Abstract
Introduction
The Olympia femoral stem is a stainless steel, anatomically shaped, polished and three-dimensionally tapered implant designed for use in cemented total hip arthroplasty (THA). The primary aim of this study was to determine the long-term survivorship, radiographic outcome, and patient-reported outcome measures (PROMs) of the Olympia stem.
Patients and methods
Between May 2003 and December 2005, 239 patients (264 THAs) underwent a THA with an Olympia stem in our institution. Patient-reported outcome measures were assessed using the Oxford Hip Score (OHS), EuroQol-5 dimensions (EQ-5D) score, and patient satisfaction at mean 10 years following THA. Patient records and radiographs were then reviewed at a mean of 16.5 years (SD 0.7, 15.3–17.8) following THA to identify occurrence of complications or revision surgery for any cause following surgery. Radiographs were assessed for lucent lines and lysis according to Gruen’s zones
Results
Mean patient age at surgery was 68.0 years (SD 10.9, 31–93 years). There were 156 women (65%, 176 THAs). Osteoarthritis was the indication for THA in 204 patients (85%). All cause stem survivorship at 10 years was 99.2% (95% confidence interval [CI], 97.9%–100%) and at 15 years was 97.5% (94.6%–100%). The 15-year stem survival for aseptic loosening was 100%. Analysis of all-cause THA failure demonstrated a survivorship of 98.5% (96.3%–100%) at 10 years and 95.9% (92.4%–99.4%) at 15 years. There were 9 THAs with non-progressive lucent lines in a single Gruen zone and 3 had lines in two zones, and no patient demonstrated signs for lysis. At a mean of 10-year (SD 0.8, 8.7–11.3) follow-up, mean OHS was 39 (SD 10.3, range 7–48) and 94% of patients reported being very satisfied or satisfied with their THA.
Conclusions
The Olympia stem demonstrated excellent 10-year PROMs and very high rates of stem survivorship at final follow-up beyond 15 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excellent long-term outcomes have been demonstrated for cemented total hip arthroplasty (THA) performed with a variety of different femoral stem designs [1,2,3]. Whilst the majority of modern femoral stem designs are straight, normal femoral anatomy is curved when viewed in the coronal plane [4]. This mismatch predisposes to a recognized pattern of sagittal plane implant malalignment within the femoral canal, which results in a variation in the cement mantle thickness around the implant [5, 6].
To counter this, sided anatomic stems have been developed including the Olympia femoral stem (Biomet UK Ltd.). The Olympia is a stainless steel, highly polished, three-dimensionally (3D) tapered femoral stem with an anatomic shape in two plains (Fig. 1). Compared to straight stemmed designs such as the Exeter (Stryker Orthopaedics, Mahwah, NJ), anatomic stems are more reliable at producing a centralized and anatomical position within the femoral canal and maintaining a consistent cement mantle thickness around the implant [5, 7, 8]. Ultimately, this reduces the risk of cement mantle deficiency that can be associated with osteolysis and potential periprosthetic fracture [5, 7,8,9]. The Olympia has a number of other features aimed at maintaining cement mantle integrity. Tensile stresses and abrasion at the cement mantle are reduced by a highly polished stem surface (Ra 10 nm). A smooth cross-sectional design containing no edges further minimizes stress risers within the cement mantle. The 3D taper includes an oval metaphyseal section to improve rotational stability and implant centralization. A double reduced taper aims to limit subsidence, whilst a natural anteversion is built into the 3D design that mirrors the native femur [10].
Orthogonal views of the Olympia stem, demonstrating anatomical shape in both planes [10]
There has been one mid-term study of the Olympia stem at 9 years with overall survival for aseptic loosening reported at 100%. However, there are limited published data on the survival and functional outcome of the stem after 10 years [10]. The aims of this study were to investigate the long-term survivorship (minimum of 15 years), radiographic outcome, and the associated patient-reported outcomes of the Olympia femoral stem in patients who underwent a primary total hip arthroplasty (THA).
Patients and methods
Between May 2003 and December 2005, 264 consecutive primary THAs (239 patients) incorporating an Olympia stem were performed or supervised by the same surgeon within our institution. These patients were identified from a prospectively compiled arthroplasty patient database. In those who had received bilateral THAs, at least 6 months were required between consecutive operations for each THA to be analysed individually. If the time between THA operations in an individual patient was less than 6 months, PROMs were only sampled at follow-up from the last procedure performed to minimize the impact of surgical recovery from a contralateral THA on PROMs [11]. Two THAs were excluded as a result. No bilateral THAs performed simultaneously were included in this study.
