Abstract
Introduction
Trochanteric femoral fractures are among the most common operatively treated fractures. Intramedullary fixation has become the treatment of choice in many centers around the world. Nevertheless, the knowledge of rare complications of these fractures is limited. In this study, the incidence and treatment strategies for peri-implant fractures (PIF) were assessed.
Materials and methods
A single-center retrospective cohort study was done on 987 consecutive operatively treated trochanteric fractures. PFNA cephalomedullary nail was used as a fixation method. All patients were followed up from patient records for peri-implant fractures. Plain radiographs as well as different salvage methods were analyzed and compared.
Results
The total rate of peri-implant fractures was 1.4% (n = 14). The rate of PIF for patients treated with short (200 mm) nails, intermediate-length (240 mm) nails, and long nails was 2.7% (n = 2), 1.5% (n = 11), and 0.7% (n = 1), respectively (ns, p > 0.05 for difference). Treatment of choice for PIF was either ORIF with locking plate (57%, n = 8) or exchange nailing (43%, n = 6). None of the PIF patients needed additional surgeries for non-union, malunion, or delayed union.
Conclusions
A PIF is a rare complication of intramedullary fixation of trochanteric fractures. It can be treated with either locking plates or exchange nailing with sufficient results. There are no grounds for favoring long nails to avoid PIFs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trochanteric femoral fractures (AO 31-A) are one of the most common operatively treated fractures [1]. Hip fracture patients are usually elderly with multiple comorbidities, which presents a challenge for treatment. The treatment aims to restore mobility, and prevent institutionalization and increased mortality while avoiding reoperations and readmissions. Despite the high prevalence, there is still lacking evidence on the optimal treatment for these fractures [2,3,4,5]. An increasing trend toward the use of intramedullary nailing compared to sliding hip screws has been described [6].
With the increasing use of intramedullary nailing, problems regarding peri-implant fractures (PIFs) have been brought up. Although reported incidence for PIFs has been as high as 2.6% [7], no distinct guidelines have been established for the treatment of PIFs. Previous studies do not report outcomes of salvage operations done after PIF.
Previous reports suggest a high overall complication rate, where non-surgical complications such as delirium, anemia, electrolyte disturbances, pulmonary complications, and heart complications form the majority of complications [8, 9]. The most common reasons for reoperation after intramedullary fixation are surgical site infection, mal/non-union, and mechanical complications [10].
The aim of the study was to describe the incidence of a peri-implant fracture (PIF), compare the risk with short and long cephalomedullary nails, and describe the treatment and the treatment results of PIF.
Patients and methods
The study was a single-center retrospective analysis of 987 consecutive trochanteric fractures on 966 patients (AO/OTA 31-A), all treated with intramedullary nailing with Proximal Femoral Nail Antirotation (PFNA) intramedullary nail (DePuy Synthes, Raynham, Massachusetts, US). A short nail (200 mm) was used in 7.5% (n = 74), intermediate-length nail (240 mm) 74% (n = 728), and a long nail (300–420 mm) in 15% (n = 150) of the fractures. For 3.5% (n = 35), nail length was not defined in the charts, but could be deduced to be 200 mm or 240 mm. The patients were operated on in the years 2011–2016 and the follow-up from the patient records was for a minimum of 2 years after the operation or until death.
Initial operations were performed on a traction table according to AO principles [11] under fluoroscopy guidance. Open reduction was performed if sufficient reduction was not achieved with closed reduction methods. The nail length was defined according to the surgeon’s preference. In general, short nail was used for stable trochanteric fractures, intermediate-length or long nail was used for unstable trochanteric fractures, and long nail for subtrochanteric fractures. Distal locking screws were used in all patients. Cement augmentation was not used in any of the cases.
Patient database and radiological records were searched for each patient and reoperations for PIF or nail breakage were analyzed. We collected the patient demographic data, delay to surgery, and comorbidities (ASA class, use of anticoagulants, and other illnesses) (Table 1).
The differences in demographic and preoperative characteristics between the groups were tested using the Chi-square test or Student t test when appropriate. p values of < 0.05 were considered significant. The statistical program SPSS 25 (IBM Corp. released 2017. Armonk, NY: IBM Corp.) was used for analyzes.
The research was approved by the research committee in Helsinki University Hospital. As the study was a retrospective chart review without interaction with the patients, an ethical committee approval was not sought.
Results
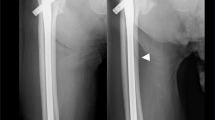
The total rate of PIF was 1.4% (n = 14). The median time to a PIF was 102 (6–896) days after initial trochanteric fracture surgery, and the median age of patients with a PIF was 90 (61–105) years (Table 1). The most common mechanism of injury was a fall from standing height or less (79%, n = 11) and the remainder (21%, n = 3) occurred without significant injuries and were classified as stress fractures. The most common site of fracture was at the distal tip of the nail (71%, n = 10), whereas two patients had PIF more proximally along with the nail and two patients distal to the nail (Figs. 1 and 2). All stress fractures occurred at the tip of the IM nail (Table 2).
