Abstract
Introduction
In Denmark, 20% of all registered total hip arthroplasties (THA) from 1995 to 2014 has been patients younger than 60 years with primary idiopathic osteoarthritis (OA). It is speculated that hip malformations may be a major contributor to early OA development. It has been shown that hip malformation may compromise implant position and, therefore, identifying and knowing the incidence of malformations is important. Our aim was to assess the prevalence and type of hip malformations in a cohort of younger patients undergoing THA.
Materials and methods
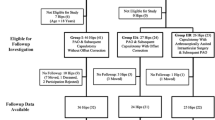
In this prospective two center cohort study, 95 consecutive patients (106 hips) met the inclusion criteria. One observer performed radiographic measurements for malformations and radiographic OA. Inter- and intraobserver variability was assessed.
Results
From 95 patients (male n = 52 and female n = 43) age ranged from 35 to 59 years and prevalences of hip malformations were; CAM-deformity 50.9 and 25.5%, coxa profunda 33 and 27.4%, acetabular retroversion 33 and 29.2%, and acetabular dysplasia 10.4 and 3.8%. All patients showed minimum of one malformation. Prevalences of Tönnis grade 0–1 were 22.6% and 2–3 were 77.4%.
Conclusion
All patients showed malformations, especially high prevalences were found for CAM-deformity, coxa profunda and acetabular retroversion. Identifying these malformations is fairly simple and recognizing the high prevalence may help surgeons avoid pitfalls during implant positioning in THA surgery. Further, focus on hip malformations may facilitate correct referral to joint-preserving surgery before OA develops.




Similar content being viewed by others
References
Klit J, Gosvig K, Magnussen E, Gelineck J, Kallemose T, Soballe K, Troelsen A (2014) Cam deformity and hip degeneration are common after fixation of a slipped capital femoral epiphysis. Acta Orthop 85(6):585–591
Nguyen N-AT, Klein G, Dogbey G, McCourt JB, Mehlman CT (2012) Operative versus nonoperative treatments for Legg-Calve-Perthes disease: a meta-analysis.” J Pediatr Orthop 32(7):697–705
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87(7):1012–1018
Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 466(2):264–272
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2):217–220
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B (2005) Reducing the risk of dislocation after total hip arthroplasty the effect of orientation of the acetabular component. J Bone Jt Surgery Br 87(6):762–769
Ali Khan MA, Brakenbury PH, Reynolds IS (1981) Dislocation following total hip replacement. J Bone Joint Surg Br 63-B(2):214–218
Abe H, Sakai T, Hamasaki T, Takao M, Nishii T, Nakamura N, Sugano N (2012) Is the transverse acetabular ligament a reliable cup orientation guide?” Acta Orthop 83(5):474–480
Ha YC, Yoo JJ, Lee YK, Kim JY, Koo KH (2012) Acetabular component positioning using anatomic landmarks of the acetabulum. Clin Orthop Relat Res 470(12):3515–3523
Leslie IJ, Williams S, Isaac G, Ingham E, Fisher J (2009) High cup angle and microseparation increase the wear of hip surface replacements. Clin Orthop Relat Res 467(9):2259–2265
Wan Z, Boutary M, Dorr LD (2008) The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty 23(1):51–56
Gallo J, Havranek V, Zapletalova J (2010) Risk factors for accelerated polyethylene wear and osteolysis in ABG i total hip arthroplasty. Int Orthop 34(1):19–26
Widmer KH (2007) Containment versus impingement: Finding a compromise for cup placement in total hip arthroplasty. Int Orthop 31(Suppl. 1):29–33
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H (2011) The john charnley award: Risk factors for cup malpositioning: Quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res 469(2):319–329
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ (1998) Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty 13(5):530–534
Garcia-Cimbrelo E, a Diaz-Martin R, Madero, Munera L (2000) Loosening of the cup after low-friction arthroplasty in patients with acetabular protrusion. The importance of the position of the cup. J Bone Joint Surg Br 82(1):108–115
Holt G, Murnaghan C, Reilly J, Meek RMD, Features S (2007) The biology of aseptic osteolysis. Clin Orthop Relat Res 460(460):240–252
Styregruppen for DHR (2013) Dansk hoftealloplastik register—årsrapport 2013,” no. december 2012, pp 2–97
Jacobsen S, Sonne-Holm S, Lund B, Søballe K, Kiaer T, Rovsing H, Monrad H (2004) Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand 75(6):721–729
R Core Team (2013) “R Core Team” R A Lang. Environ. Stat. Comput. R Found. Stat. Comput. Vienna, Austria., pp. ISBN 3-900051-07–00, http://www.R-project.org/
Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E (2007) A new radiological index for assessing asphericity of the femoral head in cam impingement.” J Bone Joint Surg Br 89:1309–1316
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteo-arthritis.” Acta Chir Scand 83:1–132
Jacobsen S, Sonne-Holm S (2005) Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology 44(2):211–218
Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA (2015) What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res 473(4):1234–1246