Patient demographics and indication for THA were recorded and The Scottish Index of Multiple Deprivation used to assign social deprivation scores to patients based on postcode. The SIMD ranks geographic areas based on seven domains: income, employment, education, housing, health, crime, and geographical access. Data zones are defined by postcodes and once ranked nationally are divided into population-weighted quintiles with 1 representing the most deprived and 5 the least deprived [12].
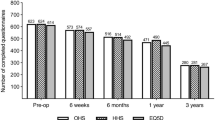
Post-operative questionnaires including the following patient-reported outcome measures (PROMs) were sent to patients at a mean of 10.0 years (SD 0.8, 8.8–11.3) following THA: Oxford Hip Score (OHS), the EuroQol-5 dimensions (EQ-5D) score, and satisfaction scores. The OHS is a validated hip-specific outcome measure of 12 questions with five possible answers giving a score of between 0 and 48 [13]. Higher scores represent better function. The EQ-5D evaluates five domains of general health (mobility, self-care, usual activities, pain, and anxiety) and in addition a visual analogue scale (VAS) for general health [from 0 (worst) to 100 (best)] [14]. Pain was also assessed using a VAS [from 0 (worst) to 100 (best)]. Patient satisfaction was recorded by asking the patient “How satisfied are you with your hip?” The answer was documented using a 5-point Likert scale: very satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, or very dissatisfied [15]. Patients were also asked in the questionnaire “Have you had any further surgery on or complications with the joint in question?” All patient notes and radiographs were reviewed again at a final mean of 16.5 years (SD 0.7, 15.3 to 17.8) following THA to examine for occurrence of any complications or surgery having occurred at any time following primary THA.
Radiographic analysis was performed on radiographs taken in the immediate post-operative period and during longer term follow-up as part of routine and unscheduled clinical follow-up. All radiographs were reviewed by a consultant radiologist and checked by a senior author or orthopaedic specialty trainee using PACS software and interpreted using the Gruen grading system [19]. Patients were searched on a national radiographic database at a mean of 16.5 years (SD 0.7, 15.3–17.8) following surgery to ensure that the results of the most recently available radiographs were included. Final radiographs included in the analysis were taken at a mean of 11.6 years following surgery (SD 3.3, 5 to 17.3).
Surgical technique
All patients underwent surgery in a lateral decubitus position; an anterolateral or Modified Hardinge approach was used in all cases except one where a posterior approach was performed. After broaching and lavage of the femur, an Exeter cement restrictor was inserted. A third-generation cementing technique was performed involving pulsatile jet lavage, retrograde cement application, and 3-phase pressurization before Olympia stem insertion. A similar technique was used to implant a cemented acetabular component. Three cups were used, namely the Exeter Contemporary Flanged (CF) cup, the Hooded Exeter Low Profile (LP) cup, and the Charnley® Ogee Cup. All of the implants were fixed with Palacos R & G cement (Heraeus Kulzer GmbH; Heraeus Medical GmbH) with the exception of 3 patients who underwent THA with autogenous floor graft whose implants were fixed with Refobacin Palacos R (Heraeus Kulzer GmbH; Biomet Europe). THAs were routinely metal on polyethylene except for 2 that were ceramic on polyethylene. Each patient was administered 3 doses of antibiotics (1 dose preoperatively and 2 postoperatively) and DVT prophylaxis postoperatively.
Statistical analysis
This was performed using Statistical Package for Social Sciences version 27.0 (SPSS Inc., Chicago, Illinois). Univariate analysis was performed using parametric (Student’s t test: paired and unpaired) and non-parametric (Mann–Whitney U test) tests, as appropriate, to assess continuous variables for significant differences between two groups. One-way analysis of variance (ANOVA) was used to compare continuous variables with multiple groups (OHS in Carstairs groups). Nominal categorical variables were assessed using a Chi-squared or Fisher’s exact test (if frequency less than 5 in one cell). Pearson’s correlation or Spearman’s rank correlation was used to assess the relationship between linear variables as appropriate. The Kaplan–Meier method was used to estimate the survival of the prosthesis. A p value of < 0.05 was considered significant in all analyses.