The rate of PIF was 2.7% (n = 2) for patients treated with short 200 mm nails, 1.5% (n = 11) with intermediate-length 240 mm nails and 0.7% (n = 1) with long nails, respectively. The differences between groups were not statistically significant. All post-operative intramedullary nail breakages (n = 3, 2.1%) occurred after treatment with a long nail. These happened at 164, 174, and 282 days from the initial fracture surgery, respectively.
Treatment of choice for PIF was either fixation with a locking plate (n = 8, 57%) or exchange nailing (n = 6, 43%). The treatment strategy was defined based on fracture morphology and whether the initial fracture had healed. All nail breakages occurring after treatment with long nails happened by the hole for the blade (Fig. 3). These were treated with exchange nailing and with autogenic bone grafting from the iliac crest.
None of the patients needed additional surgeries for malunion, non-union, or delayed union after the initial surgery for the PIF. One patient had a post-operative surgical site infection after salvage treatment treated with a series of surgical debridements and intravenous antibiotics. The mortality after PIF was 7% at 30 and 90 days, 29% at 1 year, and 43% at 2 years. As a comparison, mortality after initial trochanteric fracture was 7% at 30 days, 14% at 90 days, 26% at 1 year, and 35% at 2 years, respectively.
The rate of blade cut-out was 2.7% (n = 2/74) for short nails, 1.2% (n = 9/728) for intermediate-length nails, and 1.3% (n = 2/150) for long nails. Overall, reoperation rate was 11% (n = 8/74) for short nails, 5.9% (n = 43/728) for intermediate-length nails, and 10% (n = 15/150) for long nails, respectively.
Discussion
The rate of PIF (1.4%) in our study was similar to earlier reports, with 1.6–2.1% reported for PFNA and 1.7% for all cephalomedullary nails together [7, 12]. Previously, Skala-Rosenbaum et al. reported an incidence of 2.0% (n = 17) for PIFs in their series of 849 trochanteric fractures treated with intermediate-length (240 mm) cephalomedullary nails [13]. However, 16 of the 17 PIFs occurred in patients with no distal locking screw. Compared to our material, distinctly more PIFs occurred by the intramedullary nail which is probably caused by the absence of the distal locking screw. The patients in their series were treated by inserting distal locking screw, exchange nailing, or plating, and all the patients healed without complications. This is parallel to our study where no additional surgeries were needed due to prolonged fracture healing, although one patient suffered a post-operative infection and had multiple revision surgeries.
We found a nonsignificant trend for fewer PIFs with long nails compared to intermediate-length and short nails (0.7% vs. 1.5% vs. 2.7%). However, this advantage is negated by the risk of nail breakage with long nails (2.1%). In addition, the length of surgery and the amount of bleeding are increased when using long nails compared to short nails [14]. Fortunately, PIFs and nail breakages were rare in both groups. We do not recommend the use of long cephalomedullary nails to reduce the risk for PIF, but rather to decide the fixation method on the basis of the fracture morphology.
In recent years, four different classifications have been proposed for PIFs after intramedullary fixation of proximal femoral fractures [13, 15,16,17]. All classifications take into account the fracture location, whereas some include a description of the PIF morphology and/or initial fracture healing. With the validation processes still in progress, the assistance for clinicians regarding choosing the treatment remains minor.
We hypothesize that nail breakage at the hole for the collum blade with PFNA occurs similarly to nail breakage with gamma nails and is caused by delayed union [18]. Increased and prolonged stress to the weakest point of the nail makes the nail break at a certain time point. Metallurgic and electronic microscope analysis by Dragosloveanu et al. suggests that this stress might be increased because of minor malalignment of the blade from multiple insertions of the guidewire for helical blade [19]. In our study, most PIFs occurred at the tip of the nail, suggesting that the stress point at that site defines the typical site of bone to fail.
The treatment of PIFs is challenging, as many of the patients had their PIF during the recovery period from the initial surgery. The treatment strategy is dependent on fracture morphology and whether the initial fracture has healed. In our material, both exchange nailing and locking plates yielded good results. The surgeon treating these complications should be comfortable to use both techniques as well as have the capability and instrumentation for implant removal.
The main limitation of the study is its retrospective nature without patient-reported outcomes. PIFs are rare and occur to elderly patients with multiple comorbidities. For statistical analysis to be possible, a large multicenter study would be needed.
Based on these single-center study outcomes, we suggest the following treatment protocol:
(1) if the original fracture has healed and a stable fixation can be achieved by nailing, the fracture should be treated with exchange nailing to a longer intramedullary nail
(2) When the healing of the original fracture is uncertain or a stable fixation is not considered possible with a nail, fixation with a locking plate is the treatment of choice
In conclusion, PIF is a rare complication after intramedullary nailing of trochanteric fracture. Depending on fracture morphology and healing of the initial fracture, both revision surgery with exchange nailing and locking plate osteosynthesis appear to be adequate treatment options.
