Abstract
The osteoarthritic (OA) disease pattern of the knee is one of the determinants for choice of arthroplasty concept when knee replacement is indicated, but whether the disease pattern has a direct effect on postoperative outcome has not previously been investigated. The aim was to investigate if different OA disease patterns have an effect on postoperative outcome after receiving total knee arthroplasty (TKA).
Materials and methods
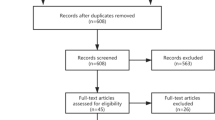
472 patients with pre- and 1-year postoperative patient reported outcome measures (PROMs) undergoing TKA surgery were retrospectively identified and classification of the OA disease pattern was made on preoperative radiographs. Measured resection was the universal technical approach.
Results
The key findings showed greater improvement in mean PROMs for anteromedial OA (AMOA) compared with other OA disease patterns; 3.1 points (95% CI 1.4–4.7, p < 0.001) in Oxford Knee score, 11.7 points (95% CI 0.9–22.5, p = 0.034) in Forgotten Joint score and 0.08 points (95% CI 0.02–0.14, p = 0.007) in EQ 5D score. Similar results were observed when comparing AMOA with AMOA that had only partial thickness cartilage loss (AMOA-PTCL).
Conclusions
Patients with AMOA achieve greater improvement in PROMs after TKA surgery when using measured resection compared with other OA disease patterns. This finding has important implications for reporting, risk stratification and interpretation in TKA outcome studies, including randomized trials, why further investigation of the topic is of highly relevance.



Similar content being viewed by others
References
Hamilton TW, Pandit HG, Lombardi AV et al (2016) Radiological Decision Aid to determine suitability for medial unicompartmental knee arthroplasty: development and preliminary validation. Bone Joint J 98-B:3–10. https://doi.org/10.1302/0301-620X.98B10.BJJ-2016-0432.R1
Goodfellow J, Kershaw C, Benson M, O’Connor J (1988) The Oxford Knee for unicompartmental osteoarthritis—the first 103 cases. J Bone Jt Surg 70 B:692–701
Berend KR, Berend ME, Dalury DF et al (2015) Consensus statement on indications and contraindications for medial unicompartmental knee arthroplasty. J Surg Orthop Adv 24:252–256
Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG (2005) Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Jt Surg 87-A:999–1006
Price AJ, Rees JL, Beard DJ et al (2004) Sagittal plane kinematics of a mobile-bearing unicompartmental knee arthroplasty at 10 years: a comparative in vivo fluoroscopic analysis. J Arthroplast 19:590–597. https://doi.org/10.1016/j.arth.2003.12.082
Pandit H, Gulati A, Jenkins C et al (2017) Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 18:168–171. https://doi.org/10.1016/j.knee.2010.05.003
Maier MW, Kuhs F, Streit MR et al (2015) Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135:1169–1175. https://doi.org/10.1007/s00402-015-2236-4
Hamilton TW, Pandit HG, Ostlere SJ et al (2017) Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss. Bone Joint J 99:475–482. https://doi.org/10.1302/0301-620X.99B4.BJJ-2016-1061.R1
Polkowski GG II, Ruh EL, Barrack RM, Nunley RLB (2013) Is pain and dissatisfaction after TKA related to early-grade preoperative osteoarthritis ? Clin Orthop Relat Res 471:162–168. https://doi.org/10.1007/s11999-012-2465-6
Howell RE, Lombardi AV, Crilly R Jr, Opolot S, Berend KR (2015) Unicompartmental knee arthroplasty: does a selection bias exist? J Arthroplast 30:1740–1742. https://doi.org/10.1016/j.arth.2015.05.010
Williams DP, Blakey CM, Hadfield SG et al (2013) Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J 95-B:45–51. https://doi.org/10.1302/0301-620X.95B1.28573
Rothwell AG, Hooper GJ, Hobbs A, Frampton CM (2010) An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Jt Surg Br 92:413–418. https://doi.org/10.1302/0301-620X.92B3.22913
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “Forgotten Joint” as the ultimate goal in joint arthroplasty. Validation of a new patient-reported outcome measure. J Arthroplast 27:430–436.e1. https://doi.org/10.1016/j.arth.2011.06.035
Brooks R (1996) EuroQol: the current state of play. Health Policy 37:53–72. https://doi.org/10.1016/0168-8510(96)00822-6
Clement ND, MacDonald D, Simpson AHRW (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc 22:1933–1939. https://doi.org/10.1007/s00167-013-2776-5
