Abstract
Purpose
The potential benefits of vegetarian diets in reducing cognitive impairment have garnered attention due to existing mixed results; hence, our study aims to examine the impact of vegetarianism on cognitive function and neuropsychological status among urban community-dwelling adults from Telangana.
Methods
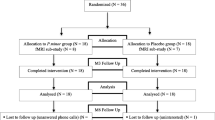
The dietary patterns were self-reported and dietary data collected using a Food Frequency Questionnaire while cognitive function was assessed using Mini-Mental State Examination (MMSE) and depression, anxiety, and stress (DASS-21) questionnaire for psychological measures. Adults (N = 304) aged 40 years and above, who followed either a vegetarian or non-vegetarian diet for at least 6 months prior to data collection, scored MMSE ≥ 19 indicating mild cognitive impairment, and were recruited using convenience sampling.
Results
Among the participants, vegetarians (n = 155) exhibited significantly better mood states compared to non-vegetarians (n = 149), as indicated by lower scores on the DASS subscales for depression (10.0 ± 0.06 vs. 17.0 ± 0.07, p = < 0.001), anxiety (4.0 ± 0.05 vs. 6.0 ± 0.07, p = 0.005), and stress (8.0 ± 0.02 vs. 10.0 ± 0.05, p = 0.007). Vegetarians also demonstrated superior cognitive functioning compared to non-vegetarians, as indicated by higher MMSE scores (26.0 ± 0.04 vs. 24.0 ± 0.03, p = < 0.001). MMSE scores were inversely correlated with depression, anxiety, and stress for vegetarians (ρ = − 0.371, p = 0.000; ρ = − 0.027, p = 0.734; and ρ = − 0.105, p = 0.914), respectively. Similar to the vegetarians group, MMSE scores were negatively correlated with depression (ρ = − 0.059), but the correlation is not significant.
Conclusion
Vegetarianism exerted a positive influence on the cognitive and neuropsychological status of the investigated population. Nevertheless, additional research is required to comprehend the underlying mechanisms that elucidate the long-term effects of vegetarianism and plant-based nutritional interventions on brain health.



Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request. The data cannot be accessed publicly due to specific limitations that could compromise the confidentiality and privacy of the participants.
References
Ferreira D, Correia R, Nieto A, Machado A, Molina Y, Barroso J (2015) Cognitive decline before the age of 50 can be detected with sensitive cognitive measures. Psicothema 27(3):216–222. https://doi.org/10.7334/psicothema2014.192
Salthouse TA (2009) When does age-related cognitive decline begin? Neurobiol Aging 30(4):507–514. https://doi.org/10.1016/j.neurobiolaging.2008.09.023
Ferreira D, Machado A, Molina Y, Nieto A, Correia R, Westman E, Barroso J (2017) Cognitive variability during middle-age: possible association with neurodegeneration and cognitive reserve. Front Aging Neurosci 9:188. https://doi.org/10.3389/fnagi.2017.00188
Gautam P, Cherbuin N, Sachdev PS, Wen W, Anstey KJ (2011) Relationships between cognitive function and frontal grey matter volumes and thickness in middle aged and early old-aged adults: the PATH through life study. Neuroimage 55(3):845–855. https://doi.org/10.1016/j.neuroimage.2011.01.015
Zimprich D, Mascherek A (2010) Five views of a secret: does cognition change during middle adulthood? Eur J Ageing 7(3):135–146. https://doi.org/10.1007/s10433-010-0161-5
Thrippangottur (2011) Census of India. Registrar General and Census Commissioner of India. Retrieved 2023-05-08
