Abstract
The nitric oxide (NO)–protein kinase G (PKG) pathway has been known for some time to be an important target for cardioprotection against ischaemia/reperfusion injury and heart failure. While many approaches for reducing infarct size in patients have failed in the past, the advent of novel drugs that modulate cGMP and its downstream targets shows very promising results in recent preclinical and clinical studies. Here, we review main aspects of the NO–PKG pathway in light of recent drug development and summarise potential cardioprotective strategies in which cGMP is the main player.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the initial discovery that nitric oxide (NO) is the endothelial-derived relaxing factor, the last few decades have seen intensive research directed toward understanding this signal molecule and its intracellular signalling cascades. Numerous preclinical studies have shown promising results suggesting a cardioprotective role of NO signalling and revealed the NO–cGMP–PKG cascade as the responsible signalling pathway [6, 27, 28, 30, 39, 63]. Indeed numerous studies have demonstrated that disruption of this pathway leads to various pathological changes in the heart, including vascular and ventricular dysfunction, fibrosis and hypertrophy. Although not all studies are in accordance with this optimistic view on the NO–cGMP–PKG system, targeting this pathway has gained much attention, particularly from scientists keen to develop an efficient drug to treat heart failure. In this brief review, we will focus on pharmacological aspects of the cGMP–PKG pathway with updates from recent preclinical and clinical studies in relation to its direct effect on the heart. We also refer readers to excellent recent reviews providing in-depth overview of NO–cGMP–PKG pathway such as [40].
Cardioprotective cGMP–PKG pathway
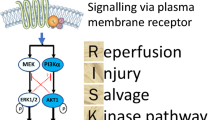
NO and natriuretic peptides (NPs) are the two known classes of upstream molecules that can trigger the cGMP–PKG pathway. NO initiates the signalling pathway by activating soluble guanylate cyclase (sGC), a heterodimeric enzyme consisting of α- and β-subunits with a prosthetic heme moiety, which catalyses cGMP synthesis. On the other hand, NPs, such as ANP (atrial NP), BNP (brain NP) and CNP (C-type NP), activate particulate GC (pGC) present in the plasma membrane to produce cGMP. Both sGC and pGC generate the same second messenger cGMP, but the downstream effects of cGMP can be strikingly different depending on its subcellular localization. The elevated intracellular level of cGMP exerts its physiological actions largely by targeting cGMP-dependent protein kinase (PKG). In mammals PKG-I is the primary kinase responsible for transducing the physiological effects in the cardiovascular system. PKG-Iα and PKG-1β have different N-termini derived from alternative splicing. It is reported that PKG-Iα is ten times more sensitive to cGMP than PKG-1β. Also, due to a unique cysteine residue (Cys 42) in PKG-Iα, it can be activated by thiol-oxidation independently of cGMP [4]. This cGMP-independent form of PKG-1α activation is able to lower blood pressure through vasodilation, but its effect in cardiomyocytes is unknown.
A number of studies have suggested that there are multiple downstream effectors of cGMP-PKG-I in the cardiovascular system. For example, an elevated level of cytosolic Ca2+ can result in increased cardiomyocyte inotropy but it is also known to be a lethal cause of reperfusion injury to cardiomyocytes. Several targets have been proposed as downstream PKG effectors regulating Ca2+ homeostasis in cardiomyocytes [11]. One of the proposed mechanisms is that PKG-I phosphorylates phospholamban at Ser16, which subsequently activates SR Ca2+-ATPase (SERCA). Activated SERCA increases re-uptake of Ca2+ into the sarcoplasmic reticulum (SR) and attenuates the cytosolic Ca2+ during systole [31]. Also, it was demonstrated that cGMP-mediated PKG-I activation induces opening of mitoKATP channels residing on the inner membrane of mitochondria, and the subsequent increased K+ influx causes alkalinisation of the matrix which increases H2O2 production from complex I. The increased H2O2 activates PKC-ε and consequently protects cardiomyocytes from cell death by inhibiting the opening of mitochondrial permeability transition pores (MPTP) [11, 12, 47]. A more recent study showed that opening of cardiomyocyte Ca2+-activated K+ channels of the BK type (CMBK) is a critical modulator in remodelling following myocardial infarction (MI) using CMBK-knockout (KO) mice [24]. The study showed that more severe myocardial damage observed in the CMBK-deficient hearts after ischaemia/reperfusion (I/R) is accompanied by a significantly increased production of reactive oxygen species (ROS). Furthermore, the study showed that pharmacological agents that elevate intracellular cGMP no longer exhibited cardioprotective effects in CMBK-KO mice. Collectively, the authors proposed the GC–cGMP–CMBK pathway as a novel therapeutic target for preventing post-MI cardiac remodelling.