Kalairajah Y, Orth F, Azurza K et al (2005) Health outcome measures in the evaluation of total hip arthroplasties—a comparison between the Harris Hip Score and the Oxford Hip Score. J Arthroplast 20:1037–1041. https://doi.org/10.1016/j.arth.2005.04.017
Peterfy CG (2002) Imaging of the disease process. Curr Opin Rheumatol. https://doi.org/10.1097/01.BOR.0000025608.46603.62
Weidow J, Mars I, Cederlund C-G, Kärrholm J (2004) Standing radiographs underestimate joint width: comparison before and after resection of the joint in 34 total knee arthroplasties. Acta Orthop Scand 75:315–322. https://doi.org/10.1080/00016470410001259
Keyes GW, Carra J, Miller RK, Goodfellow JW (1992) The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand 63:497–501. https://doi.org/10.3109/17453679209154722
Mukherjee K, Pandit H, Dodd CA et al (2008) The Oxford unicompartmental knee arthroplasty: a radiological perspective. Clin Radiol 63:1169–1176. https://doi.org/10.1016/j.crad.2007.12.017
Mikkelsen M (2016) Unicompartmental knee arthroplasty: a radiographic indications study. Master thesis, Copenhagen Univ, pp 1–9
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF (2011) The position and orientation of total knee replacement components. J Bone Jt Surg 93:629–633. https://doi.org/10.1302/0301-620X.93B5.25893
Nishio Y, Onodera T, Kasahara Y, Takahashi D, Iwasaki NMT (2017) Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J Arthroplast 29:702–706. https://doi.org/10.1016/j.arth.2013.06.035
Beard DJ, Harris K, Dawson J et al (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68:73–79. https://doi.org/10.1016/j.jclinepi.2014.08.009
Thomsen MG, Latifi R, Kallemose T et al (2016) Does knee awareness differ between different knee arthroplasty prostheses? A matched, case-control, cross-sectional study. BMC Musculoskelet Disord 17:141. https://doi.org/10.1186/s12891-016-1001-3
Wise BL, Niu J, Yang MEI et al (2012) Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in Whites and African Americans. Arthritis Care Res (Hoboken) 64:847–852. https://doi.org/10.1002/acr.21606
Felson DT, Nevitt MC, Zhang Y et al (2002) High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheumatol 46:1217–1222. https://doi.org/10.1002/art.10293
Hadi M, Barlow T, Ahmed I et al (2016) Does malalignment affect patient reported outcomes following total knee arthroplasty: a systematic review of the literature. Springerplus 5:1201. https://doi.org/10.1186/s40064-016-2790-4
Parratte S, Pagnano M, Trousdale R, Berry D (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Jt Surg 92:2143–2149. https://doi.org/10.2106/JBJS.I.01398
Lanyon P, O’Reilly S, Jones A, Doherty M (1998) Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis 57:595–601. https://doi.org/10.1136/ard.57.10.595
Beattie KA, Duryea J, Pui M et al (2008) Minimum joint space width and tibial cartilage morphology in the knees of healthy individuals: a cross-sectional study. BMC Musculoskelet Disord 9:119. https://doi.org/10.1186/1471-2474-9-119
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Extract of estimates from multivariate analysis for Table 4
Appendix: Extract of estimates from multivariate analysis for Table 4
Mean difference (95% CI) | p value | |
|---|---|---|
Anteromedial OA: remaining OA patterns | ||
OKS | ||
Sex (M) | 1.54 (− 0.09 to 3.18) | 0.064 |
Age | 0.10 (0.02 to 0.19) | 0.011 |
Pre-OKS | − 0.62 (− 0.73 to − 0.50) | < 0.00 |
Vanguard CR | 4.16 (0.90 to 7.43) | 0.012 |
AGC CR | − 0.09 (− 2.75 to 2.58) | 0.948 |
NexGen CR | − 2.07 (− 6.40 to 2.27) | 0.349 |
Surgeon 1 | − 3.37 (− 8.15 to 1.41) | 0.166 |
Surgeon 2 | − 0.99 (− 17.53 to 15.55) | 0.906 |
Surgeon 3 | − 3.43 (− 8.09 to 1.23) | 0.149 |
Surgeon 3 + 1a | − 9.03 (− 18.02 to − 0.04) | 0.036 |
Surgeon 3 + 5a | 0.08 (− 8.89 to 9.04) | 0.986 |
Surgeon 4 | − 2.26 (− 7.19 to 2.67) | 0.368 |
Surgeon 5 | − 5.95 (− 11.51 to − 0.40) | 0.036 |
Surgeon 6 | 0.26 (− 2.75 to 3.27) | 0.865 |
Surgeon 7 | − 1.28 (− 5.78 to 3.21) | 0.574 |
Surgeon 7 + 1a | − 15.63 (− 32.17 to 0.90) | 0.063 |
Surgeon 8 | − 3.23 (− 7.90 to 1.44) | 0.174 |
Rights and permissions
About this article
Cite this article
Jessing, I.R., Mikkelsen, M., Gromov, K. et al. Patients with anteromedial osteoarthritis achieve the greatest improvement in patient reported outcome after total knee arthroplasty. Arch Orthop Trauma Surg 140, 517–525 (2020). https://doi.org/10.1007/s00402-020-03337-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03337-2