Gautham MS, Gururaj G, Varghese M, Benegal V, Rao GN, Kokane A, Chavan BS, Dalal PK, Ram D, Pathak K, Lenin Singh RK, Singh LK, Sharma P, Saha PK, Ramasubramanian C, Mehta RY, Shibukumar TM, Collaborators NMHS (2020) The National Mental Health Survey of India (2016): prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry 66(4):361–372. https://doi.org/10.1177/0020764020907941
Shriraam V, Mahadevan S, Arumugam P (2021) Prevalence and risk factors of diabetes, hypertension and other non-communicable diseases in a tribal population in South India. Indian J Endocrinol Metab 25(4):313–319. https://doi.org/10.4103/ijem.ijem_298_21
Arshad F, Samim MM, Paplikar A, Rajendran S, Kalkonde Y, Alladi S (2021) Vascular cognitive impairment in India: challenges and opportunities for prevention and treatment. Cereb Circ Cogn Behav 3:100034
Ravindranath V, Sundarakumar JS (2021) Changing demography and the challenge of dementia in India. Nat Rev Neurol 17(12):747–758. https://doi.org/10.1038/s41582-021-00565-x
Varalakshmi Manchana DRPT (2023) Group reminiscence for treating geriatric depression in rural community: a randomized controlled trial. J ReAttach Ther Dev Divers 6(9s):83–92
Puri S, Shaheen M, Grover B (2023) Nutrition and cognitive health: a life course approach. Front Public Health 11:1023907. https://doi.org/10.3389/fpubh.2023.1023907
Manchana V (2021) Modern technological intervention advancements for the physically challenged and disabled population. 1st ed.: UK: Cambridge Scholars Publishing. 10, Mediating Cognitive decline and loneliness through physical activity and social connectivity in ageing populations; p 151–185
Goyal MS, Iannotti LL, Raichle ME (2018) Brain nutrition: a life span approach. Annu Rev Nutr 38:381–399. https://doi.org/10.1146/annurev-nutr-082117-051652
Kahleova H, Petersen KF, Shulman GI, Alwarith J, Rembert E, Tura A, Hill M, Holubkov R, Barnard ND (2020) Effect of a low-fat vegan diet on body weight, insulin sensitivity, postprandial metabolism, and intramyocellular and hepatocellular lipid levels in overweight adults: a randomized clinical trial. JAMA Netw Open 3(11):e2025454. https://doi.org/10.1001/jamanetworkopen.2020.25454
Bojang KP, Manchana V (2023) Nutrition and healthy aging: a review. Curr Nutr Rep 16(3):369–375. https://doi.org/10.1007/s13668-023-00473-0
Morris C, Kirwan J, Lally R (2014) Less meat initiatives: an initial exploration of a diet-focused social innovation in transitions to a more sustainable regime of meat provision. Int J Sociol Agric Food 21:189–208
McGrattan AM, McGuinness B, McKinley MC, Kee F, Passmore P, Woodside JV, McEvoy CT (2019) Diet and inflammation in cognitive ageing and Alzheimer’s disease. Curr Nutr Rep 8(2):53–65. https://doi.org/10.1007/s13668-019-0271-4
Tsai JH, Huang CF, Lin MN, Chang CE, Chang CC, Lin CL (2022) Taiwanese vegetarians are associated with lower dementia risk: a prospective cohort study. Nutrients 14(3):588. https://doi.org/10.3390/nu14030588
Lourida I, Soni M, Thompson-Coon J, Purandare N, Lang IA, Ukoumunne OC, Llewellyn DJ (2013) Mediterranean diet, cognitive function, and dementia: a systematic review. Epidemiology 24(4):479–489. https://doi.org/10.1097/EDE.0b013e3182944410
Giem P, Beeson WL, Fraser GE (1993) The incidence of dementia and intake of animal products: preliminary findings from the Adventist Health Study. Neuroepidemiology 12(1):28–36. https://doi.org/10.1159/000110296
Galimberti A, Casiraghi M, Bruni I, Guzzetti L, Cortis P, Berterame NM, Labra M (2019) From DNA barcoding to personalized nutrition: the evolution of food traceability. Curr Opin Food Sci 28:41–48. https://doi.org/10.1016/j.cofs.2019.07.008