Although the precise mechanistic details how the cGMP–PKG pathway signals and interacts with downstream effectors to protect the heart remain to be characterised, a large number of preclinical studies have revealed the cardioprotective potency of the cGMP–PKG pathway by employing pharmacological tools or by manipulating relevant genes. Based on our limited understanding, the current therapeutic strategy for targeting this pathway is either by increasing cGMP biosynthesis (i.e. sGC activators or stimulators) or reducing cGMP’s catabolism (i.e. PDE inhibitors).
Nitric oxide
Nitric oxide (NO) is a key upstream molecule able to increase intracellular cGMP. NO is generated as a by-product of the enzymatic conversion of l-arginine to l-citrulline by nitric oxide synthases (NOS) [60]. These include endothelial NOS (eNOS), neuronal NOS (nNOS) and inducible NOS (iNOS). All three isoforms are expressed in the cardiovascular system but have distinct subcellular localizations. eNOS and nNOS are constitutively expressed and work in a Ca2+-calmodulin-dependent manner, whereas iNOS is only expressed in response to inflammatory stimuli [7]. Although the cell-specific function of each isoform has not yet been fully elucidated, deletion of all three isoforms in mice resulted in the severe pathological phenotypes such as MI, spontaneous coronary artery disease and sudden cardiac death, demonstrating the cardioprotective importance of NOS in the cardiovascular system [45]. While l-arginine is the major substrate for endogenous NO production, nitrite, which can be elevated in the circulation by dietary intake, is another important source of NO [17, 51]. Nitrite can be converted non-enzymatically to NO via protonation at the low pH of the stomach [3]. Nitrite absorbed in blood and other tissues can be reduced to NO by xanthine oxidoreductase (XOR) or by a nitrite reductase activity of deoxygenated heme proteins such as deoxyhemoglobin. It is interesting to note that the rate of NO generation from nitrite is linearly dependent on reductions in oxygen and pH levels. Indeed exogenous nitrite reduced cardiac infarct size in mice subjected to myocardial I/R injury by upregulating NO [17, 29]. Due to nitrite’s high stability in the circulation, it is an important endocrine reservoir of NO. The beneficial effect of NO, at least in rodent models, has been widely reported, but there have also been discrepant results in some models. Several studies reported that NOS inhibition protects the hearts from I/R injury [21, 58, 66] and in one report exogenous NO administration actually worsened the functional recovery following I/R [57]. Furthermore, it has been shown that the infarct modulating effect of nitrite against myocardial I/R injury was very dose-dependent in mice [17]. Collectively, those studies suggest that the therapeutic effect of NO during I/R depends on dose, source, schedule and species.
Organic nitrates have been used as short-term treatment for acute MI, decompensated heart failure, and hypertensive crisis but their value in chronic treatment has been limited due to unfavourable hemodynamic effects, short plasma half-life, and the development of clinical tolerance. Much research has been devoted to overcoming these drawbacks of organic nitrates by developing a novel class of NO-releasing drugs. NO-releasing Aspirin (NCX4016), has been developed with a timed NO-releasing property [33] and has been extensively studied in various animal models. In addition to aspirin-related inhibition of platelet aggregation, chronic treatment with NCX4016 exerted an infarct-limiting effect in rabbits, pigs, and both normal and diabetic rats during myocardial I/R while native aspirin failed to protect against infarction [5, 53, 64]. Another class of novel NO-releasing drugs is the NO-statins such as NCX 6550 which showed anti-inflammatory, anti-proliferative and antiplatelet effects beyond the actions of statins alone [16, 48].
The cardioprotective properties of NO are not limited to the cGMP–PKG-dependent pathway. It has been shown that NO can directly modify proteins through protein S-nitrosylation (SNO), which has recently emerged as an important post-translational protein modification and may offer great therapeutic potential in cardiovascular diseases [9, 10, 61]. Interestingly, mitochondria-selective S-nitrosylation by mitochondrial-targeted S-nitosothiol (MitoSNO) showed an infarct-reducing effect and improved cardiac function with myocardial I/R injury when it was administered 5 min before the onset of reperfusion. Complex I generates an excessive amount of ROS early in reperfusion due to succinate-driven reverse electron transport (RET) in mitochondria during I/R [49]. A cysteine residue (Cys39) in complex I becomes susceptible to S-nitrosylation in the ischemic heart muscle whenever the absence of respiration leads to low complex I activity. S-nitrosylation of the Cys39 in the ischemic cells by MitoSNO attenuated the reactivation of Complex I with reperfusion and the resulting lethal burst of ROS [10, 43]. The cardioprotective action of MitoSNO persisted in cardiomyocyte-specific PKG-I KO mice, indicating its independence of the cGMP–PKG pathway [10] (Fig. 1).
