Abstract
Purpose
The leaky gut barrier is an important factor leading to various inflammatory gastrointestinal disorders. The nutritional value of honey and variety of its health benefits have long been recognized. This study was undertaken to assess the role of Indian mustard honey in preventing lipopolysaccharide (LPS)-induced intestinal barrier dysfunction using a combination of in vitro and in vivo experimental model systems.
Methods
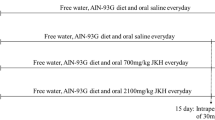
LPS was used to induce intestinal barrier damage in a trans-well model of Caco-2 cells (1 µg/ml) and in Swiss albino mice (5 mg/kg body weight). Gas chromatography–mass spectrometry (GC–MS) and liquid chromatography–mass spectrometry (LC–MS) were used to analyse sugar and phenolic components in honey samples. The Caco-2 cell monolayer integrity was evaluated by transepithelial electrical resistance (TEER) and paracellular permeability assays. The histopathology of intestinal tissue was analysed by haematoxylin and eosin dual staining. The quantitative reverse transcription-polymerase chain reaction (qRT-PCR) was used to quantify the transcription of genes. The protein expression was analysed by immunofluorescence, western blot and ELISA-based techniques.
Results
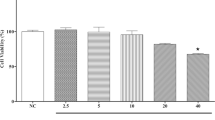
The in vitro data showed that honey prevented LPS-induced intestinal barrier dysfunction dose dependently as was measured by TEER and paracellular flux of FITC-dextran dye. Further, the in vivo data showed a prophylactic effect of orally administered honey as it prevented the loss of intestinal barrier integrity and villus structure. The cellular localization and expression of tight junction (TJ) proteins were upregulated along with downregulation of pro-inflammatory cytokines in response to the administration of honey with LPS.
Conclusions
The findings of this study suggest a propitious role of honey in the maintenance of TJ protein integrity, thereby preventing LPS-induced intestinal barrier disintegration.







Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Bai Y, Huang F, Zhang R et al (2020) Longan pulp polysaccharides relieve intestinal injury in vivo and in vitro by promoting tight junction expression. Carbohydr Polym 229:115475. https://doi.org/10.1016/j.carbpol.2019.115475
Yang Y, Li W, Sun Y et al (2015) Amino acid deprivation disrupts barrier function and induces protective autophagy in intestinal porcine epithelial cells. Amino Acids 47:2177–2184. https://doi.org/10.1007/s00726-014-1844-6
Blikslager AT, Moeser AJ, Gookin JL et al (2007) Restoration of barrier function in injured intestinal mucosa. Physiol Rev 87:545–564. https://doi.org/10.1152/PHYSREV.00012.2006/ASSET/IMAGES/LARGE/Z9J0020724330008.JPEG
Groschwitz KR, Hogan SP (2009) Intestinal barrier function: molecular regulation and disease pathogenesis. J Allergy Clin Immunol 124:3–20
Kurashima Y, Kiyono H (2017) Mucosal ecological network of epithelium and immune cells for gut homeostasis and tissue healing. Annu Rev Immunol 35:119–147
Stokes CR (1995) Handbook of mucosal immunology. Immunol Today 16:115. https://doi.org/10.1016/0167-5699(95)80113-8
Fanning AS, Jameson BJ, Jesaitis LA, Anderson JM (1998) The tight junction protein ZO-1 establishes a link between the transmembrane protein occludin and the actin cytoskeleton. J Biol Chem 273:29745–29753. https://doi.org/10.1074/jbc.273.45.29745
Furuse M, Hata M, Furuse K et al (2002) Claudin-based tight junctions are crucial for the mammalian epidermal barrier: a lesson from claudin-1-deficient mice. J Cell Biol 156:1099–1111. https://doi.org/10.1083/jcb.200110122
Clark JA, Doelle SM, Halpern MD et al (2006) Intestinal barrier failure during experimental necrotizing enterocolitis: protective effect of EGF treatment. Am J Physiol Gastrointest Liver Physiol. https://doi.org/10.1152/ajpgi.00090.2006
