Abstract
Purpose
To assess the relationship of early pregnancy maternal diet quality (DQ) with maternal plasma lipids and indicators of cardiometabolic health, including blood pressure (BP), gestational diabetes mellitus (GDM) and gestational weight gain (GWG).
Methods
Women (n = 215) aged 18–40 years with singleton pregnancies were recruited at 10–20 weeks gestation. Diet quality was assessed by the Dietary Guideline Index, calculated at early ([mean ± SD]) (15 ± 3 weeks) and late (35 ± 2 weeks) pregnancy. Lipidomic analysis was performed, and 698 species across 37 lipid classes were measured from plasma blood samples collected at early (15 ± 3 weeks) and mid (27 ± 3 weeks)-pregnancy. Clinical measures (BP, GDM diagnosis, weight) and blood samples were collected across pregnancy. Multiple linear and logistic regression models assessed associations of early pregnancy DQ with plasma lipids at early and mid-pregnancy, BP at three antenatal visits, GDM diagnosis and total GWG.
Results
Maternal DQ scores ([mean ± SD]) decreased significantly from early (70.7 ± 11.4) to late pregnancy (66.5 ± 12.6) (p < 0.0005). At a false discovery rate of 0.2, early pregnancy DQ was significantly associated with 13 plasma lipids at mid-pregnancy, including negative associations with six triglycerides (TGs); TG(54:0)[NL-18:0] (neutral loss), TG(50:1)[NL-14:0], TG(48:0)[NL-18:0], TG(52:1)[NL-18:0], TG(54:1)[NL-18:1], TG(50:0)[NL-18:0]. No statistically significant associations were found between early pregnancy DQ and BP, GDM or GWG.
Conclusion
Maternal diet did not adhere to Australian Dietary Guidelines. Diet quality was inversely associated with multiple plasma TGs. This study provides novel insights into the relationship between DQ, lipid biomarkers and cardiometabolic health during pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pregnancy is a critical life stage whereby maternal nutrition significantly impacts the immediate and long-term health of the mother and offspring [1]. Globally, unhealthy diets, which are energy dense but lack nutritional quality, comprise a significant behavioural risk factor for the development of chronic disease [2]. Sub-optimal pregnancy nutrition has been linked with increased inter-generational risk factors for cardiometabolic disease, including elevated blood lipids, hypertension, impaired glucose tolerance, and long-term obesity [2,3,4].
Pregnancy has been regarded as a ‘stress test’ for development of cardiometabolic conditions including cardiovascular disease (CVD) [5], a major cause of morbidity and mortality globally [6]. Physiological adaptations that occur with pregnancy progression, including metabolic and haemodynamic changes, increase stress on the maternal cardiovascular system [7]. In addition, common pregnancy complications including preeclampsia and gestational diabetes mellitus (GDM) often driven by obesity and excess gestational weight gain (GWG), determined by pre-pregnancy BMI [7, 8], significantly increase the risk of postpartum maternal CVD and cardiometabolic disease [8, 9]. Roughly two-thirds of all women gain more weight than recommended during pregnancy [10]. Hypertensive disorders of pregnancy affect 10% of pregnancies globally [9], and GDM prevalence is 14% [11], with up to 28% in some pregnant populations [11]. Pregnancy is therefore a unique opportunity to detect and manage risk factors for the development of future maternal CVD [12].
Altered lipid physiology and lipid accumulation will naturally occur with pregnancy progression, in response to physiological adaptations to foetal demands. However, evidence has shown that dyslipidaemia can predict pregnancy complications and adverse health outcomes [13, 14]. Specifically, dyslipidaemia has been linked extensively to the development of CVD [6, 15]. However, assessment of traditional lipid biomarkers including total triglycerides (TGs) and cholesterol does not reflect the complex lipid metabolism which occurs during pregnancy and in response to pregnancy-specific complications such as GDM [16]. Conversely, human lipidomic analysis has emerged as an in-depth and specialised approach to measuring a wide spectrum of lipid species [17]. Since its inception, lipidomic techniques have vastly expanded our understanding of the complexity of lipid dysregulation in cardiometabolic disease [17]. Lipidomic profiling during pregnancy may offer a novel tool for enhancing our understanding of altered lipid metabolism and identification of women who may require early pregnancy lifestyle intervention, such as healthy dietary modification, known to be associated with favourable lipid profiles [18] and lower risk of cardiometabolic disease [19,20,21].
Emerging research has shown that adherence to healthy dietary patterns including the Healthy Eating Index, Mediterranean Diet and the Dietary Approaches to Stop Hypertension (DASH) diet is associated with improved maternal health and reduced risk of pregnancy complications including GDM and gestational hypertension [19, 22]. However, data from mostly prospective cohort studies have shown that adherence to a single, preferred dietary pattern for decreasing risk of adverse pregnancy outcomes is yet to be determined. Further, assessment of diet quality (DQ) defined by adherence to national dietary guidelines and the impact on maternal lipidomic profiling has seldom been explored. The purpose of this study was to assess the association of early pregnancy DQ with maternal plasma lipidomic profiles at early and mid-pregnancy, blood pressure (BP) throughout pregnancy, diagnosis of GDM and total GWG.
Materials and methods
Study population
This study of pregnant women utilises data and biological samples collected as part of the Creatine in Pregnancy Outcomes (CPO) study. A detailed outline of the CPO study protocol and methodology has been previously reported [23]. Ethical approval for the original CPO study was granted in August 2015 from Monash Health (Ref 14140B) and Monash University (Ref 7785). The current study was granted ethical approval in July 2020 by the Deakin University Human Research Ethics Committee (DUHREC) (2020-236). Study procedures followed were in accordance with ethical standards of Monash Health, Monash University and Deakin University’s committees on human experimentation and conformed to the Declaration of Helsinki.
Women attending low-risk antenatal clinics at Monash Health in Melbourne, Australia, were recruited at 10–20 weeks gestation. Monash Health is a large tertiary teaching hospital in metropolitan Melbourne, Australia, and provides antenatal care to over 9000 women per year. Women gave informed, written consent to participate and agreed to have samples collected for the CPO study and biobanked for future research approved by Monash Health. For inclusion, women needed to be aged 18–40 years and classified as having a ‘low risk’, singleton pregnancy, meaning they had no known pre-existing medical or obstetric condition. Women were excluded if they were non-English speaking, had been previously diagnosed with Type 1/ Type 2 diabetes, taking creatine supplements during pregnancy, required high-risk pregnancy care due to underlying or emergent health complications or disclosed ongoing alcohol or drug use during pregnancy. The original CPO study was conducted between 2015 and 2017 and collected data for 284 women.
