Abstract
Purpose
Higher dairy consumption is associated with a lower risk of colorectal cancer (CRC), but no studies thus far have investigated its relation with recurrence in CRC. Few studies have investigated total dairy in relation to mortality in CRC, and yielded inconsistent results.
Methods
In this prospective cohort study, people newly diagnosed with stage I-III CRC filled out a food frequency questionnaire at diagnosis (n = 1812) and six months after diagnosis (n = 1672). We examined associations between pre- and post-diagnostic intake of total dairy, low-fat dairy, high-fat dairy, milk, yoghurt, and cheese with recurrence and all-cause mortality using multivariable Cox proportional hazard models and restricted cubic splines (RCS).
Results
A total of 176 recurrences and 301 deaths occurred during a median follow-up of 3.0 and 5.9 years, respectively. Before diagnosis, a higher low-fat dairy intake was associated with a lower risk of recurrence (HRQ4vsQ1: 0.42, 95% CI 0.26–0.67; PRCS: 0.008) and all-cause mortality (HRQ4vsQ1: 0.58, 95% CI 0.41–0.81; PRCS < 0.001), whereas a higher high-fat dairy consumption tended to be associated with an increased all-cause mortality risk (HRQ4vsQ1: 1.41, 95% CI 0.98–2.01; PRCS: 0.030). After diagnosis, only the associations between low- and high-fat dairy in relation to all-cause mortality remained.
Conclusions
This study demonstrated that higher pre- and post-diagnostic intakes of low-fat dairy were associated with a reduced all-cause mortality risk in people with stage I-III CRC, whereas higher intakes of high-fat dairy were associated with an increased all-cause mortality risk. Also, a higher pre-diagnostic low-fat dairy intake was associated with a reduced risk of recurrence.
Trial registration
Clinical Trials.gov identifier: NCT03191110.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evidence from observational studies suggests that dairy consumption decreases the risk of colorectal cancer (CRC) [1, 2]. Contrasting the large body of evidence and the proposed biological mechanisms [3, 4] available on dairy consumption and CRC risk, a scarcity of studies has been published on the role of dairy intake in CRC prognosis, such as cancer recurrence and all-cause mortality.
For total dairy, two large prospective cohort studies and one pooled analysis of prospective cohort studies observed no association between pre-diagnostic [5, 6] or post-diagnostic [6, 7] dairy intake and CRC-specific or all-cause mortality. However, when stratifying for fat content, one pooled analysis including 1753 individuals with CRC showed that a higher post-diagnostic intake of low-fat dairy products was associated with a reduced risk of all-cause mortality, whereas a higher post-diagnostic intake of high-fat dairy products was associated with an increased risk of all-cause mortality [7]. The authors speculated that potentially beneficial dairy components may be counteracted by fat or fat-related components of dairy [7], which may explain previously observed null associations for total dairy intake with all-cause mortality [5, 6]. We therefore hypothesise that low-fat dairy intake is associated with a reduced risk of all-cause mortality, and that high-fat dairy intake is associated with an increased risk of all-cause mortality.
Inherent to their unique nutritional compositions and in line with existing literature on CRC risk, different dairy products, such as milk, yoghurt, and cheese, are proposed to have a differential influence on CRC prognosis [1, 2, 8,9,10]. So far, not enough studies have been performed to draw firm conclusions on the association between specific dairy product intake and mortality in CRC. To the best of our knowledge, it is yet unknown whether dairy intake before or after diagnosis is associated with cancer recurrence in people with CRC.
Therefore, we investigated the relation between pre- and post-diagnostic intake of dairy (total, low-fat, high-fat) and specific dairy products (milk, yoghurt, cheese) with cancer recurrence and all-cause mortality in a prospective cohort of newly-diagnosed males and females with stage I-III CRC.
Materials and methods
Study cohort
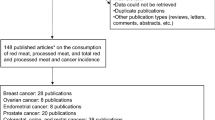
For these analyses we used data from adults with newly diagnosed CRC who participated in the ‘COlorectal cancer: Longitudinal, Observational study on Nutritional and lifestyle factors that influence colorectal tumour cancer recurrence, survival and quality of life’ (COLON) study (NCT03191110, ClinicalTrials.gov). Participants were recruited from 11 hospitals in the Netherlands between August 2010 and February 2020, and had no hereditary CRC syndrome, a history of CRC or inflammatory bowel disease [11]. Details of this study have been described previously [11]. For the current analyses, we excluded some participants (Fig. 1), among which people diagnosed with stage IV disease (n = 150), as we expect the potential role of lifestyle to be very limited in the poor prognosis of these persons. The final analytical sample sizes were as follows: 1812 (all-cause mortality) and 1341 (recurrence) for pre-diagnostic models, and 1672 (all-cause mortality) and 1236 (recurrence) for post-diagnostic models (Fig. 1). Three participants were lost to follow-up due to moving abroad. The COLON study was approved by a medical ethics committee (region Arnhem-Nijmegen, 2009–349), and all study participants provided written informed consent.