sGC activators or stimulators
One major strategy to increase the intracellular pool of cGMP is to activate sGC [18]. NO can induce sGC’s activity upon its binding to the reduced Fe2+ heme moiety on its β-subunit. However, oxidation of the heme moiety under pathological conditions during oxidative stress, such as diabetes, can result in reduced sensitivity of sGC to NO. Also the reduced bioavailability of NO associated with endothelial dysfunction is another factor that can limit the activity of sGC. Two classes of small molecule compounds have been developed to directly target sGC. sGC stimulators increase the catalytic activity of sGC with a reduced Fe2+ heme moiety. These compounds work synergistically with NO. On the other hand, sGC activators can activate the enzyme when the heme moiety is oxidised or missing. sGC activators can also trigger cGMP synthesis independently of NO [18]. Both classes of drugs, sGC activators (e.g. BAY58-2667—Cinaciguat and HMR-1766—Ataciguat) [23, 36, 56] and stimulators (e.g. BAY63-6521—Riociguat, BAY60-4552, and BAY1021189—Vericiguat) [2, 42], have shown promising results in preclinical and clinical studies. Among them, Vericiguat has a dual mode of action. It sensitises sGC to endogenous NO by promoting NO–sGC binding and it also activates sGC independently of NO. Vericiguat has been structurally optimised for chronic use in heart failure (HF) patients, allowing once-a-day dosage with low pharmacokinetic variability [22]. In a Phase IIb dose-finding study, the SOCRATES-REDUCED trial, an exploratory analysis showed that Vericiguat improved left ventricular ejection fraction (EF) and reduced NT-proBNP (biomarker for heart failure) at the highest dose in subjects with reduced ejection fraction heart failure (HFrEF) [25]. Vericiguat entered into a phase III clinical trial, the VICTORIA trial, in 2016 in HFrEF patients [1].
Natriuretic peptides
Natriuretic peptides (NPs) augment the intracellular level of cGMP via pGC [46]. NPs such as ANP and BNP are upregulated to compensate loss of function in failing hearts. Their elevated plasma levels also serve as well-established biomarkers for heart failure. NPs have shown multiple pharmacological effects including diuresis, natriuresis, vasodilation and inhibition of the renin-angiotensin and aldosterone systems. There are a number of preclinical studies showing that elevating NPs results in cardioprotection against I/R injury and in hypertrophy models [8, 13, 46, 55]. Clinically, less data are available, however, the J-WIND-ANP trial showed promising results [35]. A continuous infusion of ANP for 3 days following reperfusion led to a 14.7% reduction in infarct size with reduced total creatine kinase (CK) release (66,459.9 IU/ml per h in the treated group vs. 77,878.9 IU/ml per h in controls) and a small but significant improvement in EF compared to the control group. In 2014, the PARADIGM-HF trial has shown that administration of Sacubitril, a first-in-class neprilysin inhibitor that interferes with NP degradation, resulted in a significant improvement in patients with HFrEF when it was given together with the angiotensin II receptor blocker, Valsartan [32, 41]. Following the successful clinical trials, Sacubitril/Valsartan (Entresto™) was approved for the treatment of HFrEF.
PDE inhibitors
The intracellular pool of cGMP is tightly regulated by PDEs, enzymes degrading cGMP, as an important part of cGMP–PKG pathway. There are 6 different PDE isoforms, PDE 1, 2, 3, 4, 5 and 9, that are expressed in the heart and are responsible for cGMP catabolism in the cardiovascular system. It is reported that PDE5 is predominantly responsible for hydrolysis of cGMP produced by sGC [63, 65]. PKG-I phosphorylates and activates PDE-5 by increasing its affinity to cGMP, thereby enhancing cGMP hydrolysis. This cGMP–PKG–PDE-5 signalling works efficiently as a negative feedback regulation maintaining the physiological cGMP homeostasis. The expression of PDE 5 is very low and mainly confined to smooth muscle cells under physiological conditions but it was found to be upregulated in ischemic and failing myocardium [44, 50, 59]. With such pathological changes, use of a PDE-5 inhibitor such as sildenafil, which is widely prescribed for the treatment of erectile dysfunction, has shown promising results against I/R injury, cardiac hypertrophy and heart failure in both preclinical and clinical settings [14, 20, 26, 38, 62]. A recent study has also demonstrated that co-treatment of a PDE-5 inhibitor, tadalafil, has a synergistic effect with the protection afforded by inhaled NO starting 30 min before reperfusion and continued for 20 min during reperfusion. This additional protection against infarction was accompanied with a significant increase of cardiac cGMP levels [40]. Although the mechanism of its protection is not fully elucidated yet, multiple studies have demonstrated that the cardioprotective effect of PDE-5 inhibitors is PKG pathway-dependent using pharmacological PKG inhibitors or selectively knocking down PKG in cardiomyocytes [15, 54]. A number of small scale clinical studies have shown favourable effects of PDE-5 inhibitors such as improved hemodynamics, left ventricular (LV) diastolic function and right ventricular (RV) systolic function in patients with heart failure with preserved ejection fraction (HFpEF). However, a recent multicentre, double-blinded, randomised, controlled trial, RELAX, failed to confirm a beneficial effect of sildenafil against HFpEF [52]. Based on evidence from prior clinical studies and the limitations of the RELAX trial, the authors suggested that only HF patients with reactive pulmonary hypertension are likely to benefit [34].