The current study utilised data from three antenatal visits; the first ([mean ± SD]) (15 ± 3 weeks gestation), third (27 ± 3 weeks gestation) and fifth (35 ± 2 weeks gestation) visits. We defined these timepoints as early, mid- and late pregnancy, respectively, consistent with common terms used to describe pregnancy progression [24, 25]. Demographic data included maternal age, education, gravida, smoking status, sex of the baby and gestational weeks at delivery. Region of birth was defined using birth countries combined into the following categories: Australian/New Zealand (Australia and New Zealand); Asian/South Asian (India, Nepal, China, Afghanistan, Singapore, Sri Lanka, Philippines, Malaysia, Pakistan, Bangladesh, Thailand); European/UK/Canada (Russia, Switzerland, Ireland, UK, Canada, Greece, France, Scotland, Poland, Germany, England); Middle Eastern/African/South American (Lebanon, Israel, Kuwait, Iran, Venezuela, Mauritius, Ghana, Ethiopia, Colombia).
Dietary intake
Dietary intake was assessed using the Cancer Council of Victoria’s (CCV) validated Dietary Questionnaire for Epidemiological Studies (DQES version 2) [26]. Design of the DQES has been described in detail elsewhere [27]. This consisted of 74 items that assessed the frequency of intake across multiple food groups. The DQES is designed to reflect usual intake over the past 12 months. It has been previously validated against 7 day food diaries among reproductive age women [26], showing comparable performance to other widely used food frequency questionnaires [28] and has been used frequently as a validated tool for assessing dietary intake among Australian women [26] and pregnant populations [29, 30]. Women completed the online DQES at early pregnancy ([mean ± SD]) (15 ± 3 weeks gestation) and again at late pregnancy (35 ± 2 weeks gestation). Completion of the DQES at early pregnancy reflected dietary intake during the first trimester of pregnancy and approximately six months leading up to pregnancy. Dietary assessment via the DQES at late pregnancy assessed women’s dietary intake across all of pregnancy specifically. Intake responses from the 74 items are grouped into categories (cereal foods, sweets and snacks, dairy products, meats and fish, fruit and vegetables) and converted to a Dietary Guideline Index (DGI) score, indicating adherence to the Australian Dietary Guidelines (2013) for adults [31].
Diet quality
The DGI has previously been used to assess DQ and risk of cardiometabolic disease in Australian adults [20, 32, 33]. The DGI included 11 food components (Table 1): diet variety; vegetables; fruit; grains and cereals; meat and alternatives; dairy and alternatives; discretionary foods; saturated fat; unsaturated fats; sugar and alcohol. Two additional components, fluid intake and limiting foods high in salt, were not included as the DQES version 2 did not include questions appropriate to score for those items. The DGI at late pregnancy was calculated to adhere to pregnancy specific guidelines which differ for the grains and cereals food group and meat and alternative food group compared to non-pregnancy guidelines. Possible scores for each food category were between 0 and 10 for nine components and 0 and 5 for two components, with a higher score in each category indicating better DQ and higher compliance with the Dietary Guidelines. The total DGI score for each participant ranged between 0 and 110, with a higher score indicating higher adherence to the Dietary Guidelines and, therefore better DQ [20, 32].
Lipidomics
Comprehensive lipid profiling was undertaken, and 698 species across 37 lipid classes were measured. Such extensive lipidomic analysis allows for identification of important biomarkers for assessment of disease risk [34] and enables an understanding of lipid metabolism in pregnancy which would otherwise go undetected. Plasma lipids were analysed in samples collected at early ([mean ± SD) (15 ± 3 weeks) and mid (27 ± 3 weeks)-pregnancy for the current study. Blood was collected in lithium heparin tubes, stored on ice and spun (400 g, 20 min, 4°) to isolate plasma. Lipids were isolated from plasma using lipidomics analysis [35]. In brief, 10 μL of plasma was mixed with 90 μL of butanol/methanol (1:1) and 10 µL of an internal standard mix [35]. Samples were sonicated on a sonicator bath for 1 h, maintained at 25 °C and centrifuged at 13,000g for 10 min and the supernatant transferred into glass vials with inserts for mass spectrometry analysis. Lipidomic analysis was performed using high-performance liquid chromatography in conjunction with an Agilent 6490 QQQ mass spectrometer. Liquid chromatography was done using a Zorbax Eclipse Plus C18 (Agilent Technologies, USA), 1.8 μm, 100 × 2.1 mm column with running solvents comprising of water/acetonitrile/isopropanol at ratios of 50:30:20 and 1:9:90, respectively (A and B), both with 10 mM ammonium formate. The column was maintained at 45 °C during the run and the autosampler controlled at 25 °C. Lipid extracts (1 μL) were injected and separated under a stepped gradient condition with a flow rate of 400 μL/min as previously described [36]. An additional passivation step was performed prior to the run, where 0.5% phosphoric acid in 9:1 acetonitrile/water was run through the HPLC system for an hour and subsequently washed with 1:9 acetonitrile/water overnight. Additional characterisation of phospholipid structures was done as reported previously [36]. Each lipid was integrated manually via Agilent software. Normalisation was done between batches (3) using the pooled plasma QC’s spaced 20 samples in between each sample. This was conducted by median centering, where the median concentration of the QC’s for each batch was used to align the concentrations between each batch. Data from the lipidomic analysis were integrated using MassHunter V8.00 (Agilent, Australia). Relative lipid concentrations were calculated by relating the area under the chromatogram for each lipid species to the corresponding internal standard.
Secondary outcome measures
Systolic and diastolic BP (mm Hg) was measured at each antenatal clinic visit by a research midwife, using Welch Allyn sphygmomanometers with manual cuff inflation and calibrated regularly as per manufacturers instruction. One reading was taken, and if abnormal, three consecutive readings were done at short intervals over 1.5 h, and the average of these readings was recorded. Medical history data (pre-existing medical conditions and GDM diagnosis) were recorded from hospital records. As part of routine care, all women without existing GDM undergo a 75 g oral glucose tolerance test at 24–28 weeks gestation [37]. A diagnosis of GDM was based on the International Association of the Diabetes and Pregnancy study groups (IADPSG) criteria; one of fasting glucose ≥ 5.1 mmol/L; 1 h level ≥ 10 mmol/L; or 2 h level ≥ 8.5 mmol/L [37]. Women’s height (cm) at the first antenatal clinic visit and weight (kg) using calibrated industrial scales at each clinic visit were measured by the same research midwife. Gestational weight gain (GWG) was calculated as weight at the last (fifth) clinic visit minus weight at the first antenatal clinic visit. Body mass index (BMI) (kg/m2) was calculated using World Health Organisation (WHO) BMI criteria for healthy weight, overweight or obese classifications [38].
