Abstract
Introduction
Bemiparin has shown to be effective and safe in clinical trials in total knee or hip replacement.
Materials and methods
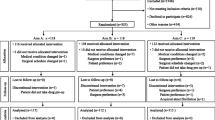
We conducted a prospective, open, multicentre, uncontrolled study to audit the utilisation patterns of bemiparin 3,500 IU/day, first dose administered 6 h after surgery, in 1,009 patients undergoing total hip or knee replacement surgery in standard clinical practice. We analysed rates of documented symptomatic venous thromboembolism (VTE) [deep-vein thrombosis (DVT) and pulmonary embolism (PE)] confirmed by objective methods, major bleeding, death, thrombocytopaenia and other adverse events up to 6 weeks.
Results
Rate of documented symptomatic DVT was 0.3% (95% CI, 0.1–0.9%). No cases of documented PE were reported. There were 14 (1.4%) major bleedings (95% CI, 0.8–2.3%). Neuraxial anaesthesia was used in 937 (92.9%) patients. There were no cases of spinal haematoma, fatal bleeding or bleeding in critical organs. There were 6 (0.6%) cases of mild thrombocytopaenia, which did not require treatment discontinuation. No cases of severe type II heparin-induced thrombocytopaenia were observed. There were no deaths during bemiparin prophylaxis. The median length of hospitalisation was 9 days and 92.5% of patients continued prophylaxis post-hospitalisation for a total median time of 38 days. There were no thromboembolic or bleeding complications during post-hospitalisation prophylaxis. Postoperative start of prophylaxis with bemiparin permitted that 29.3% of patients could be admitted to hospital the same day of the intervention.
Conclusion
Bemiparin prophylaxis, started 6 h after surgery and given for 5–6 weeks after total hip or knee replacement, was associated with low rates of VTE, major bleeding and other adverse events in normal clinical practice. Bemiparin thromboprophylaxis started 6 h after surgery makes neuraxial anaesthesia/analgesia procedures easier, without compromising efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing major orthopaedic surgery, such as total knee replacement (TKR) or total hip replacement (THR) surgery, represent a group at particularly high risk of venous thromboembolism (VTE) [9, 15]. The risk remains high for several weeks after surgery [9]. In these patients, routine chemical thromboprophylaxis has been the standard of care for the past 20 years, thus reducing overall mortality and fatal pulmonary embolism (PE) [5]. Low-molecular-weight heparin (LMWH) is significantly better than warfarin or aspirin in preventing deep-vein thrombosis (DVT) after major orthopaedic surgery [23]. Mechanical means of prophylaxis could provide an additional efficacy [9, 19]. The benefits of neuraxial anaesthesia (i.e. spinal or epidural) are also well established [1, 18].
The widespread use of thromboprophylaxis and neuraxial anaesthesia in patients undergoing major orthopaedic surgery—these procedures are used in 60–95% of all THR or TKR surgeries [8, 14]—makes it necessary to develop new strategies to enhance safety in these patients. Neuraxial anaesthesia should generally be avoided in patients whose preoperative haemostasis is impaired by antithrombotic drugs [9], because of the increased risk of spinal haematoma [11, 21]. In order to avoid preoperative impaired haemostasis, thus minimising the risk of spinal haematoma and intraoperative bleeding, it would be reasonable to start prophylaxis several hours after surgery, whenever the efficacy of LMWH should not be compromised [20, 24].
Bemiparin is a new second-generation LMWH [16] that has shown greater efficacy than standard heparin in a comparative clinical trial conducted by Kakkar et al. in the prevention of VTE after THR surgery [12]. Bemiparin may be started before or after surgery, whereas recommendations for other LMWHs in Europe primarily involve preoperative initiation [4].
In a recent, comparative clinical trial with enoxaparin in total TKR, bemiparin 3,500 IU/day started 6 h after surgery showed a non-significant trend towards a lower incidence of documented symptomatic VTE as compared with enoxaparin 4,000 IU/day started 12 h before surgery, with a similar safety profile [14].
This observational study was designed to gain additional clinical experience with postoperative start of bemiparin prophylaxis in a large population of orthopaedic patients in normal clinical practice.
Materials and methods
This study was designed as a prospective, uncontrolled, open-label, multicentre, observational “real life” assessment of bemiparin, started 6 h after surgery, in patients undergoing TKR or THR surgery. The study was conducted according to the Spanish requirements for observational studies (Circular 4/2000 of the Spanish Medicines Agency) and European Guidelines (CPMP/PhVWP/109/99/corr).
