68,69,70,71,72,73,74,75,76,77] to moderate results [16, 20, 24, 41, 62, 78,79,80]. However, when considering recent (2008–2020) high-volume studies that are not associated with a certain implant, the incidence rates of aseptic loosening and PJI are more representative and coincide with our data: Suarez et al. in a series of 566 RTKA cases (including 123 PJI) published a 12-year survival of 82% with 19% aseptic loosening and 46% PJI [19]. Aggarwal et al. followed 168 RTKA cases (44 PJI) for a mean time of 5.6 years. Complex cases with ≥ 3 previous revisions were associated with increased risk for aseptic loosening and PJI (38–50% and 50–63%, respectively). In a current single-center review of 1632 RKTA (361 PJI) and a mean FU of 5.1 years, the RTKA failure rates due to aseptic loosening was 21% and due to PJI 38.5% [24].
When assessing studies using Co vs. Cy stem designs, the majority of published data on Cy stems are performed in press-fit/hybrid fixation techniques, whereas Co stems are commonly full cemented, which corresponds to the common use in daily praxis. However, there are cases where cylindrical stems can be cemented (e.g., poor bone quality, metaphyseal stems or stems with < 4 cm diaphyseal engagement, bone deformities, implant availability) [23, 49, 81, 82] (Table 4). Fehring et al. compared cemented (53%) with cementless metaphyseal stems on 113 RTKA (33 PJI) and found in an FU > 2 years 0% vs. 10% aseptic loosening in favor of cemented stems [54]. Gililland et al. followed with a multi-center study comparing cemented stems with diaphyseal engaging press-fit stems on 82 aseptic RTKA cases. After an FU of 6–10 years, they found no differences in aseptic loosening (4% vs. 3–6%) or PJI (0% vs. 2.4%) for cemented and cementless diaphyseal stems, respectively. Re-revision rates and radiographic failure rates were similar between groups [67].
In a current study on 65 aseptic RTKA cases with cementless Cy stems, 26% of revision implants failed after 2 years FU due to aseptic loosening [62].
A study from 2004 on 26 modular segmental rotating hinge RTKA implants with cemented Cy stems (4 primary, 22 revisions) in nonneoplastic limp salvage cases and a mean FU of 5 years found 10-year survival rates < 70%, aseptic loosening in 15.4% and PJI in 19.2% with 27% reoperations and 31% complication rates [79].
In 2015, a Norwegian arthroplasty register study on 1016 cases of various RTKA implants that mostly had Cy stems (85% cemented), published at a median FU of 4.5 years PJI rates of 28%. Tibial loosening occurred in 17% vs. 9% on the femoral side. Partial component exchange, young ages and male patients were found to pose a higher risk for ReRTKA [15].
Abdelaziz et al. compared the 10-years outcomes of 25 aseptic RTKA between pure and rotating hinged designs both with cemented conical stems and 32 cones. He found aseptic loosening in 20%, from which four out of five revised RTKA implants were pure hinged. They concluded that pure hinged RKTA without cones tend toward higher loosening rates [83]. Other studies on RTKA implants with cemented Co stems published aseptic loosening rates of 7.1% for revisions [80] and 0–0.7% for primary implantations [55, 69, 70].
Despite all efforts made so far to improve outcomes by advancing implant design properties, operative techniques and the perioperative management, the RTKA failure rates are still high [14,15,16,17,18,19,20,21,22,23,24,25]. Causes of RTKA failure include PJI (21–63%), followed by aseptic loosening (20–50%), instability (3–26%), stiffness (10.5–23%), implant malposition (3%), painful knee (7.3%), extensor mechanism problems (5.2–12.8%) and periprosthetic fractures (6%) [14, 15, 19, 20, 24, 25].
Thus, highlighted by the need to improve the RTKA results, a meticulous and continuous epidemiological analysis of both patient- and surgery/implant-associated potential risks is of particular importance.
However, confronted with the fact that the existing literature is burdened with a cohort inhomogeneity and a lack of values about the exact design and proportion of conical profile of the stems used, it is difficult to examine the impact of stem conicity on the longevity of the implants and draw reliable conclusions.