Statistical analyses
Data were analysed using STATA/SE statistical software version 16.0. Descriptive analyses reported maternal demographics, systolic and diastolic BP, GDM diagnosis and maternal anthropometry as mean ± SD or n (%). Dietary Guideline Index scores were reported as mean ± SD and the score range. Change in DGI scores from early to late pregnancy was assessed via paired t-tests for women who had complete FFQ data at both early and late pregnancy (n = 203). Paired-samples t-tests were conducted to assess mean changes in all lipids between early and mid-pregnancy. Linear and logistic regression models were used to assess associations between total DGI score at early pregnancy with continuous (plasma lipids, BP and GWG) and categorical (GDM diagnosis) outcomes, respectively. Predetermined factors known widely to influence lipids including age [39], BMI [40, 41] and gestational week [42, 43] were included as covariates in the regression models. The model examining the association between early pregnancy diet and mid-pregnancy lipid concentrations also included early pregnancy lipid concentrations as a covariate. Additional covariates included well established factors known to impact (i) BP in pregnancy (smoking [44], age [19, 45], early pregnancy BMI [19, 45] and gestational week at BP measurement [46]); (ii) GDM diagnosis (age [19, 47] early pregnancy BMI [48], country of birth [47]) and (iii) excess GWG ((age [49], early pregnancy BMI [50] and education [49]). These were further included in models assessing association of DGI with pregnancy complications. Finally, the Benjamini–Hochberg method [51] was applied to regression models involving lipid outcomes at both early and mid-pregnancy. This method is widely used for controlling the false discovery rate (FDR) using sequential modified Bonferroni correction for multiple comparisons [51, 52] and has previously been applied to regression models involving the plasma lipidome [36, 39]. A cut-off of FDR of 0.05 and a less conservative level for comparison of 0.2 were used for significance. In all other models (unadjusted and adjusted), statistical significance was set as p < 0.05.
Results
Participants
Of the 286 women enrolled, four women were excluded due to complete missing data, 52 women were excluded due to missing FFQ and anthropometric data and 15 women were excluded as their GDM status was unknown and not available to be retrieved from the electronic medical record system. This left data for 215 included the analyses (Supplemental material). Women were 31.5 ± 3.9 years ([mean ± SD]), and 64% of women were tertiary educated (Table 2). Just over half (54.9%) of all women were born in Australia/New Zealand, over one third (35.8%) were born in Asia/South Asia/Middle East/Africa/South America and 9.3% were born in Europe/UK/Canada. Over half of all women (56.3%) were pregnant with their first baby, and mean gestational age at delivery was 39.2 ± 1.4 weeks. Mean early pregnancy BMI was 25.0 ± 4.6 kg/m2. Women gained 10.9 ± 4.6 kg during pregnancy, and 9.7% of women were diagnosed with GDM. Mean blood pressure measures across pregnancy (systolic/diastolic) were 110/67 ± 12/9.3 mm Hg, 111/67.6 ± 11.0/7.8 mm Hg and 114./70.2 ± 12.1/9.8 mm Hg at early, mid- and late pregnancy, respectively, with a highest overall recorded measure of 122/77.1 ± 1.8/8.7 mm Hg.
Diet quality
Compared to early pregnancy total DGI score ([mean ± SD]) (70.7 ± 11.4), DGI score at late pregnancy was statistically significantly lower (66.5 ± 12.6) (p < 0.0005) (Table 3). Scores for total cereal decreased significantly from early to late pregnancy (3.3 ± 1.2 and 2.5 ± 1.1) (p < 0.0005) and scores for total meat and alternatives also decreased significantly from early to late pregnancy (4.5 ± 1.1 and 3.9 ± 1.4) (p < 0.0005). Scores for total dairy and alternatives increased significantly from early to late pregnancy (6.3 ± 2.5 and 7.1 ± 2.5) (p < 0.0005). Intakes were poor for multiple key individual food components. Scores for limiting discretionary food items were well below the maximum score of 10 at both early and late pregnancy (4.0 ± 4.9 and 4.0 ± 4.9, respectively). DGI scores for vegetables and fruit (scored out of 10) were suboptimal at early and late pregnancy (3.3 ± 1.9 and 3.1 ± 1.8) (p = 0.078) and (7.2 ± 2.8 and 7.5 ± 2.8) (p = 0.128), respectively, where overall scores decreased for vegetables, although this difference was not significant. Further, DGI scores for limiting saturated fats and sugars were suboptimal decreased significantly from early to late pregnancy (3.6 ± 4.5 to 3.0 ± 4.4) (p = 0.018) and (5.1 ± 5.0 to 3.9 ± 4.9) (p ≤ 0.003), respectively.
Plasma lipids
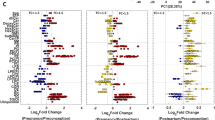
Changes in lipid level were observed for the majority of the lipids, with most increasing significantly from early to mid-pregnancy, while a smaller proportion decreased significantly from early to mid-pregnancy (Supplemental material). There were no statistically significant associations found between DGI score at early pregnancy and lipid outcomes at either early or mid-pregnancy when the model was adjusted for a FDR of 0.05 using the Benjamini–Hochberg procedure (Supplemental material). When we applied a FDR of 0.2, there were multiple statistically significant associations between early pregnancy DGI score and plasma lipids at mid-pregnancy, but not early pregnancy. We run an unadjusted model for all lipids and found that only one lipid (LPCO221) reached significance at a FDR of 0.2, despite not being significant in the adjusted model (data not presented). There was no significant association found in unadjusted models at a FDR of 0.05. Figure 1 presents associations between DGI score at early pregnancy with 698 lipid species at mid-pregnancy. Under the FDR of 0.2, significant associations were found for 13 of the 698 lipids. These significant associations are further summarised in Table 4. Total DGI score at early pregnancy was significantly associated with seven plasma TGs (out of 113 total TG species) at mid-pregnancy, six of which were negative associations. Three TGs contained the 18:0 saturated fatty acid stearic acid ((TG54:0)[NL18:0]; (TG48:0)[NL18:0]); (TG50:0)[NL18:0]). Total DGI score was significantly positively associated with one unsaturated fatty acid ((TG52:4)[NL16:1]), palmitoleic acid.
Associations of early pregnancy diet quality (diet quality assessed by total dietary guideline index score; the model included the Benjamini–Hochberg procedure applied at a FDR of 20%; linear regression adjusted for early pregnancy plasma lipid levels, maternal age, BMI and gestational week) with mid-pregnancy plasma lipids
Blood pressure, gestational diabetes and gestational weight gain
A statistically significant inverse association between DGI score and diastolic BP at late pregnancy was found (−0.14 mm Hg, 95% CI −0.26 −0.02, p = 0.028) (Table 5). No statistically significant associations were found between DGI score at early pregnancy with BP at any time point, GDM diagnosis (26–28 weeks gestation) or total GWG.