Apart from PDE-5, Lee et al. recently suggested PDE9A as a novel therapeutic target against heart failure [37]. PDE9A is expressed in cardiomyocytes and further upregulated by hypertrophy and heart failure. Interestingly, the study showed that PDE9A regulates cGMP produced by the NP–pGC pathway rather than the NO–sGC pathway. Genetic or pharmacological inhibition of PDE9A activity improved cardiac function in mice subjected to pressure overload hypertrophy by severe transverse aortic constriction (TAC). The authors proposed that PDE9A as an alternative therapeutic approach which might be effective alone or in combination with other drugs for treatment of heart failure.
Summary
Despite promising results from many preclinical studies suggesting a cardioprotective effect of cGMP–PKG signalling, a number of clinical studies evaluating GC modulators and PDE 5 inhibitors have failed to show the efficacy in large cohorts. The current difficulty in translating preclinical observation to clinical efficacy might be due to the distinct disease states derived from differences between preclinical animal models and humans [19]. For instance, subjects enrolled in clinical studies evaluating potential therapeutic tools against heart failure are likely complicated with other age-related diseases such as metabolic syndrome and other cardiovascular problems, which are often absent in preclinical animal models. Under such complex pathological condition, the efficacy of GC modulators or PDE-5 inhibitor could be limited due to the reduced sensitivity of GC to NO or the limited availability of NO, as discussed above. Based on our current understanding the complexity of such age-related diseases, employing combination therapy strategy targeting multiple mechanisms involved in the cGMP–PKG pathway, for example, targeting both NO-independent NP–pGC–cGMP and NO-dependent sCG–cGMP pathways, might be able to shed some light in the quest for new therapeutic tools against heart failure.
References
Armstrong PW, Roessig L, Patel MJ, Anstrom KJ, Butler J, Voors AA, Lam CSP, Ponikowski P, Temple T, Pieske B, Ezekowitz J, Hernandez AF, Koglin J, O’Connor CM (2017) A multicenter, randomized, double-blind, placebo-controlled trial of the efficacy and safety of the oral soluble guanylate cyclase stimulator: the VICTORIA trial. JACC Heart Fail https://doi.org/10.1016/j.jchf.2017.08.013
Bice JS, Keim Y, Stasch JP, Baxter GF (2014) NO-independent stimulation or activation of soluble guanylyl cyclase during early reperfusion limits infarct size. Cardiovasc Res 101:220–228. https://doi.org/10.1093/cvr/cvt257
Bueno M, Wang J, Mora AL, Gladwin MT (2013) Nitrite signaling in pulmonary hypertension: mechanisms of bioactivation, signaling, and therapeutics. Antioxid Redox Signal 18:1797–1809. https://doi.org/10.1089/ars.2012.4833
Burgoyne JR, Madhani M, Cuello F, Charles RL, Brennan JP, Schroder E, Browning DD, Eaton P (2007) Cysteine redox sensor in PKGIa enables oxidant-induced activation. Science 317:1393–1397. https://doi.org/10.1126/science.1144318
Burke SG, Wainwright CL, Vojnovic I, Warner T, Watson DG, Furman BL (2006) The effect of NCX4016 [2-acetoxy-benzoate 2-(2-nitroxymethyl)-phenyl ester] on the consequences of ischemia and reperfusion in the streptozotocin diabetic rat. J Pharmacol Exp Ther 316:1107–1114. https://doi.org/10.1124/jpet.105.096339
Burley DS, Ferdinandy P, Baxter GF (2007) Cyclic GMP and protein kinase-G in myocardial ischaemia-reperfusion: opportunities and obstacles for survival signaling. Br J Pharmacol 152:855–869. https://doi.org/10.1038/sj.bjp.0707409
Carnicer R, Crabtree MJ, Sivakumaran V, Casadei B, Kass DA (2013) Nitric oxide synthases in heart failure. Antioxid Redox Signal 18:1078–1099. https://doi.org/10.1089/ars.2012.4824
Charan K, Goyal A, Gupta JK, Yadav HN (2016) Role of atrial natriuretic peptide in ischemic preconditioning-induced cardioprotection in the diabetic rat heart. J Surg Res 201:272–278. https://doi.org/10.1016/j.jss.2015.10.045