Camilleri M, Madsen K, Spiller R et al (2012) Intestinal barrier function in health and gastrointestinal disease. Neurogastroenterol Motil 24:503–512. https://doi.org/10.1111/J.1365-2982.2012.01921.X
Piche T, Barbara G, Aubert P et al (2009) Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut 58:196–201. https://doi.org/10.1136/gut.2007.140806
Su L, Shen L, Clayburgh DR et al (2009) Targeted epithelial tight junction dysfunction causes immune activation and contributes to development of experimental colitis. Gastroenterology 136:551–563. https://doi.org/10.1053/j.gastro.2008.10.081
Williams JM, Duckworth CA, Watson AJM et al (2013) A mouse model of pathological small intestinal epithelial cell apoptosis and shedding induced by systemic administration of lipopolysaccharide. DMM Dis Model Mech 6:1388–1399. https://doi.org/10.1242/dmm.013284
Han X, Fink MP, Yang R, Delude RL (2004) Increased iNOS activity is essential for intestinal epithelial tight junction dysfunction in endotoxemic mice. Shock 21:261–270. https://doi.org/10.1097/01.shk.0000112346.38599.10
Adib-Conquy M, Cavaillon JM (2007) Stress molecules in sepsis and systemic inflammatory response syndrome. FEBS Lett 581:3723–3733. https://doi.org/10.1016/j.febslet.2007.03.074
Turner JR (2009) Intestinal mucosal barrier function in health and disease. Nat Rev Immunol 9:799–809
Musso G, Gambino R, Cassader M (2010) Gut microbiota as a regulator of energy homeostasis and ectopic fat deposition: mechanisms and implications for metabolic disorders. Curr Opin Lipidol 21:76–83. https://doi.org/10.1097/MOL.0b013e3283347ebb
Beutler B, Du X, Poltorak A (2016) Identification of Toll-like receptor 4 (Tlr4) as the sole conduit for LPS signal transduction: genetic and evolutionary studies. J Endotoxin Res 7:277–280. https://doi.org/10.1177/09680519010070040901
Beutler B (2002) Review paper: LPS in microbial pathogenesis: promise and fulfilment. J Endotoxin Res 8:329–335. https://doi.org/10.1177/09680519020080050601
Wellington MO, Hamonic K, Krone JEC et al (2020) Effect of dietary fiber and threonine content on intestinal barrier function in pigs challenged with either systemic E. coli lipopolysaccharide or enteric Salmonella typhimurium. J Anim Sci Biotechnol 11:1–12. https://doi.org/10.1186/s40104-020-00444-3
Bhattarai Y (2018) Microbiota-gut-brain axis: Interaction of gut microbes and their metabolites with host epithelial barriers. Neurogastroenterol Motil. https://doi.org/10.1111/NMO.13366
Roehlen N, Suarez AAR, El Saghire H et al (2020) Tight junction proteins and the biology of hepatobiliary disease. Int J Mol Sci. https://doi.org/10.3390/ijms21030825
Meddings JB, Swain MG (2000) Environmental stress-induced gastrointestinal permeability is mediated by endogenous glucocorticoids in the rat. Gastroenterology 119:1019–1028. https://doi.org/10.1053/gast.2000.18152
Suzuki T, Hara H (2009) Quercetin enhances intestinal barrier function through the assembly of zonnula occludens-2, occludin, and claudin-1 and the expression of claudin-4 in caco-2 cells. J Nutr 139:965–974. https://doi.org/10.3945/jn.108.100867
Suzuki T, Tanabe S, Hara H (2011) Kaempferol enhances intestinal barrier function through the cytoskeletal association and expression of tight junction proteins in Caco-2 cells. J Nutr 141:87–94
Watson JL, Ansari S, Cameron H et al (2004) Green tea polyphenol (-)-epigallocatechin gallate blocks epithelial barrier dysfunction provoked by IFN-γ but not by IL-4. Am J Physiol Gastrointest Liver Physiol. https://doi.org/10.1152/ajpgi.00302.2003
Kim CY, Kim KH (2014) Curcumin prevents leptin-induced tight junction dysfunction in intestinal Caco-2 BBe cells. J Nutr Biochem 25:26–35. https://doi.org/10.1016/j.jnutbio.2013.08.011
Talebi M, Talebi M, Farkhondeh T, Samarghandian S (2020) Molecular mechanism-based therapeutic properties of honey. Biomed Pharmacother 130:110590
Cianciosi D, Forbes-Hernández TY, Afrin S et al (2018) Phenolic compounds in honey and their associated health benefits: a review. Molecules 23:2322