When looking into the published data of hip arthroplasty, tapered stems appear to provide superior outcomes than cylindrical stems even in cases of greater bony deficiencies. In a recent multicenter analysis of 105 femoral revisions with Paprosky III–IV, Bedair et al. found at 5 years FU that modular revision stems with conical geometry were associated with lower rates of failed implant osseointegration (1.6% vs. 15.9%, P < 0.01) and stem re-revision (4.9% vs. 22.7%, P = 0.013) than cylindrical stems [29]. Despite the fact that these results may obtain some similarities with our observations in terms of impact of stem conicity on implant survivorships, they cannot be directly compared, as there are substantial differences in biomechanics and anchoring principles between the knee and hip.
Thus, this is the first observational study to provide evidence about the effect of stem conicity on the failure pattern of RTKA.
Compared to cylindrical designs, conical stems seem to have some mechanical advantages: while during press-fit fixations a longer intramedullary engagement length occurs, which might lead to reduced areas of micromotions between stem and cortical bone induced due to the differences in elasticity and rigidity modulus of the materials (less stress shielding, less peak stresses at the tip of the stem), in cases of cemented fixation a cone-shaped cement coat may theoretically reduce the shear stresses and thus the micromotions in the cement–implant interface which in the long-term could otherwise trigger implant migration and bond failure. However, there is still lack of clinical and biomechanical evidence that could confirm the above statements. Conical stems can also be removed more easily than cylindrical stems due to the short displacement required to achieve complete implant detachment [27, 28].
There are several limitations in the current study that may pose potential biases: (1) the small sample size of the subgroups and the retrospective setup of this work, (2) as aforementioned, we did not differentiate hinge designs and level of constraint and did not consider other stem design properties such as length, diameter, offset, bowed profile, and surface roughness values, which might have had also an impact on the failure pattern, (3) we did not report any follow-up time, as focus of this investigation was rather the epidemiological analysis of the failure patterns and not the evaluation of implant survivorship, (4) all values of stem profile of the RTKA stems included in the study were based on measurements conducted using the preoperative planning software MediCAD®, which might involve some variations and thus potential discrepancies between our measurements and the manufacturer’s values. Therefore, the validity of these results is limited. Nonetheless, it is still consistent with the available evidence. Further studies of large series including survival rates are currently being conducted by our research group to bring more clarity to this topic.
Conclusion
PJI remains the most common reason for ReRTKA, independent of the conical profile of RTKA stem extensions. Cemented cylindrical stems may pose a greater risk for aseptic loosening than conical stem designs.
References
Robertsson O, W-Dahl A, Lidgren L, Sundberg M (2020) Swedish knee arthroplasty register. Annual Report 2020. Lund. ISBN 978-91-88017-32-1
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: Annual Report 2020, Adelaide; AOA, 2020:1-474. ISN 1445-3657. https://aoanjrr.sahmri.com/annual-reports-2020
Finish Arthroplasty Register. ENDOnet 2020. https://www.thl.fi/far/#index
Klug A, Gramlich Y, Rudert M et al (2020) The projected volume of primary and revision total knee arthroplasty will place an immense burden on future heath care systems over the next 30 years. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06154-7
Delanois RE, Mistry JB, Gwam CU et al (2017) Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 32:2663–2668. https://doi.org/10.1016/j.arth.2017.03.066
Lewis PL, Graves SE, Robertsson O et al (2020) Increases in the rates of primary and revision knee replacement are reducing: a 15-year registry study across 3 continents. Acta Orthop 91:414–419. https://doi.org/10.1080/17453674.2020.1749380