Dietary assessment
Upon diagnosis, participants filled out a semi-quantitative food frequency questionnaire (FFQ) of 204 items [12, 13], reflecting dietary intake in the month prior to diagnosis. The exact date of diagnosis was not uniformly available, but in practice participants were included in the study by the health care practitioner only a few days after the diagnosis. The median time between this date of inclusion and completion of the first FFQ was 5 days (IQR: 3–10). At six months after diagnosis participants also completed the FFQ, reflecting dietary intake in the month prior to filling out the FFQ. Dairy product intakes and energy intakes per day were calculated, based on frequency of intake and portion sizes and using the online Dutch Food Composition Table [14], and categorized into total, low-fat and high-fat dairy. Total dairy comprised of all dairy products included in low- and high-fat dairy. Low-fat dairy included low-fat or skimmed versions of milk, yoghurt, custard, and soft curd cheese, and buttermilk. High-fat dairy included whole and condensed milk, full-fat versions of yoghurt, custard and soft curd cheese, all other cheeses, ice cream, whipped cream, and butter. Total milk included all plain and sweetened milk, regardless of fat content. Ready-made breakfast drinks were not included, because not all ready-made breakfast drinks on the Dutch market contain dairy. Total yoghurt included all plain and sweetened yoghurt, yoghurt drinks and soft curd cheese, regardless of fat content. Total cheese included all hard and soft cheese, except for soft curd cheese. Intake of dairy types and products was adjusted for total energy intake using the energy residual method [15]. Further assessment of individual food items, such as skimmed milk, low-fat milk and high-fat milk, was not possible due to low median intakes and a low variation in intake. To improve interpretability, the predicted dairy intake at the median total energy intake was added to individual residuals.
Study outcomes
Recurrence was defined as a local or regional cancer recurrence or a distant metastasis diagnosed after initial tumour resection. Recurrence data were requested from the Netherlands Cancer Registry via the Netherlands Comprehensive Cancer Organisation (IKNL), most recently updated in February 2018. All-cause mortality data were obtained from the municipal registrations (BRP), most recently updated in September 2021.
For recurrence, follow-up time was calculated starting from date of surgery until date of recurrence, until date of death, until the date recurrence status was updated, or until lost to follow-up, whichever came first. Follow-up time for mortality was defined as starting from date of surgery until date of death, until the last date mortality status was updated, or until lost to follow-up, whichever came first. If date of surgery was unavailable (n = 71), date of filling out the questionnaires was used. For post-diagnostic analyses, follow-up time was calculated starting from date of filling out the post-diagnostic questionnaires.
Assessment of covariates
At diagnosis and six months after diagnosis, participants filled out a general questionnaire on demographics, anthropometrics, and lifestyle habits, including questions about age (continuous), sex (male/female), education (low, medium, high), body weight (kg), height (cm), smoking status (current, former, never), and calcium and vitamin D supplement use (including multivitamins, yes/no). Physical activity was assessed using the Short QUestionnaire to ASsess Health-enhancing physical activity (SQUASH) [16]. Moderate-to-vigorous physical activity (hours/week) included all activities with a metabolic equivalent value ≥ 3 [17]. Clinical data, such as disease stage (I-III), tumour location (proximal colon (caecum to the transverse colon), distal colon (splenic flexure to the sigmoid colon), rectum (rectosigmoid junction and rectum)), American Society of Anesthesiologists (ASA) classification (I-IV) and type of treatment (only surgery, surgery and chemotherapy, surgery and radiotherapy, surgery and chemotherapy and radiotherapy, no or unknown surgery, unknown treatment), were collected via the Dutch ColoRectal Audit [18].
To assess possible confounding by other dietary factors previously associated with CRC risk [2], we also calculated total dietary intake of wholegrains, red meat, processed meat, dietary fiber, and alcohol, as defined in [2].
Statistical analysis
Population characteristics are presented as medians [interquartile range (IQR)] or numbers (percentage). Sex-specific quartiles of pre- and post-diagnostic dairy intake were calculated.