Ethical approval was obtained for this study. Collection of data was independent of the routine clinical care of the patient. Whilst the lead author was involved in developing the prospective database and original implant design, he remained independent from the process of data evaluation and manuscript preparation to exclude any potential source of bias.
Results
Patient demographics
Mean patient age at surgery was 68.0 years (SD 10.9, 31–93 years). There were 156 women (65%, 176 THAs). Osteoarthritis was the indication for THA in 204 patients (85%), rheumatoid arthritis in 14 patients (6%), and other diagnoses in 21 patients (9%). The mean body mass index (BMI) was 28.6 kg/m2 (range 17 to 45). Surgical implant variables are detailed in Table 1. At a mean of 10-year (range 6.4 -11.3) follow-up, there were 157 patients alive (66%, n = 157/239, 176 THAs) with 82 patients (34%, n = 82/239, 88 THAs) having died of unrelated causes. At a mean of 16.5-year (SD 0.7, 15.3 to 17.8) follow-up, there were 90 patients alive (38%, n = 90/239, 94 THAs) with 149 patients (62%, n = 149/239, 170 THAs) having died of unrelated causes.
Implant survival and patient experience of complications
At a mean 16.5-year (SD 0.7, 15.3 to 17.8) follow-up, there were five revisions (5/264, 1.9%) in total. All-cause stem survivorship at 10 years was 99.2% (95% confidence interval [CI], 97.9%-100%) and at 15 years was 97.5% (95% CI 94.6%–100%) (Fig. 2A). The 15-year stem survival for aseptic loosening was 100%. Analysis of all-cause THA failure demonstrated a survivorship of 98.5% (95% confidence interval [CI], 96.3%–100%) at 10 years and 95.9% (95% CI 92.4%–99.4%) at 15 years (Fig. 2B). The 10-year survival for the end-point of re-operation for any reason was 98.1% (95% CI 97.3%–98.9%), and at 15 years, this was 91.7% (95% CI 91.2%–92.2%). Dislocation rate at 15 years was 0%, with no episodes identified on patient notes, radiographs, or on patient-reported feedback.
Overall, two patients underwent revision for persistent deep infection; one patient underwent single-stage revision at 1 year following surgery, whilst the second patient underwent single-stage revision 13 years following THA. In both cases, revision was successful with no further surgery required and an infecting organism identified prior to revision. One patient sustained an atypical periprosthetic fracture requiring ORIF 13 years following index THA, related to bisphosphonate usage with clear antecedent symptoms and radiographic changes identified prior to development of periprosthetic fracture (Fig. 3). Two acetabular revisions were performed; one for aseptic loosening that developed following a heavy mechanical fall, with no stem revision required at 12 years following index THA; a further acetabular revision for aseptic loosening and implant migration was performed 11 years following index THA with cement-in-cement stem revision (original stem not found to have developed aseptic loosening) also performed.
Complications and reoperations were found to occur following 10 THAs with patient experience of complications detailed in Table 2. However, the majority of complications and reoperations (6/10, 60%) occurred more than 1 year following surgery.
Radiological analysis
There were radiographs available for 202 of the 239 patients (224 THAs) with final radiographs taken at a mean of 11.6 years following surgery (SD 3.3, 5–17.3) (Example in Fig. 4). Radiographs were not available for 37 patients (40 THAs) who died before routine follow-up or prior to the adoption of digitised radiographs in our institution. A total of 171 (77%) THA radiographs were reported as normal, whilst abnormalities were reported in the remaining 53 (23%) THAs as detailed in Table 3. Only 12 (5%) of the stems had lucent lines, all of which were non-progressive and noted to be clinically asymptomatic during clinical follow-up (Table 3). No stem demonstrated significant signs of lysis (lucent line > 2 mm). Analysis of immediate post-operative radiographs also found Barrack grade A cement mantles in all cases.