Any patient undergoing TKR or THR surgery was eligible for inclusion in the study. There were no pre-established exclusion criteria in the protocol.
All patients received once daily subcutaneous injections of bemiparin 3,500 IU, starting 6 h after surgery, that were administered during the risk period according to the physician’s criteria. The extent of exposure was shown by the median days (first and third quartile) of bemiparin prophylaxis. Non-pharmacological treatments, such as active or passive mobilisation, elastic bandages and/or intermittent pneumatic compression devices, were used according to the usual practice at each centre and were recorded in the case report form.
The primary effectiveness outcome was documented symptomatic VTE, including DVT, PE or both. If VTE was clinically suspected, it had to be confirmed by objective methods (i.e. Doppler ultrasound or ascending contrast venography for DVT, high-probability lung scanning, pulmonary angiography, helical computed tomography for non-fatal PE, or necropsy in cases of suspected fatal PE). The decision whether or not to perform confirmatory tests was left to physicians’ criteria.
The primary safety endpoint was the occurrence of major bleeding, defined as clinically overt bleeding associated with fall in haemoglobin of at least 2 g/dl or requirement of a transfusion of 2 or more units of blood, bleeding in critical organs (intracranial, spinal, retroperitoneal or intraocular bleeding), fatal bleeding, bleeding requiring reoperation to control bleed, or any bleeding requiring treatment cessation. Minor bleeding was any other overt bleeding that did not fulfil the criteria of major bleeding.
The following analytical parameters were tested: haematocrit, hemoglobin, platelets, AST (aspartate aminotransferase), ALT (alanine aminotransferase) and GGT (gamma-glutamyl transpeptidase). Thrombocytopaenia was defined as a platelet count < 150,000/mm3 during bemiparin prophylaxis. Postoperative anaemia was defined as a haemoglobin value <12 g/dl at hospital discharge. The incidence of death, allergic reactions, wound haematoma/bruising and reactions at injection site were also assessed.
Three visits were scheduled: the first one the day of surgery (baseline), the second one at the time of hospital discharge (outcome assessment visit), and the third one during the first outpatient visit (follow-up visit), according to standard clinical practice.
Ninety-five percent confidence intervals were calculated for the rates of VTE, major and minor bleeding events, thrombocytopaenia, deaths and allergic reactions. These calculations were performed using SPSS software, version 7.5.
Results
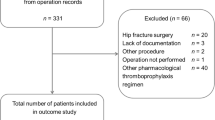
Between November 2001 and March 2003, 1,009 patients were enrolled in 23 Spanish centres. Baseline characteristics of patients included in the study are shown in Table 1. Among the 1,009 patients included, 653 (64.7%) underwent TKR surgery and 356 (35.3%) underwent THR surgery. Mean age of patients included was 70.9 years. Most patients were females (66.8%), and mean body weight was 76.9 kg. Neuraxial anaesthesia, alone [882 patients (87.4%)] or in combination with general anaesthesia [55 patients (5.5%)], was administered to 937 (92.9%) patients. Patients received bemiparin prophylaxis for a median time of 8 days during hospitalisation. More than 90% of patients continued extended outpatient prophylaxis with bemiparin 3,500 IU/day for 30 additional days (median) (Table 1). Twenty-nine percent of patients were admitted to hospital on the same day of surgery (Table 1).
All patients had an outcome assessment at hospital discharge. Three (0.3%; 95% CI, 0.1–0.9%) of the 1,009 patients experienced symptoms of DVT (Table 2). All of them occurred while in the hospital, 6–9 days after surgery. The events were two proximal DVTs after TKR and one distal DVT after THR, which were confirmed by Doppler ultrasound. One patient undergoing KR developed symptoms of PE on post-operative day 4. However, the event was ruled out by lung scanning. There were no cases of VTE after hospital discharge.
Major bleeding occurred in 14 (1.4%; 95% CI, 0.8–2.3%) of the 1,009 patients (Table 2). All major bleeding events occurred during hospitalisation, and included ten cases of excessive wound bleeding, three haemarthroses of the prosthetic joint, and one gastrointestinal bleeding (coffee ground vomiting). None were fatal. Of all major bleedings, one excessive wound bleeding occurred before the first bemiparin dose, and required reoperation for control. The major gastrointestinal bleeding occurred in one patient with a clinical history of grade III gastroesophageal reflux and hiatal hernia who was concomitantly receiving an intravenous non-steroidal anti-inflammatory drug (NSAID). Both medications, NSAID and bemiparin, were stopped. Two days after patient recovery, bemiparin was re-started and the adverse event did not recur. A total of 937 (92.9%) patients received neuraxial anaesthesia, and no cases of spinal haematoma were reported.