Abubakar MB, Abdullah WZ, Sulaiman SA, Suen AB (2012) A review of molecular mechanisms of the anti-leukemic effects of phenolic compounds in honey. Int J Mol Sci 13:15054–15073
Biesaga M, Pyrzynska K (2009) Liquid chromatography/tandem mass spectrometry studies of the phenolic compounds in honey. J Chromatogr A 1216:6620–6626. https://doi.org/10.1016/J.CHROMA.2009.07.066
Samarghandian S, Farkhondeh T, Samini F (2017) Honey and health: a review of recent clinical research. Pharmacognosy Res 9:121–127
Martinotti S, Ranzato E (2018) Honey, wound repair and regenerative medicine. J Funct Biomater 9:34
Hadjmohammadi MR, Nazari SSSJ (2010) Separation optimization of quercetin, hesperetin and chrysin in honey by micellar liquid chromatography and experimental design. J Sep Sci 33:3144–3151. https://doi.org/10.1002/jssc.201000326
Tarnawski A (2005) Cellular and molecular mechanisms of gastrointestinal ulcer healing. Dig Dis Sci 50:24–33. https://doi.org/10.1007/s10620-005-2803-6
Nzeako BC, Al-Namaani F (2006) The antibacterial activity of honey on Helicobacter pylori. Sultan Qaboos Univ Med J 6:71–76
Ranzato E, Martinotti S (2014) Cellular and molecular mechanisms of honey wound healing. Nova Science Publishers, Hauppauge, NY, pp 1–155
Van De Walle J, Hendrickx A, Romier B et al (2010) Inflammatory parameters in Caco-2 cells: effect of stimuli nature, concentration, combination and cell differentiation. Toxicol Vitr 24:1441–1449. https://doi.org/10.1016/j.tiv.2010.04.002
Hubatsch I, Ragnarsson EGE, Artursson P (2007) Determination of drug permeability and prediction of drug absorption in Caco-2 monolayers. Nat Protoc 2:2111–2119. https://doi.org/10.1038/nprot.2007.303
Shao Y, Wolf PG, Guo S et al (2017) Zinc enhances intestinal epithelial barrier function through the PI3K/AKT/mTOR signaling pathway in Caco-2 cells. J Nutr Biochem 43:18–26. https://doi.org/10.1016/j.jnutbio.2017.01.013
Putt KK, Pei R, White HM, Bolling BW (2017) Yogurt inhibits intestinal barrier dysfunction in Caco-2 cells by increasing tight junctions. Food Funct 8:406–414. https://doi.org/10.1039/c6fo01592a
Ling X, Linglong P, Weixia D, Hong W (2016) Protective effects of bifidobacterium on intestinal barrier function in LPS-induced enterocyte barrier injury of Caco-2 monolayers and in a rat NEC model. PLoS ONE. https://doi.org/10.1371/journal.pone.0161635
Afrin S, Giampieri F, Gasparrini M et al (2018) The inhibitory effect of Manuka honey on human colon cancer HCT-116 and LoVo cell growth. Part 1: the suppression of cell proliferation, promotion of apoptosis and arrest of the cell cycle. Food Funct 9:2145–2157. https://doi.org/10.1039/C8FO00164B
Gasparrini M, Afrin S, Forbes-Hernández TY et al (2018) Protective effects of Manuka honey on LPS-treated RAW 264.7 macrophages. Part 2: control of oxidative stress induced damage, increase of antioxidant enzyme activities and attenuation of inflammation. Food Chem Toxicol 120:578–587. https://doi.org/10.1016/J.FCT.2018.08.001
Jaganathan SK (2009) Honey constituents and their apoptotic effect in colon cancer cells. J ApiProduct ApiMedical Sci 1:29–36. https://doi.org/10.3896/ibra.4.01.2.02
Ruiz-Matute AI, Soria AC, Martínez-Castro I, Sanz ML (2007) A new methodology based on GC-MS to detect honey adulteration with commercial syrups. J Agric Food Chem 55:7264–7269. https://doi.org/10.1021/jf070559j
Ghaffarian R, Muro S (2013) Models and methods to evaluate transport of drug delivery systems across cellular barriers. J Vis Exp. https://doi.org/10.3791/50638
Ranneh Y, Akim AM, Hamid HA et al (2021) Honey and its nutritional and anti-inflammatory value. BMC Complement Med Ther 21:1–17. https://doi.org/10.1186/s12906-020-03170-5
Gencay C, Kilicoglu SS, Kismet K et al (2008) Effect of honey on bacterial translocation and intestinal morphology in obstructive jaundice. World J Gastroenterol 14:3410–3415. https://doi.org/10.3748/wjg.14.3410