Patient satisfaction and functional outcome at 10 years
At a mean of 10-year (SD 0.8, range 8.7–11.3) follow-up, postal questionnaires were returned by 117 patients (76%) that underwent 134 THAs. 94% of patients reported being very satisfied or satisfied with their THA. Furthermore, 84% of patients were likely or extremely likely to be willing to undergo the same operation if needed at follow-up. Only two patients reported dissatisfaction, with the remaining 4% of patients neither satisfied nor dissatisfied with their THA at long-term follow-up. Patient age at surgery (p = 0.530), deprivation level (p = 0.355), and gender (p = 0.544) had no impact on satisfaction levels. However, patient experience of complications (p = 0.023, odds ratio [OR] 5.69, 95% CI 1.47–21.4) and a BMI ≥ 35 kg m−2 (p = 0.007, OR 1.55, 95% CI 1.06–2.66) were both associated with an increased risk of dissatisfaction.
The mean OHS reported was 39 (SD 10.3, 7–48). There were no correlations found between OHS and patient age (p = 0.275), gender (p = 0.889), BMI (p = 0.197), femoral stem size (p = 0 0.601), or head size (p = 0 0.724). However, a higher deprivation level (SIMD decile < 5) was associated with a significantly lower OHS, EQ-5D index, and inferior pain scores at follow-up (Table 4). Patients that experienced complications also reported a significantly lower OHS at follow-up (39.6 SD 10.6 v 30.5 SD 7.5, p = 0.018) and lower EQ-5D index score (0.84 SD 0.15 v 0.65 SD 0.09 p < 0.001). However, EQ-5D health (p = 0.73) and pain (p = 0.34) scores were not impacted by experience of complications or patient BMI (p > 0.05). Patients with a lower OHS were more likely to report lower satisfaction ratings at follow-up (r = 0.517, p < 0.001).
Discussion
The overall survival rate for the Olympia stem was excellent at a mean of 15-year follow-up, with high patient satisfaction levels and excellent OHS also demonstrated at a mean of 10 years. Survivorship, with revision of the stem for aseptic loosening as the end-point, was 100% at 15 years. Overall survival to revision for any reason was above 98% at 10 years and 96% at 15 years. There was a low rate of non-progressive radiolucent lines, with no cases of lysis, around the stem which supports continued longevity in the future. In addition, the stem when used as part of a THA was associated with excellent PROMs and high patient satisfaction, which was achieved irrespective of patient gender, age at operation, or BMI; however, social deprivation and complications were associated with lower PROMs.
A recent study reported the survival rate for all-cause revision of the Exeter™ stem (Stryker, Newbury UK) to be 91.2% at 13.5 years [16]. A further review reported Exeter stem 10-year survival rate at 97.8% for all-cause revision and 98.9% for aseptic loosening, with a mean OHS of 36 [17]. In a radiological analysis of the Olympia, we found that 6% of patients had signs of femoral demarcation at 10-year follow-up. In an analysis of the Exeter stem at a mean of 12.7 years, Hook et al. reported defects of the cement mantle (Barrack grade C and D) in 28% of stems and a revision rate for aseptic loosening and osteolysis of 1.1% [17]. The Olympia stem appears to compare favourably to the Exeter in terms of both revision rate and functional outcome measured by the OHS. When compared to another anatomic stem design, such as the Lubinus SP II® (Link, Hamburg, Germany), results were again favourable, with all-cause 10-year survival of the Lubinus SP II® reported as 98.3% [18].
The low incidence of periprosthetic fracture (PPF) demonstrated with the Olympia stem is particularly significant, with only one revision performed in this study, in a patient that developed the recognized phenomenon of an atypical PPF related to bisphosphonate usage [19]. Revision rates for PPF in straight stems such as the Exeter have been reported to be higher at 2.3% [20] and 1.5% for the updated Exeter V40 stem at 10 years [16]. The PPF rate of the Exeter was recently compared to another anatomic stem, the Lubinus SP II® (Link, Hamburg, Germany), and found to be ten times higher [21]. Minimizing the risk of PPF in patients has large clinical and socioeconomic implications. Patients revised for PPF display poor functional outcomes scores, often require resource intensive clinical management, and have a similar mortality rates when compared to neck of femur fracture patients up to 6 months post-injury and a reported 1-year mortality rate of 9.7% [22]. Future projections suggest that the number of periprosthetic fractures is expected to increase by 4.6% every decade over the next 30 years [23]. In this context, increased use of anatomic stems therefore seems a wise investment.