Singh M, Arseneault M, Sanderson T, Murthy V, Ramassamy C (2008) Challenges for research on polyphenols from foods in Alzheimer’s disease: bioavailability, metabolism, and cellular and molecular mechanisms. J Agric Food Chem 56(13):4855–4873. https://doi.org/10.1021/jf0735073
Rossi L, Mazzitelli S, Arciello M, Capo CR, Rotilio G (2008) Benefits from dietary polyphenols for brain aging and Alzheimer’s disease. Neurochem Res 33(12):2390–2400. https://doi.org/10.1007/s11064-008-9696-7
Cory H, Passarelli S, Szeto J, Tamez M, Mattei J (2018) The role of polyphenols in human health and food systems: a mini-review. Front Nutr 21(5):87. https://doi.org/10.3389/fnut.2018.00087
Craig WJ (2010) Nutrition concerns and health effects of vegetarian diets. Nutr Clin Pract 25(6):613–620. https://doi.org/10.1177/0884533610385707
Iguacel I, Huybrechts I, Moreno LA, Michels N (2021) Vegetarianism and veganism compared with mental health and cognitive outcomes: a systematic review and meta-analysis. Nutr Rev 79(4):361–381. https://doi.org/10.1093/nutrit/nuaa030
Michalak J, Zhang XC, Jacobi F (2012) Vegetarian diet and mental disorders: results from a representative community survey. Int J Behav Nutr Phys Act 9:67. https://doi.org/10.1186/1479-5868-9-67
Kapoor A, Baig M, Tunio SA, Memon AS, Karmani H (2017) Neuropsychiatric and neurological problems among vitamin B12 deficient young vegetarians. Neurosciences 22(3):228–232. https://doi.org/10.17712/nsj.2017.3.20160445
Agarwal U, Mishra S, Xu J, Levin S, Gonzales J, Barnard ND (2015) A multicenter randomized controlled trial of a nutrition intervention program in a multiethnic adult population in the corporate setting reduces depression and anxiety and improves quality of life: the GEICO study. Am J Health Promot 29(4):245–254. https://doi.org/10.4278/ajhp.130218-QUAN-72
Beezhold BL, Johnston CS, Daigle DR (2010) Vegetarian diets are associated with healthy mood states: a cross-sectional study in seventh day adventist adults. Nutr J 9:26. https://doi.org/10.1186/1475-2891-9-26
Beezhold BL, Johnston CS (2012) Restriction of meat, fish, and poultry in omnivores improves mood: a pilot randomized controlled trial. Nutr J 11:9. https://doi.org/10.1186/1475-2891-11-9
Sofi F, Dinu M, Pagliai G, Cesari F, Gori AM, Sereni A, Becatti M, Fiorillo C, Marcucci R, Casini A (2018) Low-calorie vegetarian versus Mediterranean diets for reducing body weight and improving cardiovascular risk profile: CARDIVEG study (Cardiovascular prevention with vegetarian diet). Circulation 137(11):1103–1113. https://doi.org/10.1161/CIRCULATIONAHA.117.030088
Chiu THT, Pan WH, Lin MN, Lin CL (2018) Vegetarian diet, change in dietary patterns, and diabetes risk: a prospective study. Nutr Diabetes 8(1):12. https://doi.org/10.1038/s41387-018-0022-4
Zelaya AM, Sinibaldi EM (2021) Is vegetarianism a solution for obesity and NCDs? A review. Food Nutr Sci 12(3):249–261. https://doi.org/10.4236/fns.2021.123020
Fraser GE (1999) Associations between diet and cancer, ischemic heart disease, and all-cause mortality in non-Hispanic white California Seventh-day Adventists. Am J Clin Nutr 70(3):532S-538S. https://doi.org/10.1093/ajcn/70.3.532s
Key TJ, Appleby PN, Spencer EA, Travis RC, Allen NE, Thorogood M, Mann JI (2009) Cancer incidence in British vegetarians. Br J Cancer 101(1):192–197. https://doi.org/10.1038/sj.bjc.6605098