Mehranfard N, Yazdi A, Rafiei A et al (2020) Honey protects against chronic unpredictable mild stress induced- intestinal barrier disintegration and hepatic inflammation. Mol Biol Rep 47:8475–8484. https://doi.org/10.1007/s11033-020-05888-4
Cai G, Wu Y, Wusiman A et al (2021) Alhagi honey polysaccharides attenuate intestinal injury and immune suppression in cyclophosphamide-induced mice. Food Funct 12:6863–6877. https://doi.org/10.1039/d1fo01008e
Almasaudi SB, Abbas AT, Al-Hindi RR et al (2017) Manuka honey exerts antioxidant and anti-inflammatory activities that promote healing of acetic acid-induced gastric ulcer in rats. Evid Based Complement Alternat Med. https://doi.org/10.1155/2017/5413917
Kassim M, Yusoff KM, Ong G et al (2012) Gelam honey inhibits lipopolysaccharide-induced endotoxemia in rats through the induction of heme oxygenase-1 and the inhibition of cytokines, nitric oxide, and high-mobility group protein B1. Fitoterapia 83:1054–1059. https://doi.org/10.1016/J.FITOTE.2012.05.008
Cani PD, Bibiloni R, Knauf C et al (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet–induced obesity and diabetes in mice. Am Diabetes Assoc 57:1470–1481. https://doi.org/10.2337/db07-1403
Woting A, Blaut M (2018) Small intestinal permeability and gut-transit time determined with low and high molecular weight fluorescein isothiocyanate-dextrans in C3H mice. Nutrients. https://doi.org/10.3390/nu10060685
Feldman AT, Wolfe D (2014) Tissue processing and hematoxylin and eosin staining. Methods Mol Biol 1180:31–43. https://doi.org/10.1007/978-1-4939-1050-2_3
Erben U, Christoph Loddenkemper KD, Spieckermann S et al (2014) A guide to histomorphological evaluation of intestinal inflammation in mouse models. Int J Clin Exp Pathol 7:4557–4576
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative CT method. Nat Protoc 3:1101–1108. https://doi.org/10.1038/nprot.2008.73
Huang L, Cui K, Mao W et al (2020) Weissella cibaria attenuated LPS-induced dysfunction of intestinal epithelial barrier in a Caco-2 cell monolayer model. Front Microbiol. https://doi.org/10.3389/fmicb.2020.02039
Pereira da Costa M, Conte-Junior CA (2015) Chromatographic methods for the determination of carbohydrates and organic acids in foods of animal origin. Compr Rev Food Sci Food Saf 14:586–600. https://doi.org/10.1111/1541-4337.12148
Puścion-Jakubik A, Borawska MH, Socha K (2020) Modern methods for assessing the quality of Bee Honey and botanical origin identification. Foods 9:1028. https://doi.org/10.3390/foods9081028
Gómez-Caravaca AM, Gómez-Romero M, Arráez-Román D et al (2006) Advances in the analysis of phenolic compounds in products derived from bees. J Pharm Biomed Anal 41:1220–1234. https://doi.org/10.1016/j.jpba.2006.03.002
Chen J, Zhang R, Wang J et al (2015) Protective effects of baicalin on LPS-induced injury in intestinal epithelial cells and intercellular tight junctions. Can J Physiol Pharmacol 93:233–237. https://doi.org/10.1139/cjpp-2014-0262
Kordulewska NK, Topa J, Tańska M et al (2021) Modulatory effects of osthole on lipopolysaccharides-induced inflammation in Caco-2 cell monolayer and co-cultures with THP-1 and THP-1-derived macrophages. Nutrients 13:1–16. https://doi.org/10.3390/nu13010123
Kim MS, Kim JY (2017) Intestinal anti-inflammatory effects of cinnamon extracts in a co-culture model of intestinal epithelial Caco-2 cells and RAW264.7 macrophages. Appl Biol Chem 60:553–561. https://doi.org/10.1007/s13765-017-0311-y
Zhao H, Zhang H, Wu H et al (2012) Protective role of 1,25(OH)2vitamin D3 in the mucosal injury and epithelial barrier disruption in DSS-induced acute colitis in mice. BMC Gastroenterol 12:1–14. https://doi.org/10.1186/1471-230X-12-57
Guo S, Al-Sadi R, Said HM, Ma TY (2013) Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am J Pathol 182:375–387. https://doi.org/10.1016/j.ajpath.2012.10.014