Socioeconomic status has previously been shown to negatively affect the functional outcome of primary and revision THA, at a national level and within our local population, with inferior joint-specific and health scores demonstrated [22, 24, 25]. In this respect, the Olympia stem appeared to have a similar outcome, with significantly lower OHS, EQ-5D index scores and increased pain scores reported in patients with increased social deprivation. However, deprivation level did not affect satisfaction at long-term follow-up. The Olympia stem appeared to perform equally well regardless of patient age or gender. Patient BMI also had limited impact on outcome within the confines of our study, with OHS, EQ-5D pain scores, and implant survivorship unaffected at follow-up. However, patients with a BMI ≥ 35 were on average “satisfied,” whereas patients with a BMI ≤ 35 were on average “very satisfied.” Conflicting reports exist regarding the effect of obesity on outcomes following primary THA, with some studies suggesting that high BMI limits post-operative function and satisfaction, and increases revision and complication rates [26].
The complication rate was low, with 1.7% of patients experiencing a complication or re-operation within 12 months of their THA. This compares favourably to the literature, with 3% of patients expected to experience a significant medical complication and 7.5% of patients reported to experience a significant surgical complication following THA [27]. Nevertheless, at 10-year follow-up patients that experienced a complication continued to report significantly lower OHS and EQ-5D index scores and were less likely to be satisfied with their operation.
No episodes of dislocation following THA were identified at 15-year follow-up, despite a detailed search of patient notes, radiographs, and a patient-reported questionnaire. This again compares favourably to the literature, with a meta-analysis of over 13 000 primary THAs and minimum 12-month follow-up reporting a dislocation rate of 3.23% for the posterior approach and 2.18% for the anterolateral approach [28].
There are some limitations to our findings. Radiographic analysis was incomplete as reported radiographs were not available for all patients. Patient-reported outcomes were performed at 10 years and not repeated at 15 years which may limit their findings. There are also inherent limitations to postal questionnaires. Preoperative PROMS were also not routinely collected or available from our institution prior to 2006 and so were not available for comparison. A number of patients were also lost to death. Surgical implantation was supervised or performed by a single experienced surgeon in a high-volume arthroplasty centre, potentially limiting external validity of results. Furthermore, survivorship analysis was performed on a relatively small number of implants when compared to that available for stems used in higher volume such as the Exeter stem [2,3,4].
The Olympia stem was demonstrated to be associated with an excellent 15-year survivorship. When revision of the stem for aseptic loosening is considered, 15-year survivorship is 100%. This survival rate is supported by the low rate of non-progressive radiolucent lines, with no cases of lysis, and indicates continued longevity of the stem. PROMs were excellent and compare favourably to other commonly used implants. Furthermore, it has a negligible rate of PPF compared to other polished taper slip stems, which should promote continued use of the implant in future as the clinical burden of PPFs continues to increase.
References
López-López JA, Humphriss RL, Beswick AD, Thom HHZ, Hunt LP, Burston A et al (2017) Choice of implant combinations in total hip replacement: systematic review and network meta-analysis. BMJ 359:j4651
Association AO (2017) Australian orthopaedic association national joint registry annual report. Adelaide, Australia
Etkin CD, Springer BD (2017) The american joint replacement registry-the first 5 years. Arthroplast Today 3:67–69
Lidgren L, Robertsson O, W-Dahl A, Sundberg M (2017) The Swedish arthroplasty register—annual report. Lund University, Lund
Breusch SJ, Lukoschek M, Kreutzer J, Brocai D, Gruen TA (2001) Dependency of cement mantle thickness on femoral stem design and centralizer. J Arthroplast 16:648–657
Garellick G, Malchau H, Regnér H, Herberts P (1999) The Charnley versus the spectron hip prosthesis: radiographic evaluation of a randomized, prospective study of 2 different hip implants. J Arthroplast 14:414–425