Chouchani ET, James AM, Methner C, Pell VR, Prime TA, Erickson BK, Forkink M, Lau GY, Bright TP, Menger KE, Fearnley IM, Krieg T, Murphy MP (2017) Identification and quantification of protein S-nitrosation by nitrite in the mouse heart during ischemia. J Biol Chem 292:14486–14495. https://doi.org/10.1074/jbc.M117.798744
Chouchani ET, Methner C, Nadtochiy SM, Logan A, Pell VR, Ding S, James AM, Cocheme HM, Reinhold J, Lilley KS, Partridge L, Fearnley IM, Robinson AJ, Hartley RC, Smith RA, Krieg T, Brookes PS, Murphy MP (2013) Cardioprotection by S-nitrosation of a cysteine switch on mitochondrial complex I. Nat Med 19:753–759. https://doi.org/10.1038/nm.3212
Costa AD, Garlid KD, West IC, Lincoln TM, Downey JM, Cohen MV, Critz SD (2005) Protein kinase G transmits the cardioprotective signal from cytosol to mitochondria. Circ Res 97:329–336. https://doi.org/10.1161/01.RES.0000178451.08719.5b
Costa AD, Pierre SV, Cohen MV, Downey JM, Garlid KD (2008) cGMP signalling in pre- and post-conditioning: the role of mitochondria. Cardiovasc Res 77:344–352. https://doi.org/10.1093/cvr/cvm050
D’Souza SP, Yellon DM, Martin C, Schulz R, Heusch G, Onody A, Ferdinandy P, Baxter GF (2003) B-type natriuretic peptide limits infarct size in rat isolated hearts via KATP channel opening. Am J Physiol Heart Circ Physiol 284:H1592–H1600. https://doi.org/10.1152/ajpheart.00902.2002
Das A, Durrant D, Salloum FN, Xi L, Kukreja RC (2015) PDE5 inhibitors as therapeutics for heart disease, diabetes and cancer. Pharmacol Ther 147:12–21. https://doi.org/10.1016/j.pharmthera.2014.10.003
Das A, Xi L, Kukreja RC (2008) Protein kinase G-dependent cardioprotective mechanism of phosphodiesterase-5 inhibition involves phosphorylation of ERK and GSK3beta. J Biol Chem 283:29572–29585. https://doi.org/10.1074/jbc.M801547200
Di Filippo C, Monopoli A, Ongini E, Perretti M, D’Amico M (2010) The cardio-protective properties of Ncx-6550, a nitric oxide donating pravastatin, in the mouse. Microcirculation 17:417–426. https://doi.org/10.1111/j.1549-8719.2010.00040.x
Duranski MR, Greer JJ, Dejam A, Jaganmohan S, Hogg N, Langston W, Patel RP, Yet SF, Wang X, Kevil CG, Gladwin MT, Lefer DJ (2005) Cytoprotective effects of nitrite during in vivo ischemia-reperfusion of the heart and liver. J Clin Invest 115:1232–1240. https://doi.org/10.1172/JCI22493
Evgenov OV, Pacher P, Schmidt PM, Hasko G, Schmidt HH, Stasch JP (2006) NO-independent stimulators and activators of soluble guanylate cyclase: discovery and therapeutic potential. Nat Rev Drug Discov 5:755–768. https://doi.org/10.1038/nrd2038
Ferdinandy P, Hausenloy DJ, Heusch G, Baxter GF, Schulz R (2014) Interaction of risk factors, comorbidities, and comedications with ischemia/reperfusion injury and cardioprotection by preconditioning, postconditioning, and remote conditioning. Pharmacol Rev 66:1142–1174. https://doi.org/10.1124/pr.113.008300
Fisher PW, Salloum F, Das A, Hyder H, Kukreja RC (2005) Phosphodiesterase-5 inhibition with sildenafil attenuates cardiomyocyte apoptosis and left ventricular dysfunction in a chronic model of doxorubicin cardiotoxicity. Circulation 111:1601–1610. https://doi.org/10.1161/01.CIR.0000160359.49478.C2
Flogel U, Decking UK, Godecke A, Schrader J (1999) Contribution of NO to ischemia-reperfusion injury in the saline-perfused heart: a study in endothelial NO synthase knockout mice. J Mol Cell Cardiol 31:827–836. https://doi.org/10.1006/jmcc.1998.0921
Follmann M, Ackerstaff J, Redlich G, Wunder F, Lang D, Kern A, Fey P, Griebenow N, Kroh W, Becker-Pelster EM, Kretschmer A, Geiss V, Li V, Straub A, Mittendorf J, Jautelat R, Schirok H, Schlemmer KH, Lustig K, Gerisch M, Knorr A, Tinel H, Mondritzki T, Trubel H, Sandner P, Stasch JP (2017) Discovery of the soluble guanylate cyclase stimulator vericiguat (BAY 1021189) for the treatment of chronic heart failure. J Med Chem 60:5146–5161. https://doi.org/10.1021/acs.jmedchem.7b00449