There were no deaths during the treatment period with bemiparin. Thrombocytopaenia was seen in 6 (0.6%; 95% CI, 0.2–1.3%) of the 1,009 patients included (Table 2). Thrombocytopaenia ranged from 80,000/mm3 to 135,000/mm3, and none of this required treatment discontinuation. There were no cases of severe heparin-induced thrombocytopaenia (HIT type-II). Mild to moderate postoperative anaemia (Hb 8–12 g/dl) was shown in 484 (48.0%) patients. Only three (0.3%) patients had haemoglobin levels <8 g/dl during the study. Mild, transient increases in serum aminotransferases, always less than three times the upper normal limit, were reported in 2.1% (AST), 4.0% (ALT) and 3.2% (GGT) of patients included. None of the cases were clinically significant and none of them required treatment discontinuation. A minor allergic reaction, consisting of mild urticaria around the injection site, was seen in one patient (0.1%; 95% CI, 0.0–0.6%). Treatment was not discontinued. There were no cases of systemic or general allergic reactions. Among all patients included, 16.1% developed surgical wound haematoma/bruising (95% CI, 13.8–18.5%), and none of them needed local reintervention or prolonged hospitalisation. Overall, 1.5% patients experienced surgical wound infection. Only 6 of 23 centres reported any surgical wound infection. Injection site reactions were reported in 20% of patients. Most of these reactions were mild ecchymoses. There were no cases of injection site haematomas greater than 5 cm in diameter or requiring treatment discontinuation. There were no rare or unexpected adverse drug reactions to bemiparin during the study.
Follow-up
A total of 931 patients (92.5%) received extended outpatient prophylaxis. There were no thromboembolic or haemorrhagic complications during the time from hospital discharge to the follow-up visit. A 72-year-old male patient with clinical history of ischaemic heart disease died from an acute myocardial infarction 2 months after TKR surgery and 20 days after the last bemiparin dose.
Discussion
A low incidence of documented symptomatic VTE was seen when bemiparin was started 6 h after surgery in normal clinical practice. The incidence of documented symptomatic VTE during hospitalisation in our observational study was 0.3% (two proximal DVTs, one distal DVT, and no cases of documented symptomatic PE), which is entirely comparable and even lower than the incidence of symptomatic VTE reported with other antithrombotic drugs during short-term prophylaxis after major orthopaedic surgery [22]. It must be pointed out that comparisons of the results of observational studies with those of clinical trials should be interpreted with caution, given the methodological differences between the two types of studies.
In our study, more than 90% of patients received extended prophylaxis with bemiparin for a median time of 38 days. No cases of VTE were reported during extended bemiparin prophylaxis after hospital discharge. The incidence is lower than the 1.3% (range 0–3.5%) rate of symptomatic VTE reported in a recent meta-analysis with other LMWH during extended prophylaxis after TKR or THR [6], or the 3.3% incidence with placebo in the same meta-analysis [6], and lower than the 0.3% incidence of symptomatic VTE during extended prophylaxis with fondaparinux [7]. The duration of prophylaxis used in our study is consistent with current recommendations [9] including the use of prolonged prophylaxis for up to 4–5 weeks in patients undergoing THR surgery. The need of prolonged thromboprophylaxis after TKR is still in debate [9]. Nevertheless, a recent meta-analysis showed that, among patients undergoing THR or TKR, extended-duration prophylaxis significantly reduced the frequency of symptomatic venous thromboembolism [6]. The reduction in risk of symptomatic VTE was higher in THR than in TKR [6].
We found a low incidence of major bleeding complications—1.4%—which agrees with the reported incidence for short-term in-hospital prophylaxis with bemiparin during clinical trials in major orthopaedic surgery [12, 14]. This rate is lower than the 2.7% incidence reported with fondaparinux and similar to the 1.7% incidence reported with enoxaparin during short-term in-hospital prophylaxis after major orthopaedic surgery in selected populations from clinical trials [3]. In addition, no major bleeding complications were reported during extended outpatient prophylaxis with bemiparin in our study, which is similar to the 0.1% incidence of major bleeding found in a recent meta-analysis of extended LMWH prophylaxis in TKR or THR surgery [6], and lower than the 2.4% incidence seen during extended outpatient prophylaxis with fondaparinux [7].