Siebenrock Ka, Kistler L, Schwab JM, Büchler L, Tannast M (2012) The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res 470:3355–3360
Troelsen A, Rømer L, Kring S, Elmengaard B, Søballe K (2010) Assessment of hip dysplasia and osteoarthritis: variability of different methods. Acta radiol 51:187–193
Jacobsen S (2005) Joint space width in dysplasia of the hip: a case-control study of 81 adults followed for ten years. J Bone Jt Surg-Br 87-B(4):471–477
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Ipach I, Mittag F, Syha R, Kunze B, Wolf P, Kluba T (2012) Indications for total hip arthroplasty in young adults—idiopathic osteoarthritis seems to be overestimated. Rofo 184(3):239–247
Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P (2008) The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol 49(4):436–441
Laborie LB, Lehmann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K (2011) Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology 260(2):494–502
Albers CE, Steppacher SD, Haefeli PC, Werlen S, Hanke MS, Siebenrock KA, Tannast M (2015) Twelve percent of hips with a primary cam deformity exhibit a slip-like morphology resembling sequelae of slipped capital femoral epiphysis. Clin Orthop Relat Res 473(4):1212–1223
Lehmann CL, Arons RR, Loder RT, Vitale MG (2006) The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop 26(3):286–290
Klit J, Gosvig K, Jacobsen S, Sonne-Holm S, Troelsen A (2011) The prevalence of predisposing deformity in osteoarthritic hip joints. HIP Int 21:537–541
Diesel CV, Ribeiro TA, Coussirat C, Scheidt RB, Macedo CAS, Galia CR (2015) Coxa profunda in the diagnosis of pincertype femoroacetabular impingement and its prevalence in asymptomatic subjects. Bone Jt J 97-B(4):478–483
Nepple JJ, Lehmann CL, Ross JR, Schoenecker PL, Clohisy JC (2013) Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Jt Surg 95(5):417–423
Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A (2010) Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am 92(5):1162–1169
Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M (2009) Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res 467(3):666–675
Tannast M, Fritsch S, Zheng G, Siebenrock KA, Steppacher SD (2015) Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res 473(4):1255–1266
Kappe T, Kocak T, Neuerburg C, Lippacher S, Bieger R, Reichel H (2011) Reliability of radiographic signs for acetabular retroversion. Int Orthop 35(6):817–821
Larson CM, Moreau-Gaudry A, Kelly BT, Byrd JWT, Tonetti J, Lavallee S, Chabanas L, Barrier G, Bedi A (2015) Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res 473(4):1247–1254
Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B (2005) Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the osteoarthrosis substudy of the Copenhagen City Heart Study. Acta Orthop 76(2):149–158
Song K-S, Oh C-W, Lee H-J, Kim S-D (2009) Epidemiology and demographics of slipped capital femoral epiphysis in Korea: a multicenter study by the Korean pediatric orthopedic society. J Pediatr Orthop 29(7):683–686
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22(4):815–821
Yamaguchi M, Akisue T, Bauer TW, Hashimoto Y (2000) The spatial location of impingement in total hip arthroplasty. J Arthroplasty 15(3):305–313
Hartig-Andreasen C, Stilling M, Søballe K, Thillemann TM, Troelsen A (2014) Is cup positioning challenged in hips previously treated with periacetabular osteotomy? J Arthroplasty 29(4):763–768
Gromov K, Greene ME, Huddleston JI, Emerson R, Gebuhr P, Malchau H, Troelsen A (2015) Acetabular dysplasia and surgical approaches other than direct anterior increases risk for malpositioning of the acetabular component in total hip arthroplasty. J Arthroplasty 2015:1–7
Epinette J-A, Mertl P, Combourieu B, Goncalves H, Blairon A, Ehlinger M, Tabutin J (2015) Outcomes and prognostic factors in revision hip arthroplasty for severe intra-pelvic cup protrusion: 246 cases. Orthop Traumatol Surg Res 101(6):S257–S263
Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL (2007) The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res 462:115–121
Dudda M, Albers C, Mamisch TC, Werlen S, Beck M (2009) Do normal radiographs exclude asphericity of the femoral head-neck junction?” Clin Orthop Relat Res 467(3):651–659
Hipfl C, Titz M, Chiari C, Schopf V, Kainberger F, Windhager R, Domayer S (2017) Detecting cam-type deformities on plain radiographs: what is the optimal lateral view?. Arch Orthop Trauma Surg 137(12):1699–1705
Naal FD, Miozzari HH, Schär M, Hesper T, Nötzli HP (2012) Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med 40(7):1501–1510
Steppacher SD, Anwander H, Zurmuhle CA, Tannast M, Siebenrock KA (2015) Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have a good clinical result without osteoarthritis progression at 10 years. Clin Orthop Relat Res 473(4):1333–1341
Hufeland M, Kruger D, Haas NP, Perka C, Schroder JH (2016) Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg 136(5):687–691
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Karimi, D., Kallemose, T., Troelsen, A. et al. Hip malformation is a very common finding in young patients scheduled for total hip arthroplasty. Arch Orthop Trauma Surg 138, 581–589 (2018). https://doi.org/10.1007/s00402-018-2900-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2900-6