Folstein MF, Folstein SE, McHugh PR (1975) ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Iqbal R, Ajayan K, Bharathi AV, Zhang X, Islam S, Soman CR, Merchant AT (2009) Refinement and validation of an FFQ developed to estimate macro- and micronutrient intakes in a south Indian population. Public Health Nutr 12(1):12–18. https://doi.org/10.1017/S1368980008001845
Lovibond SH, Lovibond PF (1995) Manual for the Depression Anxiety Stress Scales (2nd ed.). Sydney: Psychology Foundation of Australia
Longvah T, Ananthan R, Bhaskar K, Venkaiah K (2017) Indian food Composition Tables. National Institute of Nutrition
Shaji S, Bose S, Verghese A (2005) Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry 186:136–140. https://doi.org/10.1192/bjp.186.2.136
Aajami Z, Kazazi L, Toroski M, Bahrami M, Borhaninejad V (2020) Relationship between depression and cognitive impairment among elderly: a cross-sectional study. J Caring Sci 9(3):148–153. https://doi.org/10.34172/jcs.2020.022
Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A (2019) Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr Dis Treat 10(15):1249–1258
Muhammad T, Meher T (2021) Association of late-life depression with cognitive impairment: evidence from a cross-sectional study among older adults in India. BMC Geriatr 21(1):364. https://doi.org/10.1186/s12877-021-02314-7
Institute of Medicine (US) Committee on Military Nutrition Research (1999) The Role of Protein and Amino Acids in Sustaining and Enhancing Performance. Washington (DC): National Academies Press (US). 14, Amino Acid and Protein Requirements: Cognitive Performance, Stress, and Brain Function. Available from: https://www.ncbi.nlm.nih.gov/books/NBK224629/
Burgoyne RD, Haynes LP (2012) Understanding the physiological roles of the neuronal calcium sensor proteins. Mol Brain 5(1):2. https://doi.org/10.1186/1756-6606-5-2
Ma F, Wu T, Zhao J, Song A, Liu H, Xu W, Huang G (2016) Folic acid supplementation improves cognitive function by reducing the levels of peripheral inflammatory cytokines in elderly Chinese subjects with MCI. Sci Rep 6:37486. https://doi.org/10.1038/srep37486
Plevin D, Galletly C (2020) The neuropsychiatric effects of vitamin C deficiency: a systematic review. BMC Psychiatry 20(1):315. https://doi.org/10.1186/s12888-020-02730-w
Moritz B, Schmitz AE, Rodrigues ALS, Dafre AL, Cunha MP (2020) The role of vitamin C in stress-related disorders. J Nutr Biochem 85:108459. https://doi.org/10.1016/j.jnutbio.2020.108459
Shridhar K, Dhillon PK, Bowen L, Kinra S, Bharathi AV, Prabhakaran D, Reddy KS, Ebrahim S (2014) Nutritional profile of Indian vegetarian diets—The Indian Migration Study (IMS). Nutr J 13:55. https://doi.org/10.1186/1475-2891-13-55
Parletta N, Milte CM, Meyer BJ (2013) Nutritional modulation of cognitive function and mental health. J Nutr Biochem 24(5):725–743. https://doi.org/10.1016/j.jnutbio.2013.01.002
Cherbuin N, Anstey KJ (2012) The Mediterranean diet is not related to cognitive change in a large prospective investigation: the PATH through life study. Am J Geriatr Psychiatry 20(7):635–639. https://doi.org/10.1097/JGP.0b013e31823032a9
Qin B, Adair LS, Plassman BL, Batis C, Edwards LJ, Popkin BM, Mendez MA (2015) Dietary patterns and cognitive decline among Chinese older adults. Epidemiology 26(5):758–768. https://doi.org/10.1097/EDE.0000000000000338
Ramey MM, Shields GS, Yonelinas AP (2022) Markers of a plant-based diet relate to memory and executive function in older adults. Nutr Neurosci 25(2):276–285. https://doi.org/10.1080/1028415X.2020.1751506
Krikorian R, Shidler MD, Dangelo K, Couch SC, Benoit SC, Clegg DJ (2012) Dietary ketosis enhances memory in mild cognitive impairment. Neurobiol Aging 33(2):425.e19-425.e27. https://doi.org/10.1016/j.neurobiolaging.2010.10.006