In our observational study, there were no deaths during the study period. All cases of thrombocytopaenia were mild to moderate and did not require treatment discontinuation. There were no cases of type-II severe thrombocytopaenia. The rates of surgical wound haematoma/bruising and injection site reactions were similar to those previously reported with bemiparin, and lower than reported with enoxaparin in a comparative clinical trial in TKR [14]. No rare or unexpected adverse drug reactions to bemiparin occurred during the study.
In our study, nearly one-third of patients included were admitted to hospital the same day of surgery, instead of on the evening before the procedure, thus potentially reducing hospital stay costs. In a recent pharmacoeconomic study, bemiparin administered postoperatively was a dominant strategy over enoxaparin administered preoperatively, offering better outcome at lower cost [10].
In our study, neuraxial anaesthesia was used alone or combined with general anaesthesia in more than 90% of patients, and no cases of spinal haematoma were reported. Although the timing of the first administration of thromboprophylaxis is controversial [17], it is recognised that bemiparin administration started 6 h after surgery does not compromise efficacy [14], and is compatible with neuraxial anaesthesia techniques [11]. On the contrary, patients on preoperative LMWH thromboprophylaxis can be assumed to have altered coagulation. In these patients, needle placement should occur at least 10–12 h after the LMWH dose [11]. Thromboprophylaxis started less than 6 h after surgery may increase the risk of bleeding without improved efficacy [17]. Initiation 12–24 h postoperatively may be less effective than initiation at 6 h [17].
This study has several methodological limitations. However, the results of this observational study should be interpreted in the setting of normal clinical practice. This type of studies add information that is not available in randomised controlled trials [2] where exclusion criteria, limited sample size and use in specific clinical situation leads to significant loss of useful pragmatic data. Therefore, we were able to assess the “real life” effect of bemiparin in a large audit of orthopaedic patients. Clinical endpoints are of major value to assess the effects of a new drug in clinical studies on the prevention of VTE [13].
In conclusion, bemiparin prophylaxis, started 6 h after surgery and given for 5–6 weeks after THR or TKR was associated with low rates of VTE, major bleeding and other adverse events in normal clinical practice. Moreover, bemiparin thromboprophylaxis started 6 h after surgery minimises the risk of spinal haematoma and makes neuraxial anaesthesia/analgesia procedures easier, without compromising efficacy.
References
Beattie WS, Badner NH, Choi P (2001) Epidural analgesia reduces postoperative myocardial infarction: a meta-analysis. Anesth Analg 93:853–858
Black N (2001) Why we need observational studies to evaluate the effectiveness of health care. BMJ 312:1215–1218
Bounameaux H, Perneger T (2002) Fondaparinux: a new pentasaccharide for thrombosis prevention. Lancet 359:1710–1711
Chapman TM, Goa KL (2003) Bemiparin: A review of its use in the prevention of venous thromboembolism and treatment of deep vein thrombosis. Drugs 63:2357–2377
Dahl OE, Caprini JA, Colwell CW Jr, Frostick SP, Haas S, Hull RD, Laporte S, Stein PD (2005) Fatal vascular outcomes following major orthopedic surgery. Thromb Haemost 93:860–866
Eikelboom JW, Quinlan DJ, Douketis JD (2001) Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet 358:9–15
Eriksson BI, Lassen MR; PENTasaccharide in HIp-FRActure Surgery Plus Investigators (2003) Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med 163:1337–1342
Fenollosa J, Seminario P (2001) Eficacia y seguridad de bemiparina en la profilaxis del tromboembolismo venoso en cirugía ortopédica. Rev Ortop Traumatol 6:460–465
Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, Ray JG (2004) Prevention of venous thromboembolism: the 7th ACCP conference on antithrombotic and thrombolytic therapy. Chest 126:338S–400S
Honorato J, Gómez-Outes A, Navarro-Quilis A, Martínez-González J, Rocha E, Planès A (2004) Pharmacoeconomic analysis of bemiparin and enoxaparin as prophylaxis for venous thromboembolism in total knee replacement surgery. Pharmacoeconomics 22:885–894