Schwartz AM, Farley KX, Guild GN, Bradbury TL (2020) Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty 35:S79–S85. https://doi.org/10.1016/j.arth.2020.02.030
Grimberg A, Jansson V, Liebs T, et al. (2015) Endoprothesenregister Deutschland (EPRD). Jahresbericht 2015. Berlin. ISBN: 978-3-9817673-1-5. https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/EPRD-Jahresbericht_2015_FINAL_Web.pdf
Boy O, Hahn S, Kociemba E, BQS-Fachgruppe Orthopädie und Unfallchirurgie (2009) BQS Bundesgeschäftsstelle für Qualitätssicherung. Qualitätsreport 2008. Knie -Endoprothesenwechsel und -komponentenwechsel. https://www.bqs.de/kunden-extranet/bqs-qualitaetsreports-2002-2008.php
Oduwole KO, Molony DC, Walls RJ et al (2010) Increasing financial burden of revision total knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc 18:945–948. https://doi.org/10.1007/s00167-010-1074-8
Bhandari M, Smith J, Miller LE, Block JE (2012) Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord 5:89–94. https://doi.org/10.4137/CMAMD.S10859
Kurtz SM, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am 89:780–785. https://doi.org/10.2106/JBJS.F.00222
Yu S, Szulc A, Walton S et al (2017) Pain control and functional milestones in total knee arthroplasty: liposomal bupivacaine vs. femoral nerve block. Clin Orthop Relat Res 475:110–117. https://doi.org/10.1007/s11999-016-4740-4
Mortazavi SMJ, Molligan J, Austin MS et al (2011) Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop 35:1157–1164. https://doi.org/10.1007/s00264-010-1134-1
Leta TH, Lygre SHL, Skredderstuen A et al (2015) Failure of aseptic revision total knee arthroplasties: 145 Revision failures from the Norwegian Arthroplasty Register, 1994–2011. Acta Orthop 86:48–57. https://doi.org/10.3109/17453674.2014.964097
Aggarwal VK, Goyal N, Deirmengian G et al (2014) Revision total knee arthroplasty in the young patient: Is there trouble on the horizon? J Bone Jt Surg 96:536–542. https://doi.org/10.2106/JBJS.M.00131
Nelson CL, Vanushkina M, Irgit K et al (2015) Stemmed femoral implants show lower failure rates in revision total knee arthroplasty. Knee 22:429–434. https://doi.org/10.1016/j.knee.2015.02.013
Lindberg-Larsen M, Jørgensen CC, Bagger J et al (2016) Revision of infected knee arthroplasties in Denmark. Acta Orthop 87:333–338. https://doi.org/10.3109/17453674.2016.1148453
Suarez J, Griffin W, Springer B et al (2008) Why do revision knee arthroplasties fail? J Arthroplasty 23:99–103. https://doi.org/10.1016/j.arth.2008.04.020
Agarwal S, Kabariti R, Kakar R et al (2019) Why are revision knee replacements failing? Knee 26:774–778. https://doi.org/10.1016/j.knee.2019.04.012
Bini SA, Chan PH, Inacio MCSS et al (2016) Antibiotic cement was associated with half the risk of re-revision in 1154 aseptic revision total knee arthroplasties. Acta Orthop 87:55–59. https://doi.org/10.3109/17453674.2015.1103568
Wilke B, Wagner E, Trousdale R (2015) Long-term survival of a semi-constrained implant following revision for infection. J Arthroplasty 30:808–812. https://doi.org/10.1016/j.arth.2014.10.037
Wilke BK, Wagner ER, Trousdale RT (2014) Long-term survival of semi-constrained total knee arthroplasty for revision surgery. J Arthroplasty 29:1005–1008. https://doi.org/10.1016/j.arth.2013.10.025
Geary MB, Macknet DM, Ransone MP et al (2020) Why do revision total knee arthroplasties fail? A single-center review of 1632 revision total knees comparing historic and modern cohorts. J Arthroplasty 35:2938–2943. https://doi.org/10.1016/j.arth.2020.05.050
Yu S, Saleh H, Bolz N et al (2020) Re-revision total hip arthroplasty: epidemiology and factors associated with outcomes. J Clin Orthop Trauma 11:43–46. https://doi.org/10.1016/j.jcot.2018.08.021
Heinecke M, Rathje F, Layher F, Matziolis G (2018) The proximal and distal femoral canal geometry influences cementless stem anchorage and revision hip and knee implant stability. Orthopedics 41:e369–e375. https://doi.org/10.3928/01477447-20180320-02