Valls-Pedret C, Sala-Vila A, Serra-Mir M, Corella D, de la Torre R, Martínez-González MÁ, Martínez-Lapiscina EH, Fitó M, Pérez-Heras A, Salas-Salvadó J, Estruch R, Ros E (2015) Mediterranean diet and age-related cognitive decline: a randomized clinical trial. JAMA Intern Med 175(7):1094–1103. https://doi.org/10.1001/jamainternmed.2015.1668
Moore E, Mander A, Ames D, Carne R, Sanders K, Watters D (2012) Cognitive impairment and vitamin B12: a review. Int Psychogeriatr 24(4):541–556. https://doi.org/10.1017/S1041610211002511
Hibbeln JR, Northstone K, Evans J, Golding J (2018) Vegetarian diets and depressive symptoms among men. J Affect Disord 225:13–17. https://doi.org/10.1016/j.jad.2017.07.051
Rosell MS, Lloyd-Wright Z, Appleby PN, Sanders TA, Allen NE, Key TJ (2005) Long-chain n-3 polyunsaturated fatty acids in plasma in British meat-eating, vegetarian, and vegan men. Am J Clin Nutr 82(2):327–334. https://doi.org/10.1093/ajcn.82.2.327
Beezhold B, Radnitz C, Rinne A, DiMatteo J (2015) Vegans report less stress and anxiety than omnivores. Nutr Neurosci 18(7):289–296. https://doi.org/10.1179/1476830514Y.0000000164
Gatto NM, Garcia-Cano J, Irani C, Jaceldo-Siegl K, Liu T, Chen Z, Paul J, Fraser G, Wang C, Lee GJ (2021) Vegetarian dietary patterns and cognitive function among older adults: the adventist health Study-2. J Nutr Gerontol Geriatr 40(4):197–214. https://doi.org/10.1080/21551197.2021.1965939
Zhu A, Yuan C, Pretty J, Ji JS (2022) Plant-based dietary patterns and cognitive function: a prospective cohoranalysis of elderly individuals in China (2008–2018). Brain Behav 12(8):e2670. https://doi.org/10.1002/brb3.2670
Gómez-Pinilla F (2008) Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci 19(7):568–578. https://doi.org/10.1038/nrn2421
Craddock JC, Neale EP, Peoples GE, Probst YC (2019) Vegetarian-based dietary patterns and their relation with inflammatory and immune biomarkers: a systematic review and meta-analysis. Adv Nutr 10(3):433–451. https://doi.org/10.1093/advances/nmy103
Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, Herrup K, Frautschy SA, Finsen B, Brown GC, Verkhratsky A, Yamanaka K, Koistinaho J, Latz E, Halle A, Kummer MP (2015) Neuroinflammation in Alzheimer’s disease. Lancet Neurol 14(4):388–405. https://doi.org/10.1016/S1474-4422(15)70016-5
Soni M, Rahardjo TB, Soekardi R, Sulistyowati Y, Lestariningsih Y-UA, Yesufu-Udechuku A, Irsan A, Hogervorst E (2014) Phytoestrogens and cognitive function: a review. Maturitas 77(3):209–220. https://doi.org/10.1016/j.maturitas.2013.12.010
Fusar-Poli P, Salazar de Pablo G, De Micheli A, Nieman DH, Correll CU, Kessing LV, Pfennig A, Bechdolf A, Borgwardt S, Arango C, van Amelsvoort T (2020) What is good mental health? A scoping review. Eur Neuropsychopharmacol 31:33–46. https://doi.org/10.1016/j.euroneuro.2019.12.105
Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, Akbaraly T (2019) Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry 24(7):965–986. https://doi.org/10.1038/s41380-018-0237-8
Firth J, Gangwisch JE, Borisini A, Wootton RE, Mayer EA (2020) Food and mood: how do diet and nutrition affect mental wellbeing? BMJ 369:m2382. https://doi.org/10.1136/bmj.m2382
Li XD, Cao HJ, Xie SY, Li KC, Tao FB, Yang LS, Zhang JQ, Bao YS (2019) Adhering to a vegetarian diet may create a greater risk of depressive symptoms in the elderly male Chinese population. J Affect Disord 243:182–187. https://doi.org/10.1016/j.jad.2018.09.033
