Abstract
Purpose
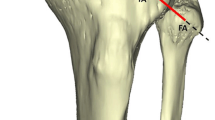
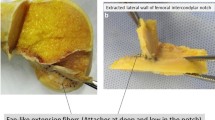
Kaplan fibers (KF) have been described as connections between the iliotibial band and the distal femur. They are divided into two distinct structures, proximal (PKF) and distal (DKF) fibers, which may participate in the control of the rotatory knee stability. Their anatomical characteristics have not been investigated completely, in particular with respect to reconstruction procedures. The aim was to determine their anatomical characteristics and their morphological variation.
Methods
Twenty-one nonpaired fresh frozen human cadaveric knees (from whole leg) were used for the analysis of PKF and DKF through an anterolateral approach. The anatomical relationships between the adjacent anterolateral structures were reported and anatomical characteristics of PKF and DKF (thickness, width and length) measured at 50° knee flexion under different rotational conditions (neutral: NR, Internal at 5Nm: IR applied with a dynamometric torque rig). Bony ridges of PKF and DKF were measured.
Results
PKF and DKF and their respective bony ridges were individually identified in all knees studied (n = 21). The PKF and DKF were proximal and posterior to the lateral femoral epicondyle, respective distances 49.20 ± 7.38 and 27.54 ± 7.69 mm. DKF were thicker (p < 0.001), wider (p < 0.001) and longer (p < 0.001) than the PKF, regardless of the tibial rotation applied. Tensioning of KF was achieved in IR with a decrease in thickness and width, alongside fiber lengthening (p < 0.001).
Conclusion
PKF and DKF are distinct and constant anatomical structures of the lateral compartment of the knee, whose anatomical characteristics and their tensioning in IR presume a function of controlling rotational knee stability.





Similar content being viewed by others
References
Geeslin AG, Chahla J, Moatshe G et al (2018) anterolateral knee extra-articular stabilizers: a robotic sectioning study of the anterolateral ligament and distal iliotibial band Kaplan fibers. Am J Sports Med 46:1352–1361. https://doi.org/10.1177/0363546518759053
Leys T, Salmon L, Waller A et al (2012) Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med 40:595–605. https://doi.org/10.1177/0363546511430375
Stensbirk F, Thorborg K, Konradsen L et al (2014) Iliotibial band autograft versus bone-patella-tendon-bone autograft, a possible alternative for ACL reconstruction: a 15-year prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 22:2094–2101. https://doi.org/10.1007/s00167-013-2630-9
Mouarbes D, Menetrey J, Marot V et al (2019) Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar Tendon-bone and hamstring-tendon autografts. Am J Sports Med 47:3531–3540. https://doi.org/10.1177/0363546518825340
Oh J-Y, Kim K-T, Park Y-J et al (2020) Biomechanical comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction: a meta-analysis. Knee Surg Relat Res 32:14. https://doi.org/10.1186/s43019-020-00033-8
Sonnery-Cottet B, Thaunat M, Freychet B et al (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43:1598–1605. https://doi.org/10.1177/0363546515571571
Jonsson H, Riklund-Ahlström K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75:594–599. https://doi.org/10.1080/00016470410001484
Slette EL, Mikula JD, Schon JM et al (2016) biomechanical results of lateral extra-articular tenodesis procedures of the knee: a systematic review. Arthroscopy 32:2592–2611. https://doi.org/10.1016/j.arthro.2016.04.028
Grassi A, Zicaro JP, Costa-Paz M et al (2020) Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg Sports Traumatol Arthrosc 28:418–431. https://doi.org/10.1007/s00167-019-05625-w
Getgood AMJ, Bryant DM, Litchfield R et al (2020) Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the stability study randomized clinical trial. Am J Sports Med 48:285–297. https://doi.org/10.1177/0363546519896333
Sonnery-Cottet B, Daggett M, Fayard J-M et al (2017) Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament—deficient knee. J Orthop Traumatol 18:91–106. https://doi.org/10.1007/s10195-017-0449-8
Claes S, Vereecke E, Maes M et al (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328. https://doi.org/10.1111/joa.12087
Ueki H, Katagiri H, Otabe K et al (2019) Contribution of additional anterolateral structure augmentation to controlling pivot shift in anterior cruciate ligament reconstruction. Am J Sports Med 47:2093–2101. https://doi.org/10.1177/0363546519854101
Chahla J, Menge TJ, Mitchell JJ et al (2016) Anterolateral ligament reconstruction technique: an anatomic-based approach. Arthrosc Tech 5:e453–e457. https://doi.org/10.1016/j.eats.2016.01.032