Maslaris A, Layher F, Brinkmann O et al (2018) Cemented conical stems can be removed more easily than cylindrical stems, regardless of cone angle in revision knee arthroplasty. Arch Orthop Trauma Surg 138:1747–1754. https://doi.org/10.1007/s00402-018-3053-3
Maslaris A, Layher F, Bungartz M et al (2019) Sagittal profile has a significant impact on the explantability of well-fixed cemented stems in revision knee arthroplasty: a biomechanical comparison study of five established knee implant models. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-019-03160-4
Bedair H, Tetrault M, Choi H-R et al (2013) A comparison of modular tapered vs. modular cylindrical stems for complex femoral revisions) 71–73. J Arthroplasty 28:71–73. https://doi.org/10.1016/j.arth.2013.04.052
Rawlinson JJ, Closkey RF, Davis N et al (2008) Stemmed implants improve stability in augmented constrained condylar knees. Clin Orthop Relat Res 466:2639–2643. https://doi.org/10.1007/s11999-008-0424-z
Rawlinson JJ, Peters LE, Campbell DA et al (2005) Cancellous bone strains indicate efficacy of stem augmentation in constrained condylar knees. Clin Orthop Relat Res 440:107–116. https://doi.org/10.1097/01.blo.0000187340.10003.68
Stern SH, Wills RD, Gilbert JL (1997) The effect of tibial stem design on component micromotion in knee arthroplasty. Clin Orthop Relat Res 345:44–52
Morgan-Jones R, Oussedik SIS, Graichen H, Haddad FS (2015) Zonal fixation in revision total knee arthroplasty. Bone Jt J 97-B:147–149. https://doi.org/10.1302/0301-620X.97B2.34144
Boureau F, Putman S, Arnould A et al (2015) Tantalum cones and bone defects in revision total knee arthroplasty. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2014.11.020
Faizan A, Bhowmik-Stoker M, Alipit V et al (2017) Development and verification of novel porous titanium metaphyseal cones for revision total knee arthroplasty. J Arthroplasty 32:1946–1953. https://doi.org/10.1016/j.arth.2017.01.013
Bugler KE, Maheshwari R, Ahmed I et al (2015) Metaphyseal sleeves for revision total knee arthroplasty: good short-term outcomes. J Arthroplasty 30:1990–1994. https://doi.org/10.1016/j.arth.2015.05.015
Chalmers BP, Desy NM, Pagnano MW et al (2017) Survivorship of metaphyseal sleeves in revision total knee arthroplasty. J Arthroplasty 32:1565–1570. https://doi.org/10.1016/j.arth.2016.12.004
Graichen H, Scior W, Strauch M (2015) Direct, cementless, metaphyseal fixation in knee revision arthroplasty with sleeves—short-term results. J Arthroplasty 30:2256–2259. https://doi.org/10.1016/j.arth.2015.06.030
Levent A, Suero EM, Gehrke T et al (2021) Risk factors for aseptic loosening in complex revision total knee arthroplasty using rotating hinge implants. Int Orthop 45:125–132. https://doi.org/10.1007/s00264-020-04878-2
Brown LR, Clement ND, MacDonald DJ, Breusch SJ (2019) The survivorship of the link endo-rotational hinge total knee arthroplasty: 5–12-year follow-up of 100 patients. Arch Orthop Trauma Surg 139:107–112. https://doi.org/10.1007/s00402-018-3064-0
Abdelaziz H, Jaramillo R, Gehrke T et al (2019) Clinical survivorship of aseptic revision total knee arthroplasty using hinged knees and tantalum cones at minimum 10-year follow-up. J Arthroplasty 34:3018–3022. https://doi.org/10.1016/j.arth.2019.06.057
Hicks CA, Noble P, Tullos H (1995) The anatomy of the tibial intramedullary canal. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199512000-00017
El-Zayat BF, Heyse TJ, Fanciullacci N et al (2016) Fixation techniques and stem dimensions in hinged total knee arthroplasty: a finite element study. Arch Orthop Trauma Surg 136:1741–1752. https://doi.org/10.1007/s00402-016-2571-0
Completo A, Simões JA, Fonseca F, Oliveira M (2008) The influence of different tibial stem designs in load sharing and stability at the cement-bone interface in revision TKA. Knee 15:227–232. https://doi.org/10.1016/j.knee.2008.01.008
Jazrawi LM, Bai B, Kummer FJ et al (2001) The effect of stem modularity and mode of fixation on tibial component stability in revision total knee arthroplasty. J Arthroplasty 16:759–767. https://doi.org/10.1054/arth.2001.25507
Luring C, Perlick L, Trepte C et al (2006) Micromotion in cemented rotating platform total knee arthroplasty: cemented tibial stem vs. hybrid fixation. Arch Orthop Trauma Surg 126:45–48. https://doi.org/10.1007/s00402-005-0082-5