Jain R, Larsuphrom P, Degremont A, Latunde-Dada GO, Philippou E (2022) Association between vegetarian and vegan diets and depression: a systematic review. Nutr Bull 47(1):27–49. https://doi.org/10.1111/nbu.12540
Lee MF, Eather R, Best T (2021) Plant-based dietary quality and depressive symptoms in Australian vegans and vegetarians: a cross-sectional study. BMJ Nutr Prev Health 4(2):479–486. https://doi.org/10.1136/bmjnph-2021-000332
Shen YC, Chang CE, Lin MN, Lin CL (2021) Vegetarian diet is associated with lower risk of depression in Taiwan. Nutrients. https://doi.org/10.3390/nu13041059
Jin Y, Kandula NR, Kanaya AM, Talegawkar SA (2021) Vegetarian diet is inversely associated with prevalence of depression in middle-older aged South Asians in the United States. Ethn Health 26(4):504–511. https://doi.org/10.1080/13557858.2019.1606166
Storz MA, Ronco AL (2023) Adherence to a vegetarian diet is not associated with depression: results from the National health and nutrition examination surveys. Psychiatry Investig 20(4):315–324. https://doi.org/10.30773/pi.2022.0251
Arab A, Mehrabani S, Moradi S, Amani R (2019) The association between diet and mood: A systematicreview of current literature. Psychiatry Res 271:428–437. https://doi.org/10.1016/j.psychres.2018.12.014
Aucoin M, LaChance L, Cooley K, Kidd S (2020) Diet and psychosis: a scoping review. Neuropsychobiology 79(1):20–42. https://doi.org/10.1159/000493399
Fernstrom JD (1994) Dietary amino acids and brain function. J Am Diet Assoc 94(1):71–77. https://doi.org/10.1016/0002-8223(94)92045-1
Refsum H, Yajnik CS, Gadkari M, Schneede J, Vollset SE, Örning L, Guttormsen AB, Joglekar A, Sayyad MG, Ulvik A, Ueland PM (2001) Hyperhomocysteinemia and elevated methylmalonic acid indicate a high prevalence of cobalamin deficiency in Asian Indians. Am J Clin Nutr 74(2):233–241. https://doi.org/10.1093/ajcn/74.2.233
Acknowledgements
The authors express their gratitude for the assistance and support provided by Indian Council of Cultural Research (ICCR) and University of Hyderabad, an Institution of Eminence (IoE) for all the logistical assistance and infrastructure facility to carry out the study, and we extend our since acknowledgements to Ranga Reddy community for participation in data collection. The study is part of the thesis conducted in School of Medical Sciences, University of Hyderabad in India.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
BKP helped in conceptualization of the study, development of the study design, data collection and analysis, and original draft preparation. MVL helped in study conceptualization, methodology design, revision of data analysis, manuscript editing and reviewing, and supervision. All authors were responsible for manuscript revision and also gave their approval for the final manuscript as submitted and have agreed to take responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the University of Hyderabad Institutional Ethics Committee (UH/IEC/2022/390) dated November 30, 2022. Written informed consent was obtained from all participants after explaining the study purpose and ensuring privacy and confidentiality.
Appendix
Appendix
See Tables 1, 2, 3, 4 and 5 here.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bojang, K.P., Manchana, V. Impact of vegetarianism on cognition and neuropsychological status among urban community-dwelling adults in Telangana, South India: a cross-sectional study. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03328-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03328-8