König J, Wells J, Cani PD et al (2016) Human intestinal barrier function in health and disease. Clin Transl Gastroenterol. https://doi.org/10.1038/ctg.2016.54
Vancamelbeke M, Vermeire S (2017) The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol 11:821–834. https://doi.org/10.1080/17474124.2017.1343143
De Santis S, Cavalcanti E, Mastronardi M et al (2015) Nutritional keys for intestinal barrier modulation. Front Immunol. https://doi.org/10.3389/fimmu.2015.00612
Ménard S, Cerf-Bensussan N, Heyman M (2010) Multiple facets of intestinal permeability and epithelial handling of dietary antigens. Mucosal Immunol 3:247–259. https://doi.org/10.1038/mi.2010.5
He S, Guo Y, Zhao J et al (2020) Ferulic acid ameliorates lipopolysaccharide-induced barrier dysfunction via MicroRNA-200c-3p-mediated activation of PI3K/AKT pathway in Caco-2 cells. Front Pharmacol 11:1–13. https://doi.org/10.3389/fphar.2020.00376
Xu J, Song J, Zhang Y et al (2020) Jinzhi protects lipopolysaccharide-treated mice against mortality by repairing intestinal mucosal barrier damage and intestinal microecology. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2019.109749
Beguin P, Errachid A, Larondelle Y, Schneider YJ (2013) Effect of polyunsaturated fatty acids on tight junctions in a model of the human intestinal epithelium under normal and inflammatory conditions. Food Funct 4:923–931. https://doi.org/10.1039/c3fo60036j
Ghosh SS, Wang J, Yannie PJ, Ghosh S (2020) Intestinal barrier dysfunction, LPS translocation, and disease development. J Endocr Soc 4:1–15. https://doi.org/10.1210/jendso/bvz039
Catalioto R-M, AMaggiGiuliani ACS (2012) Intestinal epithelial barrier dysfunction in disease and possible therapeutical interventions. Curr Med Chem 18:398–426. https://doi.org/10.2174/092986711794839179
Raynaud A, Ghezali L, Gloaguen V et al (2013) Honey-induced macrophage stimulation: AP-1 and NF-κB activation and cytokine production are unrelated to LPS content of honey. Int Immunopharmacol 17:874–879. https://doi.org/10.1016/j.intimp.2013.09.014
Wu L, Du B, Vander Heyden Y et al (2017) Recent advancements in detecting sugar-based adulterants in honey—a challenge. TrAC Trends Anal Chem 86:25–38. https://doi.org/10.1016/j.trac.2016.10.013
Erejuwa OO, Sulaiman SA, Wahab MSA (2012) molecules fructose might contribute to the hypoglycemic effect of honey. Molecules. https://doi.org/10.3390/molecules17021900
Walle T, Otake Y, Brubaker JA et al (2001) Disposition and metabolism of the flavonoid chrysin in normal volunteers. Br J Clin Pharmacol 51:143–146. https://doi.org/10.1111/j.1365-2125.2001.01317.x
Roberts AT, Martin CK, Liu Z et al (2007) The safety and efficacy of a dietary herbal supplement and gallic acid for weight loss. J Med Food 10:184–188. https://doi.org/10.1089/jmf.2006.272
Cao G, Ying P, Yan B et al (2015) Pharmacokinetics, safety, and tolerability of single and multiple-doses of pinocembrin injection administered intravenously in healthy subjects. J Ethnopharmacol 168:31–36. https://doi.org/10.1016/j.jep.2015.03.041
dos Scholz MBS, Quinhone Júnior A, Delamuta BH et al (2020) Indication of the geographical origin of honey using its physicochemical characteristics and multivariate analysis. J Food Sci Technol 57:1896. https://doi.org/10.1007/S13197-019-04225-3
El Sohaimy SA, Masry SHD, Shehata MG (2015) Physicochemical characteristics of honey from different origins. Ann Agric Sci 60:279–287. https://doi.org/10.1016/J.AOAS.2015.10.015
Wolfs TGAM, Kramer BW, Thuijls G et al (2014) Chorioamnionitis-induced fetal gut injury is mediated by direct gut exposure of inflammatory mediators or by lung inflammation. Am J Physiol Gastrointest Liver Physiol 306:382–393. https://doi.org/10.1152/ajpgi.00260.2013
Wang X, Wang S, Li Y et al (2013) Sulfated Astragalus polysaccharide can regulate the inflammatory reaction induced by LPS in Caco2 cells. Int J Biol Macromol 60:248–252. https://doi.org/10.1016/j.ijbiomac.2013.05.037