Discussion
To our knowledge, this study was the first to explore the relationship between the DGI and maternal lipids, utilising lipidomics. Our findings provide novel insights into the potential impact of early pregnancy diet on important lipid biomarkers. We also provide a unique assessment of DQ across pregnancy, and its association with important pregnancy outcomes as markers of maternal cardiometabolic health. Pregnancy has been regarded a ‘missed opportunity’ for CVD prevention [53]. The novel and comprehensive application of lipidomic analysis in our study has shown it is possible to identify abnormalities across an extensive range of plasma lipids in pregnancy, which would otherwise go undetected.
The relationship between dietary guideline adherence and maternal lipid profile was strongest for the TG lipid species when the model was adjusted for a FDR of 0.2. A higher total DGI score at early pregnancy was associated with lower levels of six TGs at mid-pregnancy (27 ± 3 weeks gestation), all containing saturated and monounsaturated long-chain fatty acid tails. Specific NL observations with these lipids highlighted observing fatty acid 14:0, 18:0 and 18:1 within these TG headgroups. Whilst past research has shown that saturated fatty acids containing 12–16 carbon atoms have the greatest effect on LDL cholesterol concentration and subsequent CVD risk [54], stearic acid has been shown to be a major contributor to development of ischemic heart disease [54, 55], inflammation and lipotoxicity [54]. Further, a significant, positive association was found between total DGI score and one monounsaturated TG, palmitoleic acid (16:1). The link between palmitoleic acid and cardiometabolic health is less clear. However, epidemiological studies have linked palmitoleic acid to cholesterol metabolism, increased insulin sensitivity and glucose tolerance [56]. High dietary intakes of palmitoleic acid have also been shown to be associated with lower blood LDL cholesterol concentrations [54, 57]. Our findings therefore suggest that healthier dietary intakes during pregnancy may have a potential role in modifying TG levels during a critical period when women are vulnerable to dyslipidaemia. Whilst further work is needed to understand the complex relationships between early pregnancy diet and TG levels, in the context of pregnancy-related cardiometabolic health, our findings have revealed the usefulness of utilising lipidomic assessment in examining this relationship.
The importance of dietary intakes which adhere to dietary guidelines during pregnancy extends beyond the need to support optimal growth and development of the foetus, but importantly, to positively impact maternal health. Recent evidence has shown that maternal dyslipidaemia is linked with multiple, adverse maternal and foetal outcomes [53, 58, 59]. Specifically in relation to TGs, elevated saturated/low unsaturated levels have been shown to predict GDM in the few studies that have used lipidomics to quantify lipid profiles in pregnancy [16, 60]. The impact of dyslipidaemia on maternal health can also persist far beyond pregnancy. For example, data from the Generation R study, (n = 5690) assessed early pregnancy maternal lipid profiles at 13 weeks gestation and found that TG and remnant cholesterol levels in early pregnancy were associated with long-term postpartum hypertension at 6 and 9 years [13]. Therefore, pregnancy is a unique life-stage which offers an opportunity to identify and appropriately manage, risk factors for current and future cardiometabolic disease in the clinical setting.
We found that DQ scores reflected low adherence to the Australian Dietary Guidelines, findings similar to other studies which have assessed dietary intake during pregnancy [61,62,63] and across non-pregnant populations [64]. In our study, intake of fruit and vegetables and discretionary food items did not adhere to guidelines. Whilst many barriers to implementation of dietary guidelines during pregnancy have been identified, including pregnancy symptoms such as fatigue and nausea [63, 65] inadequate provision of nutrition counselling from antenatal healthcare providers [65, 66] and a lack of knowledge regarding healthy eating during pregnancy [61, 67], adherence to dietary guidelines assessed via DQ indices has been consistently shown to reduce the risk of cardiometabolic disease [32, 68]. This indicates the overall potential long-term benefit of achieving dietary intakes which adhere to dietary guidelines and underpins pregnancy a critical period. Pregnancy care practices should ensure women are adequately supported to achieve optimal dietary intakes for both short- and long-term health benefit.
Aside from an association between DQ and diastolic BP at late pregnancy, we found no other significant associations between DQ and BP or GDM. Previous studies have shown a reduced risk of GDM with dietary intakes high in fruit and vegetables, whole grains and legumes, yet overall, findings have been mixed [69]. In the only systematic review and meta-analysis to date to have evaluated the impact of DQ using defined adherence to dietary guidelines during preconception and pregnancy on adverse perinatal outcomes [22], pooled data from 33 prospective cohort studies showed that higher DQ was associated with lower risk for GDM and preeclampsia [22]. Specifically, the Mediterranean Diet and the Dietary Approaches to Stop Hypertension (DASH) diets have shown promising results in reducing risk for pregnancy complications, including gestational hypertension. They have previously been associated with improved glucose and lipid metabolism and with lower systolic and diastolic BP [19, 70]. Variation in dietary approaches across DQ assessment (e.g. Mediterranean diet, Prime Diet Quality Score, the Alternative Healthy Eating Index and the Nordic Diet) points to the need for further large prospective cohort and population studies which assess DQ with pregnancy outcomes, to determine a preferred dietary pattern for use in early pregnancy interventions.
We found no association between DQ at early pregnancy and total GWG, a finding consistent with the literature to date reporting this relationship [22]. Perhaps not surprisingly, overall energy intake rather than DQ has been suggested to be the main driver of GWG during pregnancy [22, 71]. Excess GWG is a significant contributing factor to postpartum weight retention [72] and should be routinely monitored as part of screening for risk factors which impact women’s cardiometabolic health during pregnancy.