van Loon CJ, Kyriazopoulos A, Verdonschot N et al (2000) The role of femoral stem extension in total knee arthroplasty. Clin Orthop Relat Res 378:282–289
Li MG, Nilsson KG (2000) The effect of the preoperative bone quality on the fixation of the tibial component in total knee arthroplasty. J Arthroplasty 15:744–753. https://doi.org/10.1054/arth.2000.6617
Mabry TM, Vessely MB, Schleck CD et al (2007) Revision total knee arthroplasty with modular cemented stems: long-term follow-up. J Arthroplasty 22:100–105. https://doi.org/10.1016/j.arth.2007.03.025
Murray PB, Rand JA, Hanssen AD (1994) Cemented long-stem revision total knee arthroplasty. Clin Orthop Relat Res (309):116–123
Shannon BD, Klassen JF, Rand JA et al (2003) Revision total knee arthroplasty with cemented components and uncemented intramedullary stems. J Arthroplasty 18:27–32. https://doi.org/10.1016/S0883-5403(03)00301-2
Vince KG, Long W (1995) Revision knee arthroplasty. The limits of press fit medullary fixation. Clin Orthop Relat Res (317):172–177
Whaley AL, Trousdale RT, Rand JA, Hanssen AD (2003) Cemented long-stem revision total knee arthroplasty. J Arthroplasty 18:592–599. https://doi.org/10.1016/S0883-5403(03)00200-6
Fehring TK, Odum S, Olekson C et al (2003) Stem fixation in revision total knee arthroplasty: a comparative analysis. Clin Orthop Relat Res 416:217–224. https://doi.org/10.1097/01.blo.0000093032.56370.4b
Gehrke T, Kendoff D, Haasper C (2014) The role of hinges in primary total knee replacement. Bone Joint J 96-B:93–95. https://doi.org/10.1302/0301-620X.96B11.34143
Beksac B, Taveras NA, Della VAG, Salvati EA (2006) Surface finish mechanics explain different clinical survivorship of cemented femoral stems for total hip arthroplasty. J Long Term Eff Med Implants 16:407–422. https://doi.org/10.1615/JLongTermEffMedImplants.v16.i6.10
Crowninshield RD, Jennings JD, Laurent ML, Maloney WJ (1998) Cemented femoral component surface finish mechanics. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199810000-00010
Hernandez-Vaquero D, Garcia-Sandoval MA, Fernandez-Carreira JM, Gava R (2008) Influence of the tibial stem design on bone density after cemented total knee arthroplasty: a prospective seven-year follow-up study. Int Orthop 32:47–51. https://doi.org/10.1007/s00264-006-0280-y
Kutzner I, Heinlein B, Graichen F et al (2010) Loading of the knee joint during activities of daily living measured in vivo in five subjects. J Biomech 43:2164–2173. https://doi.org/10.1016/j.jbiomech.2010.03.046
Heinlein B, Kutzner I, Graichen F et al (2009) ESB clinical biomechanics award 2008: complete data of total knee replacement loading for level walking and stair climbing measured in vivo with a follow-up of 6–10 months. Clin Biomech 24:315–326. https://doi.org/10.1016/j.clinbiomech.2009.01.011
Levine D, Radha Manohar V (2019) Analysis of cemented stem extension for knee application. In: 50th Annu. Meet. Orthop. Res. Soc. pp 2–3
Lee SH, Shih HN, Chang CH et al (2020) Influence of extension stem length and diameter on clinical and radiographic outcomes of revision total knee arthroplasty. BMC Musculoskelet Disord 21:1–10. https://doi.org/10.1186/s12891-019-3030-1
Fleischman AN, Azboy I, Fuery M et al (2017) Effect of stem size and fixation method on mechanical failure after revision total knee arthroplasty. J Arthroplasty 32:S202–S208. https://doi.org/10.1016/j.arth.2017.04.055 (e1)
Conlisk N, Gray H, Pankaj P, Howie CR (2012) The influence of stem length and fixation on initial femoral component stability in revision total knee replacement. Bone Joint Res 1:281–288. https://doi.org/10.1302/2046-3758.111.2000107
Citak M, Levent A, Suero EM et al (2021) A novel radiological classification system of the distal femur. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03828-w
Levent A, Suero EM, Gehrke T, Citak M (2021) Risk factors for aseptic loosening after total knee arthroplasty with a rotating-hinge implant: a case-control study. J Bone Joint Surg Am 103:517–523. https://doi.org/10.2106/JBJS.20.00788
