Abstract
Tuberculous arthritis of the elbow joint is not commonly seen by orthopaedic physicians. In the past 20 years, with the pandemic of the human immunodeficiency virus and the increase in immunocompromised people, we have observed a resurgence of tuberculosis. Osteoarticular involvement has increased, too. Spinal and monoarthritis of weight-bearing joints such as the hip or knee are most frequently involved. The elbow joint is an uncommon location of osteoarticular tuberculosis. The aim of this case report is to describe a case of tuberculous arthritis of the elbow and the diagnostic problems that may arise and lead to a delay in treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis affects one-third of the world’s population. This problem has increased in the past few years in relation to acquired immuno-deficiency syndrome (AIDS) and immigration of people from endemic zones. Skeletal tuberculosis occurs in 1%–3% of the cases and represents the third form of extrapulmonary tuberculosis after ganglion and kidney affection [3]. Elbow tuberculosis accounted for 1%–5% of the cases, and the elbow is the joint more commonly affected in the upper extremity [2]. It is very important to suspect a tuberculosis aetiology in a patient affected with chronic monoarticular arthritis with risk factors that present an insidious evolution.
We describe a case of tuberculous arthritis of the elbow and the difficult diagnosis that was established by DNA extracted from a specimen and confirmed by anatomo-pathological studies. The treatment consisted of antituberculous drugs, surgical synovectomy, debridement and curettage.
Case report
We report the case of a 75-year-old man who presented with a history of pain and a gradually appearing soft-tissue mass in the left elbow lasting 1 year. In the last month, he had suffered intermittent low-grade fever and chills, and he was referred to our institution for further evaluation and treatment. There was no history of trauma or previous arthritis. He only had a history of diabetes mellitus and polycythemia vera without antecedent of tuberculosis.
Physical examination revealed a nodular elastic mass with some tenderness over the epitrochlea region of the elbow. This mass measured approximately 6×4x5 cm, and the overlying skin appeared normal with no wounds, scars or rash. The range of motion of the left elbow was limited, with a loss of extension of about 30 deg. Pronation and supination were also limited. No constitutional symptoms were present.
Admission laboratory findings were an erythrocyte sedimentation rate of 45 mm/h, C-reactive protein of 1.8 mg/l, and leukocytes 10.95×109 /L (87% neutrophils, 5.8% lymphocytes).
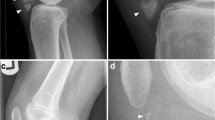
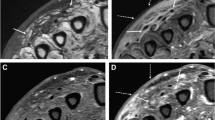
Plain radiography (Fig. 1) showed a lytic focus in the trochlea of the humerus, osteopenic bone adjacent, an impression of soft-tissue swelling, and elbow joint intact. A radiograph of the chest revealed normal findings. MRI was performed and demonstrated the extent of bone erosion over the trochlea of the humerus, diffuse synovitis, leakage from the joint, periarticular soft-tissue, diffuse decrease in signal intensity on T1-weighted images and increased signal on T2-weighted images, and a demarcated fluid collection that appeared to be located posterior to the biceps brachii muscle (Fig. 2).
Microscopy examination and culture of the liquid obtained by punction were negative. Only the tuberculin skin test was positive. The bone scan with marked leukocytes was negative.
Synovectomy and curettage of the bone was performed, and microbiological and anatomo-pathological studies were done. No acid-fast bacilli were detected in sample studies (PAS, Zhiel-Nielsen), but DNA testing for Mycobacterium tuberculosis amplified using the polymerase chain reaction (PCR) was positive. The typical caseous granulomas were observed in the anatomo-pathological studies, and the diagnosis was confirmed. Antibiotic treatment with rifampicin, isoniazid, ethambutol and pyrazinamide for 2 months followed by rifampicin and isoniazid for 6 months resolved the infection. Two years later, the patient was asymptomatic, and the range of movement of the left elbow was normal.
Discussion
In the past few years, an important increase in the incidence of patients with osteoarticular tuberculosis in association with AIDS in developing countries has been observed. The increased incidence is due to many factors including human immunodeficency virus (HIV) infection, immigration from endemic areas, alcoholism, chronic kidney disorders, immunosuppressive therapy, homelessness, crowded living conditions, drug addiction, intra-articular steroid injection, systemic illness and poor access to medical care [6, 10]. Osteoarticular tuberculosis occurs in 1%–3% of all cases of tuberculosis, but this incidence is greater in those series that include immigrants from endemic zones or immunodepressed people (2%–4%) [6].
Spinal tuberculosis is the most common form of osteoarticular tuberculosis. Joints of the upper extremity are less often affected than those of the lower extremities. Elbow tuberculosis is a rare affection and represents 1%–5% of all cases of osteoarticular tuberculosis [2, 5]. Several unusual presentations of musculoskeletal involvement have also been reported [1, 4].
Similar to other infectious arthritis, tuberculosis of the joints is characteristically a monoarticular disease. Approximately 90% of the cases of monoarticular arthritis are osteoarticular tuberculosis [5, 7]. The multifocal osteoarticular tuberculosis and tubercular osteomyelitis without articular affection are infrequent manifestations of osteoarticular tuberculosis.
Musculoskeletal involvement is caused by haematogenous, lymphatic or direct local spread of tubercle bacilli from other lesions from a quiescent pulmonary primary or other extraosseous focus. It is exceptional, but there are rare lesions due to direct inoculation [2, 8].