Strengths and limitations
A major strength of our study was the utilisation of comprehensive human lipidomic analysis. This robust method has enabled insights into the potential impact of diet on lipid metabolism at the molecular level in pregnant women. This was also the first study to our knowledge, to have assessed the relationship between DQ and maternal plasma lipidomics during pregnancy, including measures across two trimesters. An additional strength of this study was using the Australian DGI to calculate DQ at both early and late pregnancy. Dietary intake assessment has shifted from evaluating individual nutrient intake to whole foods and food patterns [73] to account for important interactions of nutrients and non-nutrient components [73]. Therefore, a major strength of the DGI is that it is a validated, food-based index and is translatable to public health messages related to the whole diet [74]. Our study also has some limitations. Recruitment of a high proportion (64%) of tertiary educated women with low-risk pregnancies means that findings are not generalizable to all pregnant women, especially those at ‘high risk’ of maternal complications. Assessment of DQ in less educated populations would enable important identification of vulnerable pregnant women, as poorer DQ may be expected in women of lower socioeconomic status and lower education level. Future research might also recruit women with more complicated pregnancies or women who are at high risk for adverse pregnancy outcomes, specifically women with a pre-pregnancy BMI > 30 kg/m2. A further limitation was the use of self-reported dietary data which may be prone to recall bias or social desirability (e.g. overreported fruit and vegetable intake). However, as mean DGI scores of healthy foods including fruit and vegetables fell short of meeting dietary guidelines, this would suggest that women did not overreport intake of healthy foods. The DQES is commonly used to assess usual intake over the past 12 months and despite having been previously validated against weighed food records, it may not entirely reflect usual dietary intake due to recall of intake over a relatively long timeframe. Further, we did not account for women’s physical activity levels in our study, which is important when considering the effect on plasma TGs. We recognise that there is a need to consider the effect of lifestyle factors including physical activity in interpreting lipidomic profiles in pregnancy, as physical activity has shown positive effects on lowering fasting and postprandial blood glucose levels and blood triglyceride concentrations [75]. Finally, as this was a low-risk sample of pregnant women without serious complications, we could not assess associations of DQ with preeclampsia. However, including BP outcomes across pregnancy was an important aspect of our study as BP monitoring of levels below clinical thresholds of gestational hypertension or preeclampsia is still important in the assessment of overall CVD-related health.
Conclusions
This study has offered novel insight into the impact of maternal diet on important lipid biomarkers in pregnant women. Further work which focuses on lipidomic analysis in early pregnancy to determine the best dietary approaches for targeting maternal lipid metabolism and cardiometabolic health in pregnancy is needed. Our analyses highlight the sensitivity of TGs to dietary intakes during pregnancy. Given the established relationships between TG metabolism and cardiometabolic health, our findings suggest that comprehensive analysis of TGs during pregnancy could be of benefit in early antenatal assessment. Future studies which assess maternal cardiometabolic health outcomes in relation to modifiable factors are needed.
Data availability
Data described in the manuscript, code book, and analytic code will be made available upon request pending reasonable application and approval.
Abbreviations
- BP:
-
Blood pressure
- GWG:
-
Gestational weight gain
- BMI:
-
Body Mass Index
- DGI:
-
Dietary Guideline Index
- GDM:
-
Gestational diabetes mellitus
- CVD:
-
Cardiovascular disease
- DQ:
-
Diet quality
- FFQ:
-
Food frequency questionnaire
- TG:
-
Triglyceride
References
Fernández-Gómez E, Luque-Vara T, Moya-Fernández PJ, López-Olivares M, Gallardo-Vigil MÁ, Enrique-Mirón C (2020) Factors influencing dietary patterns during pregnancy in a culturally diverse society. Nutrients 12(11):3242
Wilkins E, Wickramasinghe K, Pullar J, Demaio AR, Roberts N, Perez-Blanco K-M, Noonan K, Townsend N (2021) Maternal nutrition and its intergenerational links to non-communicable disease metabolic risk factors: a systematic review and narrative synthesis. J Health Popul Nutr 40(1):20. https://doi.org/10.1186/s41043-021-00241-2
Pasternak Y, Aviram A, Poraz I, Hod M (2013) Maternal nutrition and offspring’s adulthood NCD’s: a review. J Matern Fetal Neonatal Med 26(5):439–444. https://doi.org/10.3109/14767058.2012.745505
Riaz M, Shaikh F, Fawwad A, Hakeem R, Shera AS, Hitman GA, Bhowmik B, do Vale Moreira NC, Basit A, Hussain A (2018) Maternal nutrition during early pregnancy and cardiometabolic status of neonates at birth. J Diabetes Res 2018:7382946. https://doi.org/10.1155/2018/7382946
Hauspurg A, Ying W, Hubel CA, Michos ED, Ouyang P (2018) Adverse pregnancy outcomes and future maternal cardiovascular disease. Clin Cardiol 41(2):239–246. https://doi.org/10.1002/clc.22887
Kaneko H, Itoh H, Kiriyama H, Kamon T, Fujiu K, Morita K, Michihata N, Jo T, Takeda N, Morita H, Yasunaga H, Komuro I (2021) Lipid profile and subsequent cardiovascular disease among young adults aged < 50 years. Am J Cardiol 142:59–65. https://doi.org/10.1016/j.amjcard.2020.11.038
Ramlakhan KP, Johnson MR, Roos-Hesselink JW (2020) Pregnancy and cardiovascular disease. Nat Rev Cardiol 17(11):718–731. https://doi.org/10.1038/s41569-020-0390-z
Grieger JA, Hutchesson MJ, Cooray SD, Bahri Khomami M, Zaman S, Segan L, Teede H, Moran LJ (2021) A review of maternal overweight and obesity and its impact on cardiometabolic outcomes during pregnancy and postpartum. Ther Adv Reprod Health 15:2633494120986544. https://doi.org/10.1177/2633494120986544
Siritharan SS, Henry A, Gow ML, Roberts LM, Yao A, Ojurovic M, O’Sullivan AJ (2021) Maternal macro- and micronutrient intake six months after hypertensive versus normotensive pregnancy: is poor diet quality contributing to future cardiometabolic disease risk? Pregnancy Hypertension 23:196–204. https://doi.org/10.1016/j.preghy.2020.11.002