Horlocker TT, Wedel DJ, Benzon H, Brown DL, Enneking FK, Heit JA, Mulroy MF, Rosenquist RW, Rowlingson J, Tryba M, Yuan CS (2003) Regional anesthesia in the anticoagulated patient: defining the risks (the second ASRA consensus conference on neuraxial anesthesia and anticoagulation). Reg Anesth Pain Med 28:172–197
Kakkar VV, Howes J, Sharma V, Kadziola Z (2000) A comparative, double-blind, randomized trial of a new second generation LMWH (Bemiparin) and UFH in the prevention of post-operative venous thromboembolism. The Bemiparin Assessment Group. Thromb Haemost 83:523–529
Lowe GD, Sandercock PA, Rosendaal FR (2003) Prevention of venous thromboembolism after major orthopaedic surgery: is fondaparinux an advance?. Lancet 362:504–505
Navarro-Quilis A, Castellet E, Rocha E, Paz-Jiménez J, Planès A (2003) Efficacy and safety of Bemiparin compared with Enoxaparin in the prevention of venous thromboembolism after total knee arthroplasty. A randomized double-blind clinical trial. J Thromb Haemost 1:425–432
Nicolaides AN, Breddin HK, Fareed J, Goldhaber S, Haas S, Hull R, Kalodiki E, Myers K, Samama M, Sasahara A; Cardiovascular Disease Educational, Research Trust, the International Union of Angiology (2001) Prevention of venous thromboembolism international consensus statement. Guidelines compiled in accordance with the scientific evidence. Int Angiol 20:1–37
Planes A (2003) Review on bemiparin sodium—a new second generation low-molecular-weight heparin—and its applications in venous thromboembolism. Expert Opin Pharmacother 4:1551–1561
Raskob GE, Hirsh J (2003) Controversies in timing of the first dose of anticoagulant prophylaxis against venous thromboembolism after major orthopaedic surgery. Chest 124:379S–385S
Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S (2000) Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ 321:1493–1497
Silbersack Y, Taute BM, Hein W, Podhaisky H (2004) Prevention of deep-vein thrombosis after total hip and knee replacement. Low-molecular-weight heparin in combination with intermittent pneumatic compression. J Bone Joint Surg Br 86:809–812
Strebel N, Prins M, Agnelli G, Buller HR (2002) Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med 162:1451–1456
Tryba M (1998) European practice guidelines: thromboembolism prophylaxis and regional anesthesia. Reg Anesth Pain Med 23(2 Suppl):178–182
Turpie AG, Bauer KA, Eriksson BI, Lassen MR (2002) Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med 162:1833–1840
Westrich GH, Haas SB, Mosca P, Peterson M (2000) Meta-analysis of thromboembolic prophylaxis after total knee arthroplasty. J Bone Surg Br 82-B:795–800
Zufferey P, Laporte S, Quenet S, Molliex S, Auboyer C, Decousus H, Mismetti P (2003) Optimal low-molecular-weight heparin regimen in major orthopaedic surgery. A meta-analysis of randomised trials. Thromb Haemost 90:654–661
Acknowledgment
Supported by a research grant of Laboratorios Farmacéuticos Rovi, Madrid, Spain.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
Members of the “Bemiparin 6 Hours After Surgery” Study Group (all in Spain): J.I. Abad, M. Pardo, J.A. Alba, H. Carlos Haya, Málaga; P. Marquina, M.A.Z., Zaragoza; O. Tendero, J. Gascó, H. Son Dureta, P. Mallorca; P. Puertas, F. García-Zafra, H. Consolación/Cl. San José, Murcia; L. Salinas, A. Alvarez-Querol, H. Virgen del Consuelo, Valencia; A. Navarro-Quilis, E. Castellet, J. Nardi, H. Vall d’Hebrón, Barcelona; J. Fenollosa, H. Dr. Peset, Valencia; D. Serfati, H. Clínico San Carlos, Madrid; I. Otermin, Cl. Ubarmin, Pamplona; C. Sánchez- Díaz, Hosp. General, Alicante; A. Blanco, H. General Yagüe, Burgos; R. Llombart, Clínica Quirón, Valencia; G. Giménez, Cl. Mare Nostrum, Alicante; Dr. V. Zapata, H. El Tomillar, Sevilla; L.J. Roca, Clínica Victoria Eugenia, Sevilla; J. del Boz, H. San Juan de Dios, Sevilla; J.E. Minguet, Clínica Sta. Isabel, Sevilla; M. Fernández-Fairen, J. Roure, Policlínica Granollers, Barcelona; L. Peidró, F. Maculé, H. Clínico, Barcelona; S. Fuentes, H. Reina Sofía, Córdoba; E.J. García, H. Calatayud, Zaragoza; J.A. Monzón, I. Eguiraun, H. San Juan de Dios Santurce, Bilbao; R. Torres, Clínica Cemtro, Madrid.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Abad, J.I., Gómez-Outes, A., Martínez-González, J. et al. A prospective observational study on the effectiveness and safety of bemiparin, first dose administered 6 h after knee or hip replacement surgery. Arch Orthop Trauma Surg 127, 665–670 (2007). https://doi.org/10.1007/s00402-006-0239-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-006-0239-x