Fraccarollo D, Galuppo P, Motschenbacher S, Ruetten H, Schafer A, Bauersachs J (2014) Soluble guanylyl cyclase activation improves progressive cardiac remodeling and failure after myocardial infarction. Cardioprotection over ACE inhibition. Basic Res Cardiol 109:421. https://doi.org/10.1007/s00395-014-0421-1
Frankenreiter S, Bednarczyk P, Kniess A, Bork N, Straubinger J, Koprowski P, Wrzosek A, Mohr E, Logan A, Murphy MP, Gawaz M, Krieg T, Szewczyk A, Nikolaev VO, Ruth P, Lukowski R (2017) cGMP-elevating compounds and ischemic conditioning provide cardioprotection against ischemia and reperfusion injury via cardiomyocyte-specific BK channels. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.117.028723
Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, Ponikowski P, Shah SJ, Solomon SD, Kraigher-Krainer E, Samano ET, Muller K, Roessig L, Pieske B, S-R Investigators Coordinators (2015) Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA 314:2251–2262. https://doi.org/10.1001/jama.2015.15734
Guazzi M, Samaja M, Arena R, Vicenzi M, Guazzi MD (2007) Long-term use of sildenafil in the therapeutic management of heart failure. J Am Coll Cardiol 50:2136–2144. https://doi.org/10.1016/j.jacc.2007.07.078
Heusch G (2017) Cardioprotection is alive but remains enigmatic: the nitric oxide-protein kinases-mitochondria signaling axis. Circulation 136:2356–2358. https://doi.org/10.1161/CIRCULATIONAHA.117.031978
Heusch G, Boengler K, Schulz R (2008) Cardioprotection: nitric oxide, protein kinases, and mitochondria. Circulation 118:1915–1919. https://doi.org/10.1161/CIRCULATIONAHA.108.805242
Hunter CJ, Dejam A, Blood AB, Shields H, Kim-Shapiro DB, Machado RF, Tarekegn S, Mulla N, Hopper AO, Schechter AN, Power GG, Gladwin MT (2004) Inhaled nebulized nitrite is a hypoxia-sensitive NO-dependent selective pulmonary vasodilator. Nat Med 10:1122–1127. https://doi.org/10.1038/nm1109
Inserte J, Garcia-Dorado D (2015) The cGMP/PKG pathway as a common mediator of cardioprotection: translatability and mechanism. Br J Pharmacol 172:1996–2009. https://doi.org/10.1111/bph.12959
Inserte J, Hernando V, Ruiz-Meana M, Poncelas-Nozal M, Fernandez C, Agullo L, Sartorio C, Vilardosa U, Garcia-Dorado D (2014) Delayed phospholamban phosphorylation in post-conditioned heart favours Ca2+ normalization and contributes to protection. Cardiovasc Res 103:542–553. https://doi.org/10.1093/cvr/cvu163
Jessup M, Fox KA, Komajda M, McMurray JJ, Packer M (2014) PARADIGM-HF–the experts’ discussion. N Engl J Med 371:e15. https://doi.org/10.1056/NEJMp1410203
Keeble JE, Moore PK (2002) Pharmacology and potential therapeutic applications of nitric oxide-releasing non-steroidal anti-inflammatory and related nitric oxide-donating drugs. Br J Pharmacol 137:295–310. https://doi.org/10.1038/sj.bjp.0704876
Kim GE, Kass DA (2017) Cardiac phosphodiesterases and their modulation for treating heart disease. Handb Exp Pharmacol 243:249–269. https://doi.org/10.1007/164_2016_82
Kitakaze M, Asakura M, Kim J, Shintani Y, Asanuma H, Hamasaki T, Seguchi O, Myoishi M, Minamino T, Ohara T, Nagai Y, Nanto S, Watanabe K, Fukuzawa S, Hirayama A, Nakamura N, Kimura K, Fujii K, Ishihara M, Saito Y, Tomoike H, Kitamura S, JW investigators (2007) Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (J-WIND): two randomised trials. Lancet 370:1483–1493. https://doi.org/10.1016/S0140-6736(07)61634-1
Krieg T, Liu Y, Rutz T, Methner C, Yang XM, Dost T, Felix SB, Stasch JP, Cohen MV, Downey JM (2009) BAY 58-2667, a nitric oxide-independent guanylyl cyclase activator, pharmacologically post-conditions rabbit and rat hearts. Eur Heart J 30:1607–1613. https://doi.org/10.1093/eurheartj/ehp143
Lee DI, Zhu G, Sasaki T, Cho GS, Hamdani N, Holewinski R, Jo SH, Danner T, Zhang M, Rainer PP, Bedja D, Kirk JA, Ranek MJ, Dostmann WR, Kwon C, Margulies KB, Van Eyk JE, Paulus WJ, Takimoto E, Kass DA (2015) Phosphodiesterase 9A controls nitric-oxide-independent cGMP and hypertrophic heart disease. Nature 519:472–476. https://doi.org/10.1038/nature14332