Whitaker KM, Becker C, Healy H, Wilcox S, Liu J (2020) Women’s report of health care provider advice and gestational weight gain: a systematic review. J Womens Health 30(1):73–89. https://doi.org/10.1089/jwh.2019.8223
Nguyen CL, Pham NM, Binns CW, Duong DV, Lee AH (2018) Prevalence of gestational diabetes mellitus in Eastern and Southeastern Asia: a systematic review and meta-analysis. J Diabetes Res 2018:6536974. https://doi.org/10.1155/2018/6536974
Thong EP, Ghelani DP, Manoleehakul P, Yesmin A, Slater K, Taylor R, Collins C, Hutchesson M, Lim SS, Teede HJ, Harrison CL, Moran L, Enticott J (2022) Optimising cardiometabolic risk factors in pregnancy: a review of risk prediction models targeting gestational diabetes and hypertensive disorders. J Cardiovasc Dev Dis 9(2):55
Adank MC, Benschop L, Peterbroers KR, Smak Gregoor AM, Kors AW, Mulder MT, Schalekamp-Timmermans S, Roeters Van Lennep JE, Steegers EAP (2019) Is maternal lipid profile in early pregnancy associated with pregnancy complications and blood pressure in pregnancy and long term postpartum? Am J Obstet Gynecol 221(2):150.e151-150.e113. https://doi.org/10.1016/j.ajog.2019.03.025
Chen Q, Chen H, Xi F, Sagnelli M, Zhao B, Chen Y, Yang M, Xu D, Jiang Y, Chen G, Luo Q (2020) Association between maternal blood lipids levels during pregnancy and risk of small-for-gestational-age infants. Sci Rep 10(1):19865. https://doi.org/10.1038/s41598-020-76845-1
Gomez-Delgado F, Katsiki N, Lopez-Miranda J, Perez-Martinez P (2021) Dietary habits, lipoprotein metabolism and cardiovascular disease: from individual foods to dietary patterns. Crit Rev Food Sci Nutr 61(10):1651–1669. https://doi.org/10.1080/10408398.2020.1764487
Rahman ML, Feng Y-CA, Fiehn O, Albert PS, Tsai MY, Zhu Y, Wang X, Tekola-Ayele F, Liang L, Zhang C (2021) Plasma lipidomics profile in pregnancy and gestational diabetes risk: a prospective study in a multiracial/ethnic cohort. BMJ Open Diabetes Res Care 9(1):e001551. https://doi.org/10.1136/bmjdrc-2020-001551
Lai M, Al Rijjal D, Röst HL, Dai FF, Gunderson EP, Wheeler MB (2020) Underlying dyslipidemia postpartum in women with a recent GDM pregnancy who develop type 2 diabetes. Elife. https://doi.org/10.7554/eLife.59153
Ushula TW, Mamun A, Darssan D, Wang WYS, Williams GM, Whiting SJ, Najman JM (2022) Dietary patterns and the risk of abnormal blood lipids among young adults: a prospective cohort study. Nutr Metab Cardiovasc Dis 32(5):1165–1174. https://doi.org/10.1016/j.numecd.2022.01.030
Li M, Grewal J, Hinkle SN, Yisahak SF, Grobman WA, Newman RB, Skupski DW, Chien EK, Wing DA, Grantz KL, Zhang C (2021) Healthy dietary patterns and common pregnancy complications: a prospective and longitudinal study. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab145
Livingstone K, McNaughton S (2016) Diet quality is associated with obesity and hypertension in Australian adults: a cross sectional study. BMC Public Health. https://doi.org/10.1186/s12889-016-3714-5
Glenn AJ, Hernández-Alonso P, Kendall CWC, Martínez-González MÁ, Corella D, Fitó M, Martínez JA, Alonso-Gómez ÁM, Wärnberg J, Vioque J, Romaguera D, López-Miranda J, Estruch R, Tinahones FJ, Lapetra J, Serra-Majem JL, Bueno-Cavanillas A, Tur JA, Celada SR, Pintó X, Delgado-Rodríguez M, Matía-Martín P, Vidal J, Mas-Fontao S, Daimiel L, Ros E, Jenkins DJA, Toledo E, Sorlí JV, Castañer O, Abete I, Rodriguez AM, Barceló OF, Oncina-Canovas A, Konieczna J, Garcia-Rios A, Casas R, Gómez-Pérez AM, Santos-Lozano JM, Vazquez-Ruiz Z, Portolés O, Schröder H, Zulet MA, Eguaras S, Lete IS, Zomeño MD, Sievenpiper JL, Salas-Salvadó J (2021) Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin Nutr 40(5):2825–2836. https://doi.org/10.1016/j.clnu.2021.03.016
Yu Y, Hardy I, Sun W, Dean F, Zhou Y, Feng C, Ouyang F, Marc I, Fraser W, Dubois L (2021) Association between diet quality during preconception or pregnancy and adverse perinatal outcomes: a systematic review and meta-analysis. Authorea Preprints. https://doi.org/10.22541/au.163251147.74307797/v1
De Guingand DL, Ellery SJ, Davies-Tuck ML, Dickinson H (2019) Creatine and pregnancy outcomes, a prospective cohort study in low-risk pregnant women: study protocol. BMJ Open 9(1):e026756. https://doi.org/10.1136/bmjopen-2018-026756
Chang S-R, Lin W-A, Chang T-C, Lin H-H, Lee C-N, Lin M-I (2021) Risk factors for stress and urge urinary incontinence during pregnancy and the first year postpartum: a prospective longitudinal study. Int Urogynecol J 32(9):2455–2464. https://doi.org/10.1007/s00192-021-04788-w
Young M, Nguyen P, Khuong LQ, Tran L, Tandon S, Martorell R, Ramakrishnan U (2022) Maternal hemoglobin concentrations across pregnancy and child health and development from birth through 6 y. Curr Dev Nutr 6(Supplement_1):576–583. https://doi.org/10.1093/cdn/nzac067.086
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G (2000) The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 24(6):576–583. https://doi.org/10.1111/j.1467-842X.2000.tb00520.x
Ireland P, Jolley D, Giles G, O’Dea K, Powles J, Rutishauser I, Wahlqvist ML, Williams J (1994) Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr 3(1):19–31
Schoenaker DAJM, Soedamah-Muthu SS, Callaway LK, Mishra GD (2015) Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: results from an Australian population-based prospective cohort study. Diabetologia 58(12):2726–2735. https://doi.org/10.1007/s00125-015-3742-1
Hure A, Young A, Smith R, Collins C (2009) Diet and pregnancy status in Australian women. Public Health Nutr 12(6):853–861. https://doi.org/10.1017/S1368980008003212
Lee A, Muggli E, Halliday J, Lewis S, Gasparini E, Forster D (2018) What do pregnant women eat, and are they meeting the recommended dietary requirements for pregnancy? Midwifery 67:70–76. https://doi.org/10.1016/j.midw.2018.09.005
Council NHaMR (2013) Eat for health: Australian dietary guidelines. Canberra. https://www.eatforhealth.gov.au/guidelines
Livingstone KM, McNaughton SA (2018) Association between diet quality, dietary patterns and cardiometabolic health in Australian adults: a cross-sectional study. Nutr J 17(1):19–19. https://doi.org/10.1186/s12937-018-0326-1
McNaughton SA, Dunstan DW, Ball K, Shaw J, Crawford D (2009) Dietary quality is associated with diabetes and cardio-metabolic risk factors. J Nutr 139(4):734–742. https://doi.org/10.3945/jn.108.096784