Tuberculous arthritis commonly presents with chronic pain accompanied by swelling and progressive loss of function. Pain is the more common symptom. The onset is usually insidious, the diagnosis is often delayed, and the functional results after treatment may be poor, especially when there is extensive bone and articular destruction [7]. A history of tuberculosis infection or exposure may or may not be present. In approximately 50% of patients, however, no radiographic evidence of pulmonary involvement can be identified. In the absence of co-existing active pulmonary disease, tuberculosis is frequently not considered in the differential diagnosis of chronic inflammation of the joints [3, 5, 7].
A positive tuberculin skin test supports the diagnosis, but a negative result should not be considered as evidence excluding tuberculosis infection.
The radiological findings are non-specific in the early stages, and the initial lesions are easily missed. As the disease progresses, periarticular osteopenia can become extensive. Later on, varying degrees of cartilage destruction and periarticular bone destruction are seen. Relative preservation of joint space narrowing becomes apparent, which may be modest at first but increases as the articular cartilage is destroyed. If the disease is left untreated, complete joint obliteration with fibrous ankylosis of the joint may result. The typical radiographic findings of osteoarticular tuberculosis are periarticular osteoporosis, peripherally located osseous erosions and gradual narrowing of the cartilage space. This triad of radiographic features (Phemister trial) is characteristic of tuberculous arthritis [7].
MRI is the best modality for evaluating soft-tissue masses. Bone scans with 99mTc are more sensitive than conventional radiography to identify osteomyelitis foci in the early phases.
CT may facilitate the diagnosis through guided percutaneous biopsy. The definitive diagnosis is made from a positive mycobacterial culture and histologic examination of the synovial fluid or synovial membrane. Material for culture may be obtained from aspiration of joint fluid, thus synovial or bone biopsy. Examination of a biopsy specimen is the most important and useful diagnostic method. If osteoarticular tuberculosis is diagnosed and treated at an early stage, approximately 90%–95% of patients heal with near normal function [9].
The disability resulting from osteoarticular tuberculosis is related to the time of detection of the disease and initiation of appropriate treatment. A long history of symptoms and extensive involvement of bone and joint are associated with poor results. Before antibiotic therapy, osteoarticular tuberculosis was treated with long periods of immobilisation. Currently, multidrug chemotherapy and active-assisted non-weight-bearing exercises of the involved joint are the mainstay of treatment. The drugs of primary choice for the treatment of skeletal tuberculosis are the same as those for other forms of tuberculosis: rifampicin, isoniazid, ethambutol and pyrazinamide. However, there is a worldwide threat of an untreatable epidemic of multidrug-resistant tuberculosis with the global explosion of HIV. Surgery may be indicated in a few cases mainly for biopsy and histopathologic confirmation of the disease. If the patient is not responding to the chemotherapy, synovectomy and debridement, or the healed status has resulted in a painful ankylosis, joint arthrodesis or joint replacement may be considered [9].
In conclusion, we believe that osteoarticular tuberculosis should be considered in patients who present with unexplained soft-tissue swelling and pain, particularly if they are immunosuppressed or were born in an endemic area. Thus, an early diagnosis and adequate treatment can be followed by good functional results. Differential diagnoses in patients with elbow swelling should included pyogen arthritis, gout, pigmented villonodular synovitis, haemophilic arthropathy, rheumatoid arthritis, synovial osteochondromatosis and tumours [3, 7].
References
Babhulkar SS, Pande SK (2002) Extraspinal tuberculosis: unusual manifestations of osteoarticular tuberculosis. Clin Orthop 2002:114–120
Chen WS, Wang CJ, Eng HL (1997) Tuberculous arthritis of the elbow. Int Orthop 21:367–370
Davidson PT, Horowitz I (1970) Skeletal tuberculosis. A review with patient presentations and discussion. Am J Med 48:77–84
García S, Combalía A, Serra A, Segur JM, Ramón R (1997) Unusual locations of osteoarticular tuberculosis. Arch Orthop Traum Surg 116:321–323
Hunfeld KP, Rittmeister M, Wichelhaus TA, Brade V, Enzensberger R (1998) Two cases of chronic arthritis of the forearm due to Mycobacterium tuberculosis. Eur J Microbiol Infect Dis 17:344–348
Khan K, Muenning P, Bheta M, Zivin JG (2002) Global drug-resistance patterns and the management of latent tuberculosis infection in immigrants to the United States. N Engl J Med 347:1850–1859
Martini M (1988) Tuberculosis of the bones and joints, 2nd edn. Springer, Berlin Heidelberg New York
Muradali D, Gold WL, Vellend H, Becker E (1993) Multifactorial osteoarticular tuberculosis: report of four cases and review of management. Clin Infect Dis 17:204–209
Tuli SM (2002) General principles of osteoarticular tuberculosis. Clin Orthop 2002:11–19
Vallés X, Sánchez F, Pañella H, García de Olalla P, Jansá JM, Caylà JA (2002) Tuberculosis importada: una enfermedad emergente en países industrializados. Med Clín (Barc) 118:376–378
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Domingo, A., Nomdedeu, M., Tomás, X. et al. Elbow tuberculosis: an unusual location and diagnostic problem. Arch Orthop Trauma Surg 125, 56–58 (2005). https://doi.org/10.1007/s00402-003-0612-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-003-0612-y