Hank C, Schneider M, Achary CS, Smith L, Breusch SJ (2010) Anatomic stem design reduces risk of thin cement mantles in primary hip replacement. Arch Orthop Trauma Surg 130:17–22
Crawford RW, Psychoyios V, Gie G, Ling R, Murray D (1999) Incomplete cement mantles in the sagittal femoral plane: an anatomical explanation. Acta Orthop Scand 70:596–598
Breusch SJ, Draenert Y, Draenert K (1998) Anatomic basis of the cemented femur shaft. A comparative study of straight and anatomic design. Z Orthop Grenzgeb 136:554–559
Avasthi A, Goyal S, Taylor LJ (2011) THE OLYMPIA – A TAPERED, POLISHED ANATOMIC CEMENTED FEMORAL PROSTHESIS: 10 YEAR RESULTS. Orthop Proc 93-B:304
Judge A, Arden NK, Kiran A, Price A, Javaid MK, Beard D et al (2012) Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Jt Surg Br vol 94:412–418
Government TS (2020) The Scottish index of multiple deprivation. The Scottish Government
Dawson J, Fitzpatrick R, Carr A, Murray D (1996) Questionnaire on the perceptions of patients about total hip replacement. J Bone Jt Surg Br Vol 78:185–190
EuroQol Group (1990) A new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Likert R (1932) A technique for the measurement of attitudes. Archives of psychology. The Science Press, New York
Westerman RW, Whitehouse SL, Hubble MJW, Timperley AJ, Howell JR, Wilson MJ (2018) The Exeter V40 cemented femoral component at a minimum 10-year follow-up: the first 540 cases. Bone Jt J 100-B:1002–1009
Hook S, Moulder E, Yates PJ, Burston BJ, Whitley E, Bannister GC (2006) The Exeter universal stem: a minimum ten-year review from an independent centre. J Bone Jt Surg Br Vol 88:1584–1590
Prins W, Meijer R, Kollen BJ, Verheyen CC, Ettema HB (2014) Excellent results with the cemented Lubinus SP II 130-mm femoral stem at 10 years of follow-up: 932 hips followed for 5–15 years. Acta Orthop 85:276–279
MacKenzie SA, Ng RT, Snowden G, Powell-Bowns MFR, Duckworth AD, Scott CEH (2019) Periprosthetic atypical femoral fractures exist and are associated with duration of bisphosphonate therapy. Bone Jt J 101-B:1285–1291
Inngul C, Enocson A (2015) Postoperative periprosthetic fractures in patients with an Exeter stem due to a femoral neck fracture: cumulative incidence and surgical outcome. Int Orthop 39:1683–1688
Chatziagorou G, Lindahl H, Kärrholm J (2019) The design of the cemented stem influences the risk of Vancouver type B fractures, but not of type C: an analysis of 82,837 Lubinus SPII and Exeter polished stems. Acta Orthop 90:135–142
Turnbull GS, Scott CEH, MacDonald DJ, Breusch SJ (2018) Return to activity following revision total hip arthroplasty. Arch Orthop Trauma Surg 139:411
Pivec R, Issa K, Kapadia BH, Cherian JJ, Maheshwari AV, Bonutti PM et al (2015) Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implant 25:269–275
Clement ND, Jenkins PJ, MacDonald D, Nie YX, Patton JT, Breusch SJ et al (2013) Socioeconomic status affects the Oxford knee score and short-form 12 score following total knee replacement. The bone & joint journal. 95-B:52–58
Turnbull GS, Scott CEH, MacDonald DJ, Breusch SJ (2019) Gender and preoperative function predict physical activity levels after revision total knee arthroplasty. J Arthroplast 34:939–946
Liu W, Wahafu T, Cheng M, Cheng T, Zhang Y, Zhang X (2015) The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. Orthop Traumatol Surg Res 101:289–296
Aggarwal VK, Elbuluk A, Dundon J, Herrero C, Hernandez C, Vigdorchik JM et al (2019) Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Jt J 101-B:646–651
Masonis JL, Bourne RB (2002) Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Related Res 405:46–53
Funding
No funding was received to perform this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Whilst an author of the manuscript was involved in developing the local prospective arthroplasty database and original Olympia implant design, they remained independent from the process of data evaluation and manuscript preparation to exclude any potential source of bias.
Ethical approval
Local ethical approval was obtained for this study.
Informed consent
Patients included in the study gave informed consent to collection of their data and analysis of radiographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Turnbull, G.S., Marshall, C., Nicholson, J.A. et al. The Olympia anatomic polished cemented stem is associated with a high survivorship, excellent hip-specific functional outcome, and high satisfaction levels: follow-up of 239 consecutive patients beyond 15 years. Arch Orthop Trauma Surg 142, 2361–2370 (2022). https://doi.org/10.1007/s00402-021-03992-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03992-z