Beyene HB, Olshansky G, Giles C, Huynh K, Cinel M, Mellett NA, Smith AAT, Shaw JE, Magliano DJ, Meikle PJ (2021) Lipidomic signatures of changes in adiposity: a large prospective study of 5849 adults from the Australian diabetes. Obesity and Lifestyle Study. Metabolites 11(9):646. https://doi.org/10.3390/metabo11090646
Alshehry ZH, Barlow CK, Weir JM, Zhou Y, McConville MJ, Meikle PJ (2015) An efficient single phase method for the extraction of plasma lipids. Metabolites 5(2):389–403. https://doi.org/10.3390/metabo5020389
Huynh K, Barlow CK, Jayawardana KS, Weir JM, Mellett NA, Cinel M, Magliano DJ, Shaw JE, Drew BG, Meikle PJ (2019) High-throughput plasma lipidomics: detailed mapping of the associations with cardiometabolic risk factors. Cell Chem Biol 26(1):71-84.e74. https://doi.org/10.1016/j.chembiol.2018.10.008
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (2017) Diagnosis of gestational diabetes mellitus (GDM). https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Diagnosis-of-GDM-(C-Obs-7)-review-July-2017.pdf?ext=.pdf. Accessed 28 Aug 2023
H. R, M. R (2017) Obesity: definitions and measurement. https://ourworldindata.org/obesity#definitions-measurement. Accessed 16 June 2021
Mousa A, Naderpoor N, Mellett N, Wilson K, Plebanski M, Meikle PJ, de Courten B (2019) Lipidomic profiling reveals early-stage metabolic dysfunction in overweight or obese humans. Biochim Biophys Acta (BBA) Mol Cell Biol Lipids 1864(3):335–343. https://doi.org/10.1016/j.bbalip.2018.12.014
Farias D, Franco-Sena A, Vilela A, Lepsch J, Mendes R, Kac G (2016) Lipid changes throughout pregnancy according to pre-pregnancy BMI: results from a prospective cohort. BJOG Int J Obstetr Gynaecol 123(4):570–578. https://doi.org/10.1111/1471-0528.13293
Geraghty AA, Alberdi G, O’Sullivan EJ, O’Brien EC, Crosbie B, Twomey PJ, McAuliffe FM (2017) Maternal and fetal blood lipid concentrations during pregnancy differ by maternal body mass index: findings from the ROLO study. BMC Pregnancy Childbirth 17(1):360. https://doi.org/10.1186/s12884-017-1543-x
Wang J, Li Z, Lin L (2019) Maternal lipid profiles in women with and without gestational diabetes mellitus. Medicine (Baltimore) 98(16):e15320. https://doi.org/10.1097/md.0000000000015320
Geraghty AA, Alberdi G, O’Sullivan EJ, O’Brien EC, Crosbie B, Twomey PJ, McAuliffe FM (2016) Maternal blood lipid profile during pregnancy and associations with child adiposity: findings from the ROLO study. PLOS ONE 11(8):e0161206. https://doi.org/10.1371/journal.pone.0161206
Hutcheon JA, Lisonkova S, Joseph KS (2011) Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 25(4):391–403. https://doi.org/10.1016/j.bpobgyn.2011.01.006
Garovic VD, Dechend R, Easterling T, Karumanchi SA, Baird SM, Magee LA, Rana S, Vermunt JV, August P (2022) Hypertension in pregnancy: diagnosis, blood pressure goals, and pharmacotherapy: a scientific statement from the American Heart Association. Hypertension 79(2):e21–e41. https://doi.org/10.1161/HYP.0000000000000208
Shen M, Tan H, Zhou S, Smith GN, Walker MC, Wen SW (2017) Trajectory of blood pressure change during pregnancy and the role of pre-gravid blood pressure: a functional data analysis approach. Sci Rep 7(1):6227. https://doi.org/10.1038/s41598-017-06606-0
Du Y, Rafferty AR, McAuliffe FM, Wei L, Mooney C (2022) An explainable machine learning-based clinical decision support system for prediction of gestational diabetes mellitus. Sci Rep 12(1):1170. https://doi.org/10.1038/s41598-022-05112-2
Chu SY, Callaghan WM, Kim SY, Schmid CH, Lau J, England LJ, Dietz PM (2007) Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care 30(8):2070–2076. https://doi.org/10.2337/dc06-2559a
Faucher MA, Barger MK (2015) Gestational weight gain in obese women by class of obesity and select maternal/newborn outcomes: a systematic review. Women and Birth 28(3):e70–e79. https://doi.org/10.1016/j.wombi.2015.03.006
Gilmore LA, Klempel-Donchenko M, Redman LM (2015) Pregnancy as a window to future health: excessive gestational weight gain and obesity. Semin Perinatol 39(4):296–303. https://doi.org/10.1053/j.semperi.2015.05.009
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc Ser B (Methodol) 57(1):289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x
Haynes W (2013) Benjamini–Hochberg method. In: Dubitzky W, Wolkenhauer O, Cho K-H, Yokota H (eds) Encyclopedia of systems biology. Springer New York, New York, NY, pp 78–78
Lumsden RH, Pagidipati N (2022) Management of cardiovascular risk factors during pregnancy. Heart. https://doi.org/10.1136/heartjnl-2021-319606
Shramko VS, Polonskaya YV, Kashtanova EV, Stakhneva EM, Ragino YI (2020) The short overview on the relevance of fatty acids for human cardiovascular disorders. Biomolecules 10(8):1127. https://doi.org/10.3390/biom10081127
Praagman J, Vissers LET, Mulligan AA, Laursen ASD, Beulens JWJ, van der Schouw YT, Wareham NJ, Hansen CP, Khaw KT, Jakobsen MU, Sluijs I (2019) Consumption of individual saturated fatty acids and the risk of myocardial infarction in a UK and a Danish cohort. Int J Cardiol 279:18–26. https://doi.org/10.1016/j.ijcard.2018.10.064
Tricò D, Mengozzi A, Nesti L, Hatunic M, Gabriel Sanchez R, Konrad T, Lalić K, Lalić NM, Mari A, Natali A (2020) Circulating palmitoleic acid is an independent determinant of insulin sensitivity, beta cell function and glucose tolerance in non-diabetic individuals: a longitudinal analysis. Diabetologia 63(1):206–218. https://doi.org/10.1007/s00125-019-05013-6
Frigolet ME, Gutiérrez-Aguilar R (2017) The role of the novel lipokine palmitoleic acid in health and disease. Adv Nutr 8(1):173s–181s. https://doi.org/10.3945/an.115.011130
Lin X-h, Wu D-d, Li C, Xu Y-j, Gao L, Lass G, Zhang J, Tian S, Ivanova D, Tang L, Chen L, Ding R, Liu X-m, Han M, Fan J-x, Li X-f, Sheng J-z, O’Byrne KT, Huang H-f (2018) Maternal high triglyceride levels during early pregnancy and risk of preterm delivery: a retrospective cohort study. J Clin Endocrinol Metab 104(4):1249–1258. https://doi.org/10.1210/jc.2018-01372
Zhu H, He D, Liang N, Lai A, Zeng J, Yu H (2020) High serum triglyceride levels in the early first trimester of pregnancy are associated with gestational diabetes mellitus: a prospective cohort study. J Diabetes Investig 11(6):1635–1642. https://doi.org/10.1111/jdi.13273
Begum H, Li B, Shui G, Cazenave-Gassiot A, Soong R, Ong RT-H, Little P, Teo Y-Y, Wenk MR (2016) Discovering and validating between-subject variations in plasma lipids in healthy subjects. Sci Rep 6(1):19139. https://doi.org/10.1038/srep19139