Gililland JM, Gaffney CJ, Odum SM et al (2014) Clinical and radiographic outcomes of cemented vs. diaphyseal engaging cementless stems in aseptic revision TKA. J Arthroplasty 29:224–228. https://doi.org/10.1016/j.arth.2014.03.049
Gill UN, Ahmed N, Noor SS et al (2020) Management of the bone loss by metaphyseal sleeves in primary and revision knee arthroplasty: clinical experience and outcome after forty three cases. Int Orthop 44:2315–2320. https://doi.org/10.1007/s00264-020-04663-1
Böhm P, Holy T (1998) Is there a future for hinged prostheses in primary total knee arthroplasty? A 20-year survivorship analysis of the Blauth prosthesis. J Bone Joint Surg Br 80:302–309. https://doi.org/10.1302/0301-620x.80b2.7905
Petrou G, Petrou H, Tilkeridis C et al (2004) Medium-term results with a primary cemented rotating-hinge total knee replacement. A 7- to 15-year follow-up. J Bone Jt Surg 86:813–817. https://doi.org/10.1302/0301-620X.86B6.14708
Howard JL, Kudera J, Lewallen DG, Hanssen AD (2011) Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Jt Surg 93:478–484. https://doi.org/10.2106/JBJS.I.01322
von Hintze J, Niemeläinen M, Sintonen H et al (2021) Outcomes of the rotating hinge knee in revision total knee arthroplasty with a median follow-up of 6.2 years. BMC Musculoskelet Disord 22:1–9. https://doi.org/10.1186/s12891-021-04205-9
Gurel R, Morgan S, Elbaz E et al (2021) Mid-term clinical and radiographic outcomes of porous-coated metaphyseal sleeves used in revision total knee arthroplasty. Knee Surg Relat Res 33:1–6. https://doi.org/10.1186/s43019-021-00103-5
Martin-Hernandez C, Floria-Arnal LJ, Muniesa-Herrero MP et al (2017) Mid-term results for metaphyseal sleeves in revision knee surgery. Knee Surg Sport Traumatol Arthrosc 25:3779–3785. https://doi.org/10.1007/s00167-016-4298-4
Barrack RL, Lyons TR, Ingraham RQ, Johnson JC (2000) The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty 15:858–866. https://doi.org/10.1054/arth.2000.9056
Bloch BV, Shannak OA, Palan J et al (2020) Metaphyseal sleeves in revision total knee arthroplasty provide reliable fixation and excellent medium to long-term implant survivorship. J Arthroplasty 35:495–499. https://doi.org/10.1016/j.arth.2019.09.027
Panda I, Wakde O, Singh H, Rajgopal A (2018) Management of large bone defects around the knee using porous tantalum trabecular metal cones during complex primary and revision total knee arthroplasty. Semin Arthroplast JSES 29:265–271. https://doi.org/10.1053/j.sart.2019.01.014
Siqueira MBP, Jacob P, McLaughlin J et al (2017) The varus-valgus constrained knee implant: survivorship and outcomes. J Knee Surg 30:484–492. https://doi.org/10.1055/s-0036-1593361
Springer BD, Sim FH, Hanssen AD, Lewallen DG (2004) The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000126306.87452.59
Efe T, Roessler PP, Heyse TJ et al (2012) Mid-term results after implantation of rotating-hinge knee prostheses: primary vs. revision. Orthop Rev (Pavia) 4:35. https://doi.org/10.4081/or.2012.e35
Villanueva-Martínez M, De la Torre-Escudero B, Rojo-Manaute JM et al (2013) Tantalum cones in revision total knee arthroplasty. A promising short-term result with 29 cones in 21 patients. J Arthroplasty 28:988–993. https://doi.org/10.1016/j.arth.2012.09.003
Lachiewicz PF, Bolognesi MP, Henderson RA et al (2012) Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res 470:199–204. https://doi.org/10.1007/s11999-011-1888-9
Abdelaziz H, Saleri S, Mau H et al (2019) Interprosthetic femoral sleeves in revision arthroplasty: a 20-year experience. J Arthroplasty 34:1423–1429. https://doi.org/10.1016/j.arth.2019.02.055
Funding
Open Access funding enabled and organized by Projekt DEAL. None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Obtained prior to beginning the study.
Informed consent
Not applied (anonymous retrospective data analysis).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maslaris, A., Tsiridis, E., Schoeneberg, C. et al. Does stem profile have an impact on the failure patterns in revision total knee arthroplasty?. Arch Orthop Trauma Surg 143, 1549–1569 (2023). https://doi.org/10.1007/s00402-022-04683-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04683-z