References
Gromov K, Brix M, Kallemose T, Troelsen A (2014) Early results and future challenges of the danish fracture database. Dan Med J 61(6):A4851
Nyholm AM, Palm H, Malchau H, Troelsen A, Gromov K (2016) Lacking evidence for performance of implants used for proximal femoral fractures—a systematic review. Injury 47(3):586–594. https://doi.org/10.1016/j.injury.2016.01.001
Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR (2017) Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Jt J 99-B(1):128–133. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0134.R1
Nie B, Wu D, Yang Z, Liu Q (2017) Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: a meta-analysis. Medicine (Baltimore) 96(27):e7446. https://doi.org/10.1097/MD.0000000000007446
Sreekanta A, Eardley WG, Parker MJ et al (2019) Surgical interventions for treating extracapsular hip fractures in adults: A network meta-analysis. Cochrane Libr. https://doi.org/10.1002/14651858.CD013405
Werner BC, Fashandi AH, Gwathmey FW, Yarboro SR (2015) Trends in the management of intertrochanteric femur fractures in the united states 2005–2011. Hip Int 25(3):270–276. https://doi.org/10.5301/hipint.5000216
Norris R, Bhattacharjee D, Parker MJ (2011) Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: A systematic review of 13,568 patients. Injury 43(6):706–711. https://doi.org/10.1016/j.injury.2011.10.027
Saul D, Riekenberg J, Ammon JC, Hoffmann DB, Sehmisch S (2019) Hip fractures: therapy, timing, and complication spectrum. Orthop Surg 11(6):994–1002. https://doi.org/10.1111/os.12524
Flikweert ER, Wendt KW, Diercks RL et al (2017) Complications after hip fracture surgery: are they preventable? Eur J Trauma Emerg Surg 44(4):573–580. https://doi.org/10.1007/s00068-017-0826-2
Koval KJ (2007) Intramedullary nailing of proximal femur fractures. Am J Orthop (Belle Mead, NJ) 36(4 Suppl):4–7
Buckley RE, Moran CG, Apivatthakakul T (2017) AO principles of fracture management. Thieme Medical Publishers, New York
Müller F, Galler M, Zellner M, Bäuml C, Marzouk A, Füchtmeier B (2016) Peri-implant femoral fractures: the risk is more than three times higher within PFN compared with DHS. Injury 47(10):2189–2194. https://doi.org/10.1016/j.injury.2016.04.042
Skála-Rosenbaum J, Džupa V, Bartoška R, Douša P, Waldauf P, Krbec M (2016) Distal locking in short hip nails: cause or prevention of peri-implant fractures? Injury 47(4):887–892. https://doi.org/10.1016/j.injury.2016.02.009
Dunn J, Kusnezov N, Bader J, Waterman B, Orr J, Belmont P (2016) Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): a systematic review. J Orthop Traumatol 17(4):361–367. https://doi.org/10.1007/s10195-016-0405-z
Toro G, Moretti A, Ambrosio D et al (2021) Fractures around trochanteric nails: the “Vergilius classification system.” Adv Orthop. https://doi.org/10.1155/2021/7532583
Videla-Cés M, Sales-Pérez J, Sánchez-Navés R, Romero-Pijoan E, Videla S (2019) Proposal for the classification of peri-implant femoral fractures: retrospective cohort study. Injury 50(3):758–763. https://doi.org/10.1016/j.injury.2018.10.042
Chan L, Gardner A, Wong M, Chua K, Kwek E (2018) Non-prosthetic peri-implant fractures: classification, management and outcomes. Arch Orthop Trauma Surg 138(6):791–802. https://doi.org/10.1007/s00402-018-2905-1
Johnson NA, Uzoigwe C, Venkatesan M et al (2017) Risk factors for intramedullary nail breakage in proximal femoral fractures: a 10-year retrospective review. Ann R Coll Surg Engl 99(2):145–150. https://doi.org/10.1308/rcsann.2016.0297
Dragosloveanu Ş, Dragosloveanu CDM, Stanca HT, Cotor DC, Dragosloveanu CI, Stoica CI (2020) A new perspective toward failure of gamma nail systems. Exp Ther Med 20(6):216. https://doi.org/10.3892/etm.2020.9346
Funding
Open access funding provided by University of Helsinki including Helsinki University Central Hospital. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest. There was no financial support for the research. No writing aid obtained.
Ethical approval
The research was approved by the research committee in Helsinki University Hospital. As the study was a retrospective chart review without interaction with the patients, an ethical committee approval was not sought.
Informed consent
Informed consent was not obtained, because the study was a retrospective chart review without interaction with the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Halonen, L.M., Stenroos, A., Vasara, H. et al. Peri-implant fracture: a rare complication after intramedullary fixation of trochanteric femoral fracture. Arch Orthop Trauma Surg 142, 3715–3720 (2022). https://doi.org/10.1007/s00402-021-04193-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04193-4