Lutz C (2018) Role of anterolateral reconstruction in patients undergoing anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res 104:S47–S53. https://doi.org/10.1016/j.otsr.2017.03.031
Landreau P, Catteeuw A, Hamie F et al (2019) Anatomic study and reanalysis of the nomenclature of the anterolateral complex of the knee focusing on the distal iliotibial band: identification and description of the condylar strap. Orthop J Sports Med 7:2325967118818064. https://doi.org/10.1177/2325967118818064
Ra HJ, Kim J-H, Lee D-H (2020) Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: systematic review and meta-analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03393-8
Kaplan EB (1958) The iliotibial tract; clinical and morphological significance. J Bone Joint Surg Am 40A:817–832
Godin JA, Chahla J, Moatshe G et al (2017) A comprehensive reanalysis of the distal iliotibial band: quantitative anatomy, radiographic markers, and biomechanical properties. Am J Sports Med 45:2595–2603. https://doi.org/10.1177/0363546517707961
Herbst E, Albers M, Burnham JM et al (2017) The anterolateral complex of the knee. Orthop J Sports Med 5:2325967117730805. https://doi.org/10.1177/2325967117730805
Getgood A, Brown C, Lording T et al (2018) The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5072-6
Musahl V, Herbst E, Burnham JM, Fu FH (2018) The anterolateral complex and anterolateral ligament of the knee. J Am Acad Orthop Surg 26:261–267. https://doi.org/10.5435/JAAOS-D-16-00758
Kittl C, El-Daou H, Athwal KK et al (2016) The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med 44:345–354. https://doi.org/10.1177/0363546515614312
Arnout N, Myncke J, Vanlauwe J et al (2013) The influence of freezing on the tensile strength of tendon grafts: a biomechanical study. Acta Orthop Belg 79:435–443
Lutz C, Sonnery-Cottet B, Niglis L et al (2015) Behavior of the anterolateral structures of the knee during internal rotation. Orthop Traumatol Surg Res 101:523–528. https://doi.org/10.1016/j.otsr.2015.04.007
Neri T, Testa R, Laurendon L et al (2019) Determining the change in length of the anterolateral ligament during knee motion: a three-dimensional optoelectronic analysis. Clin Biomech (Bristol, Avon) 62:86–92. https://doi.org/10.1016/j.clinbiomech.2019.01.006
Kennedy MI, LaPrade CM, Geeslin AG, LaPrade RF (2018) An overview of clinically relevant biomechanics of the anterolateral structures of the knee. Tech Orthop 33:213–218. https://doi.org/10.1097/BTO.0000000000000300
Avin KG, Bloomfield SA, Gross TS, Warden SJ (2015) Biomechanical aspects of the muscle-bone interaction. Curr Osteoporos Rep 13:1–8. https://doi.org/10.1007/s11914-014-0244-x
Batty L, Murgier J, O’Sullivan R et al (2019) The Kaplan fibers of the iliotibial band can be identified on routine knee magnetic resonance imaging. Am J Sports Med 47:2895–2903. https://doi.org/10.1177/0363546519868219
Van Dyck P, De Smet E, Roelant E et al (2019) Assessment of anterolateral complex injuries by magnetic resonance imaging in patients with acute rupture of the anterior cruciate ligament. Arthrosc J Arthrosc Rel Surg 35:521–527. https://doi.org/10.1016/j.arthro.2018.08.032
Marom N, Greditzer HG, Roux M et al (2020) The incidence of Kaplan fiber injury associated with acute anterior cruciate ligament tear based on magnetic resonance imaging. Am J Sports Med 48:3194–3199. https://doi.org/10.1177/0363546520956302
Berthold DP, Willinger L, Muench LN et al (2020) Visualization of proximal and distal kaplan fibers using 3-dimensional magnetic resonance imaging and anatomic dissection. Am J Sports Med 48:1929–1936. https://doi.org/10.1177/0363546520919986
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
GS conducted dissections, writing and revising of the manuscript. AG dissections and revising of the manuscript. AK writing and revising of the manuscript. SP writing and revising of the manuscript. FB dissections and revising of the manuscript. FF writing and revising of the manuscript. RP writing and revising of the manuscript.TN leading the project, dissections, writing and revising of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study did not need IRB approval due to the use of cadaveric specimen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sayac, G., Goimard, A., Klasan, A. et al. The anatomy of Kaplan fibers. Arch Orthop Trauma Surg 141, 447–454 (2021). https://doi.org/10.1007/s00402-020-03718-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03718-7