Bookari K, Yeatman H, Williamson M (2017) Falling short of dietary guidelines—what do Australian pregnant women really know? A cross sectional study. Women Birth 30(1):9–17. https://doi.org/10.1016/j.wombi.2016.05.010
Morton SMB, Grant CC, Wall CR, Carr PEA, Bandara DK, Schmidt JM, Ivory V, Inskip HM, Camargo CA (2014) Adherence to nutritional guidelines in pregnancy: evidence from the Growing Up in New Zealand birth cohort study. Public Health Nutr 17(9):1919–1929. https://doi.org/10.1017/S1368980014000482
Malek L, Umberger W, Makrides M, Zhou SJ (2016) Adherence to the Australian dietary guidelines during pregnancy: evidence from a national study. Public Health Nutr 19(7):1155–1163. https://doi.org/10.1017/S1368980015002232
Leme ACB, Hou S, Fisberg RM, Fisberg M, Haines J (2021) Adherence to food-based dietary guidelines: a systemic review of high-income and low- and middle-income countries. Nutrients 13(3):1038
Grenier LN, Atkinson SA, Mottola MF, Wahoush O, Thabane L, Xie F, Vickers-Manzin J, Moore C, Hutton EK, Murray-Davis B (2021) Be healthy in pregnancy: exploring factors that impact pregnant women’s nutrition and exercise behaviours. Matern Child Nutr 17(1):e13068. https://doi.org/10.1111/mcn.13068
Lucas C, Charlton KE, Yeatman H (2014) Nutrition advice during pregnancy: do women receive it and can health professionals provide it? Matern Child Health J 18(10):2465–2478. https://doi.org/10.1007/s10995-014-1485-0
de Jersey SJ, Nicholson JM, Callaway LK, Daniels LA (2013) An observational study of nutrition and physical activity behaviours, knowledge, and advice in pregnancy. BMC Pregnancy Childbirth 13(1):115. https://doi.org/10.1186/1471-2393-13-115
Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, Rexrode KM, Rimm EB, Qi L, Willett WC, Manson JE, Qi Q, Hu FB (2020) Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med 180(8):1090–1100. https://doi.org/10.1001/jamainternmed.2020.2176
Yong HY, Mohd Shariff Z, Mohd Yusof B-N, Rejali Z, Appannah G, Bindels J, Tee YYS, van der Beek EM (2020) The association between dietary patterns before and in early pregnancy and the risk of gestational diabetes mellitus (GDM): data from the Malaysian SECOST cohort. PLOS ONE 15(1):e0227246. https://doi.org/10.1371/journal.pone.0227246
Kahleova H, Salas-Salvadó J, Rahelić D, Kendall CW, Rembert E, Sievenpiper JL (2019) Dietary patterns and cardiometabolic outcomes in diabetes: a summary of systematic reviews and meta-analyses. Nutrients 11(9):2209. https://doi.org/10.3390/nu11092209
Mousa A, Naqash A, Lim S (2019) Macronutrient and micronutrient intake during pregnancy: an overview of recent evidence. Nutrients 11(2):443. https://doi.org/10.3390/nu11020443
Farpour-Lambert NJ, Ells LJ, Martinez de Tejada B, Scott C (2018) Obesity and weight gain in pregnancy and postpartum: an evidence review of lifestyle interventions to inform maternal and child health policies. Front Endocrinol. https://doi.org/10.3389/fendo.2018.00546
Thorpe MG, Milte CM, Crawford D, McNaughton SA (2016) A revised Australian dietary guideline index and its association with key sociodemographic factors, health behaviors and body mass index in peri-retirement aged adults. Nutrients 8(3):160
Lioret S, McNaughton SA, Cameron AJ, Crawford D, Campbell KJ, Cleland VJ, Ball K (2014) Three-year change in diet quality and associated changes in BMI among schoolchildren living in socio-economically disadvantaged neighbourhoods. Br J Nutr 112(2):260–268. https://doi.org/10.1017/S0007114514000749
Collings PJ, Farrar D, Gibson J, West J, Barber SE, Wright J (2020) Associations of pregnancy physical activity with maternal cardiometabolic health, neonatal delivery outcomes and body composition in a biethnic cohort of 7305 mother–child pairs: the born in Bradford Study. Sports Med 50(3):615–628. https://doi.org/10.1007/s40279-019-01193-8
Acknowledgements
Sources of support (grants and fellowships/funding): This study was funded by the Deakin University Faculty of Health, Health Research Capacity Building Grant Scheme. Initial lipidomic analyses was funded by a Monash Health and Translation Precinct seed grant to Stacey Ellery and Aya Mousa. Stacey Ellery was supported by an Australian NHMRC Early Career Fellowship (1125539). Shariful Islam was funded by a Heart Foundation Postdoctoral Fellowship and NHMRC Emerging Leadership Fellowship. Kevin Huynh and Peter Meikle were supported by a NHMRC Investigator grants (1197190 and 2009965). Aya Mousa is funded by an Australian NHMRC Biomedical Research Fellowship (1161871). This work was supported by the Victorian Government’s Operational Infrastructure Support Program. The authors would like to thank the participants of the CPO study, their pregnancy care providers and their families. We also wish to thank the broader CPO research team for their efforts in sample collection and processing and Monash Health.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
Pv designed the research, analysed data, wrote the paper and had primary responsibility for final content; KK conducted the research and analysed data; SM designed the research, wrote the paper and had primary responsibility for final content; GA performed statistical analysis and wrote the paper; SI designed the research and wrote the paper; KH conducted the lipidomic analysis and generated the lipidomic dataset; PM provided essential materials and oversaw the lipidomic analysis; AM designed and oversaw the lipidomic analysis and wrote the paper and oversaw and SE designed the research, conducted research, provided essential materials and wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
Ethical approval for the original CPO study was granted in August 2015 from Monash Health (Ref 14140B) and Monash University (Ref 7785). The current study was granted ethical approval in July 2020 by the Deakin University Human Research Ethics Committee (DUHREC) (2020-236). Study procedures followed were in accordance with ethical standards of Monash Health, Monash University and Deakin University’s committees on human experimentation and conformed to the Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Pligt, P.F., Kuswara, K., McNaughton, S.A. et al. Maternal diet quality and associations with plasma lipid profiles and pregnancy-related cardiometabolic health. Eur J Nutr 62, 3369–3381 (2023). https://doi.org/10.1007/s00394-023-03244-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03244-3