Soufli I, Toumi R, Rafa H, Touil-Boukoffa C (2016) Overview of cytokines and nitric oxide involvement in immuno-pathogenesis ofinflammatory bowel diseases. World J Gastrointest Pharmacol Ther 7:353. https://doi.org/10.4292/WJGPT.V7.I3.353
Dörfel MJ, Huber O (2012) Modulation of tight junction structure and function by kinases and phosphatases targeting occludin. J Biomed Biotechnol 2012:807356. https://doi.org/10.1155/2012/807356
Wei L, Li Y, Tang W et al (2019) Chronic unpredictable mild stress in rats induces colonic inflammation. Front Physiol. https://doi.org/10.3389/fphys.2019.01228
Moreira APB, Texeira TFS, Ferreira AB et al (2012) Influence of a high-fat diet on gut microbiota, intestinal permeability and metabolic endotoxaemia. Br J Nutr 108:801–809. https://doi.org/10.1017/S0007114512001213
Oguz S, Salt O, Ibis AC et al (2018) Combined effectiveness of honey and immunonutrition on bacterial translocation secondary to obstructive jaundice in rats: experimental study. Med Sci Monit 24:3374–3381. https://doi.org/10.12659/MSM.907977
Miguel MG, Antunes MD, Faleiro ML (2017) Honey as a complementary medicine. Integr Med Insights 12:1–15. https://doi.org/10.1177/1178633717702869
Ajibola A, Chamunorwa JP, Erlwanger KH (2012) Nutraceutical values of natural honey and its contribution to human health and wealth. Nutr Metab 9:1–12. https://doi.org/10.1186/1743-7075-9-61
Nair A, Jacob S (2016) A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm 7:27. https://doi.org/10.4103/0976-0105.177703
Gupta J, Nebreda A (2014) Analysis of intestinal permeability in mice. Bio-Protoc. https://doi.org/10.21769/bioprotoc.1289
Cho YE, Kim DK, Seo W et al (2021) Fructose promotes leaky gut, endotoxemia, and liver fibrosis through ethanol-inducible cytochrome P450–2E1–mediated oxidative and nitrative stress. Hepatology 73:2180–2195. https://doi.org/10.1002/hep.30652
Acknowledgements
This work is supported by the research grant to PR from National Bee Board, Ministry of Agriculture and Framer’s Welfare, Government of India (No. 6-44/2020-NBB dated 14.01.2021 and 6-29/2022-NBB dated 25.03.2022). SN was supported initially by funding from Department of Biotechnology, Ministry of Science and Technology (File No. BT/AGR/biofort/PHI/NIN/2011) and Ministry of Human Resources, Government of India for providing fellowship. The authors would like to thank the technical assistance of Institute Instrumentation Centre at Indian Institute of Technology Roorkee, Roorkee 247 667, Uttarakhand, India for various experiments.
Author information
Authors and Affiliations
Contributions
PR and SN designed the entire in vitro and in vivo study. SN completed the experiment process, literature search and generation of figures. ND supported in in vivo study. PK and BW provided support for carrying out experiments. SN and PR wrote the manuscript while DS supported in interpreting some data and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Ethics declarations
The entire animal handling and study were performed according to the recommendations in the Guidelines for Laboratory Animal Facility of the Committee for the Purpose of Control and Supervision on Experiments on Animals (CPCSEA), Ministry of Fisheries, Animal Husbandry and Dairying, Department of Animal Husbandry and Dairying, Government of India, with prior approval from the Institutional Animal Ethics Committee (BT/IAEC/2018/2/06 dated December 07, 2018) of the Indian Institute of Technology, Roorkee, India.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nathani, S., Das, N., Katiyar, P. et al. Consumption of honey ameliorates lipopolysaccharide-induced intestinal barrier dysfunction via upregulation of tight junction proteins. Eur J Nutr 62, 3033–3054 (2023). https://doi.org/10.1007/s00394-023-03203-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03203-y