Lewis GD, Lachmann J, Camuso J, Lepore JJ, Shin J, Martinovic ME, Systrom DM, Bloch KD, Semigran MJ (2007) Sildenafil improves exercise hemodynamics and oxygen uptake in patients with systolic heart failure. Circulation 115:59–66. https://doi.org/10.1161/CIRCULATIONAHA.106.626226
Lukowski R, Krieg T, Rybalkin SD, Beavo J, Hofmann F (2014) Turning on cGMP-dependent pathways to treat cardiac dysfunctions: boom, bust, and beyond. Trends Pharmacol Sci 35:404–413. https://doi.org/10.1016/j.tips.2014.05.003
Lux A, Pokreisz P, Swinnen M, Caluwe E, Gillijns H, Szelid Z, Merkely B, Janssens SP (2016) Concomitant phosphodiesterase 5 inhibition enhances myocardial protection by inhaled nitric oxide in ischemia-reperfusion injury. J Pharmacol Exp Ther 356:284–292. https://doi.org/10.1124/jpet.115.227850
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz M, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, Investigators P-HC (2014) Baseline characteristics and treatment of patients in prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure trial (PARADIGM-HF). Eur J Heart Fail 16:817–825. https://doi.org/10.1002/ejhf.115
Methner C, Buonincontri G, Hu CH, Vujic A, Kretschmer A, Sawiak S, Carpenter A, Stasch JP, Krieg T (2013) Riociguat reduces infarct size and post-infarct heart failure in mouse hearts: insights from MRI/PET imaging. PLoS One 8:e83910. https://doi.org/10.1371/journal.pone.0083910
Methner C, Chouchani ET, Buonincontri G, Pell VR, Sawiak SJ, Murphy MP, Krieg T (2014) Mitochondria selective S-nitrosation by mitochondria-targeted S-nitrosothiol protects against post-infarct heart failure in mouse hearts. Eur J Heart Fail 16:712–717. https://doi.org/10.1002/ejhf.100
Nagendran J, Archer SL, Soliman D, Gurtu V, Moudgil R, Haromy A, St Aubin C, Webster L, Rebeyka IM, Ross DB, Light PE, Dyck JR, Michelakis ED (2007) Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation 116:238–248. https://doi.org/10.1161/CIRCULATIONAHA.106.655266
Nakata S, Tsutsui M, Shimokawa H, Suda O, Morishita T, Shibata K, Yatera Y, Sabanai K, Tanimoto A, Nagasaki M, Tasaki H, Sasaguri Y, Nakashima Y, Otsuji Y, Yanagihara N (2008) Spontaneous myocardial infarction in mice lacking all nitric oxide synthase isoforms. Circulation 117:2211–2223. https://doi.org/10.1161/CIRCULATIONAHA.107.742692
Nishikimi T, Maeda N, Matsuoka H (2006) The role of natriuretic peptides in cardioprotection. Cardiovasc Res 69:318–328. https://doi.org/10.1016/j.cardiores.2005.10.001
Oldenburg O, Qin Q, Krieg T, Yang XM, Philipp S, Critz SD, Cohen MV, Downey JM (2004) Bradykinin induces mitochondrial ROS generation via NO, cGMP, PKG, and mitoKATP channel opening and leads to cardioprotection. Am J Physiol Heart Circ Physiol 286:H468–H476. https://doi.org/10.1152/ajpheart.00360.2003
Ongini E, Impagnatiello F, Bonazzi A, Guzzetta M, Govoni M, Monopoli A, Del Soldato P, Ignarro LJ (2004) Nitric oxide (NO)-releasing statin derivatives, a class of drugs showing enhanced antiproliferative and antiinflammatory properties. Proc Natl Acad Sci USA 101:8497–8502. https://doi.org/10.1073/pnas.0401996101
Pell VR, Chouchani ET, Frezza C, Murphy MP, Krieg T (2016) Succinate metabolism: a new therapeutic target for myocardial reperfusion injury. Cardiovasc Res 111:134–141. https://doi.org/10.1093/cvr/cvw100
Pokreisz P, Vandenwijngaert S, Bito V, Van den Bergh A, Lenaerts I, Busch C, Marsboom G, Gheysens O, Vermeersch P, Biesmans L, Liu X, Gillijns H, Pellens M, Van Lommel A, Buys E, Schoonjans L, Vanhaecke J, Verbeken E, Sipido K, Herijgers P, Bloch KD, Janssens SP (2009) Ventricular phosphodiesterase-5 expression is increased in patients with advanced heart failure and contributes to adverse ventricular remodeling after myocardial infarction in mice. Circulation 119:408–416. https://doi.org/10.1161/CIRCULATIONAHA.108.822072
Rassaf T, Totzeck M, Hendgen-Cotta UB, Shiva S, Heusch G, Kelm M (2014) Circulating nitrite contributes to cardioprotection by remote ischemic preconditioning. Circ Res 114:1601–1610. https://doi.org/10.1161/CIRCRESAHA.114.303822
Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, LeWinter MM, Rouleau JL, Bull DA, Mann DL, Deswal A, Stevenson LW, Givertz MM, Ofili EO, O’Connor CM, Felker GM, Goldsmith SR, Bart BA, McNulty SE, Ibarra JC, Lin G, Oh JK, Patel MR, Kim RJ, Tracy RP, Velazquez EJ, Anstrom KJ, Hernandez AF, Mascette AM, Braunwald E, Trial R (2013) Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 309:1268–1277. https://doi.org/10.1001/jama.2013.2024
Rossoni G, Berti M, Colonna VD, Bernareggi M, Del Soldato P, Berti F (2000) Myocardial protection by the nitroderivative of aspirin, NCX 4016: in vitro and in vivo experiments in the rabbit. Ital Heart J 1:146–155
Salloum FN, Chau VQ, Hoke NN, Abbate A, Varma A, Ockaili RA, Toldo S, Kukreja RC (2009) Phosphodiesterase-5 inhibitor, tadalafil, protects against myocardial ischemia/reperfusion through protein-kinase g-dependent generation of hydrogen sulfide. Circulation 120:S31–S36. https://doi.org/10.1161/CIRCULATIONAHA.108.843979
Sangawa K, Nakanishi K, Ishino K, Inoue M, Kawada M, Sano S (2004) Atrial natriuretic peptide protects against ischemia-reperfusion injury in the isolated rat heart. Ann Thorac Surg 77:233–237
Schafer A, Fraccarollo D, Werner L, Bauersachs J (2010) Guanylyl cyclase activator ataciguat improves vascular function and reduces platelet activation in heart failure. Pharmacol Res 62:432–438. https://doi.org/10.1016/j.phrs.2010.06.008
Schulz R, Kelm M, Heusch G (2004) Nitric oxide in myocardial ischemia/reperfusion injury. Cardiovasc Res 61:402–413. https://doi.org/10.1016/j.cardiores.2003.09.019
Schulz R, Wambolt R (1995) Inhibition of nitric oxide synthesis protects the isolated working rabbit heart from ischaemia-reperfusion injury. Cardiovasc Res 30:432–439
Shan X, Quaile MP, Monk JK, French B, Cappola TP, Margulies KB (2012) Differential expression of PDE5 in failing and nonfailing human myocardium. Circ Heart Fail 5:79–86. https://doi.org/10.1161/CIRCHEARTFAILURE.111.961706
Stuehr DJ, Santolini J, Wang ZQ, Wei CC, Adak S (2004) Update on mechanism and catalytic regulation in the NO synthases. J Biol Chem 279:36167–36170. https://doi.org/10.1074/jbc.R400017200
Sun J, Aponte AM, Kohr MJ, Tong G, Steenbergen C, Murphy E (2013) Essential role of nitric oxide in acute ischemic preconditioning: S-nitros(yl)ation versus sGC/cGMP/PKG signaling? Free Radic Biol Med 54:105–112. https://doi.org/10.1016/j.freeradbiomed.2012.09.005
Takimoto E, Champion HC, Li M, Belardi D, Ren S, Rodriguez ER, Bedja D, Gabrielson KL, Wang Y, Kass DA (2005) Chronic inhibition of cyclic GMP phosphodiesterase 5A prevents and reverses cardiac hypertrophy. Nat Med 11:214–222. https://doi.org/10.1038/nm1175
Tsai EJ, Kass DA (2009) Cyclic GMP signaling in cardiovascular pathophysiology and therapeutics. Pharmacol Ther 122:216–238. https://doi.org/10.1016/j.pharmthera.2009.02.009
Wainwright CL, Miller AM, Work LM, Del Soldato P (2002) NCX4016 (NO-aspirin) reduces infarct size and suppresses arrhythmias following myocardial ischaemia/reperfusion in pigs. Br J Pharmacol 135:1882–1888. https://doi.org/10.1038/sj.bjp.0704646
Wallis RM, Corbin JD, Francis SH, Ellis P (1999) Tissue distribution of phosphodiesterase families and the effects of sildenafil on tissue cyclic nucleotides, platelet function, and the contractile responses of trabeculae carneae and aortic rings in vitro. Am J Cardiol 83:3C–12C
Woolfson RG, Patel VC, Neild GH, Yellon DM (1995) Inhibition of nitric oxide synthesis reduces infarct size by an adenosine-dependent mechanism. Circulation 91:1545–1551
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PS is a full-time employee of Bayer AG.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Park, M., Sandner, P. & Krieg, T. cGMP at the centre of attention: emerging strategies for activating the cardioprotective PKG pathway. Basic Res Cardiol 113, 24 (2018). https://doi.org/10.1007/s00395-018-0679-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-018-0679-9