Cox proportional hazards regression analyses were used to calculate Hazard Ratios (HR) and 95% Confidence Intervals (95%CI) for the associations between pre- and post-diagnostic dairy intake, and recurrence and all-cause mortality. No violation of the proportionality assumption for the Cox models was observed when visually inspecting log–log curves. For categorical analyses, the lowest quartile was used as the reference category. Ptrend values were computed over quartiles of dairy intake using the medians of the corresponding quartiles. For continuous analyses increments were 100 g/day for total dairy, low-fat dairy, high-fat dairy, milk, and yoghurt, and 30 g/day for cheese. We first created a crude model with the exposure and outcome variables, that was adjusted for age and sex. Then, potential confounders were added to the model one by one, and were included when they changed the HR with > 10%. Based on literature, the following covariates were evaluated: disease stage, primary tumour location, BMI, education level, smoking status, moderate-to-vigorous physical activity, use of calcium supplements, use of vitamin D supplements, and total dietary intake of wholegrains, dietary fiber, red meat, processed meat and alcohol. Additionally, for the post-diagnostic dairy intake analyses, having a stoma, type of treatment, and BMI, smoking status, supplement use and dietary intake at 6 months post-diagnosis were evaluated for confounding. Finally, the adjusted model included age, sex, stage of disease and total energy intake (as part of the energy adjustment method [15]).
We also evaluated restricted cubic splines (RCS) to study linearity of the associations between dairy exposures and CRC prognosis, using the adjusted model. Knots were placed at the 5th, 50th, and 95th percentiles, and the graphs were truncated at the 1st and 99th percentile. The median intake of the first quartile of each exposure was used as the reference.
For linear associations, HRs are displayed continuously as well as in quartiles with p for trend, while for non-linear associations, only quartiles of dairy intake are displayed. All associations are visualized in plots.
Statistical analyses were performed using R Statistical Software (version 4.0.5). P-values below 0.05 and 95% confidence intervals not containing 1 were considered statistically significant.
Results
Population characteristics
Participants were on average 66 years (IQR: 61–72) at CRC diagnosis, and 37% was female (Table 1). Median BMI was 26.2 kg/m2 (IQR: 24.0–28.7) and 10% of participants were current smokers. Furthermore, 66% had a tumour located in the colon, and stage III (43%) was more common than stage I (26%) or stage II (27%) (Table 1).
Participants in the highest quartile of total pre-diagnostic dairy intake were older, less often current smokers, and more often had a lower level of education, compared to participants in the lowest quartile of total dairy products. Also, they consumed less processed meat and alcohol, consumed more dietary calcium, and less often used calcium supplements. Participants in the highest quartile of low-fat dairy intake were less often current smokers, consumed more dietary calcium and less alcohol, more often used vitamin D supplements, and less often had an ASA score of I, compared to participants in the lowest quartile. Participants in the highest quartile of high-fat dairy products were older and more often had a lower level of education, consumed more dietary calcium, and less processed meat and alcohol and had a lower total energy intake than participants in the lowest quartile (Table 1). Median pre-diagnostic energy-adjusted intakes of total, low-fat and high-fat dairy were 270 (IQR: 177–383), 165 (IQR: 70–281), and 77 (IQR: 46–126) g/day, respectively (Table 1). Median post-diagnostic energy-adjusted intakes of total, low-fat and high-fat dairy were 282 (IQR: 184–392), 161 (IQR: 70–286), and 81 (IQR: 48–136) g/day, respectively (data not shown). Pearson correlation coefficients between pre- and post-diagnostic intakes ranged between 0.41 and 0.61 (data not shown).
For pre-diagnostic analyses, we observed 176 recurrences during a median follow-up time of 3.0 years (IQR: 2.0–4.2), and 301 participants died during a median follow-up of 5.9 years (IQR: 3.9–7.2). For post-diagnostic analyses, we observed 153 recurrences that occurred during a median follow-up time of 2.6 years (IQR: 1.7–3.8), and 245 participants died during a median follow-up of 5.5 years (IQR: 3.8–6.8).
Pre-diagnostic dairy intake in relation to recurrence and all-cause mortality
As shown in Table 2 and Supplementary Fig. 1, when comparing the highest to the lowest quartile, a higher pre-diagnostic intake of total dairy was associated with a lower risk of recurrence (HR: 0.51, 95% CI 0.33–0.80; PRCS: 0.06), and tended to be associated with all-cause mortality (HRQ4 vs Q1: 0.72, 95% CI 0.52–1.01; PRCS: 0.18). A higher intake of low-fat dairy before diagnosis was associated with a lower risk of recurrence (HR: 0.42, 95%CI 0.26–0.67, PRCS: 0.008; Table 2 and Fig. 2A) and all-cause mortality (HRQ4 vs Q1: 0.58, 95% CI 0.41–0.81; PRCS < 0.001). RCS revealed a significant non-linear association between pre-diagnostic low-fat dairy intake and all-cause mortality, with intakes higher than the median of the first quartile (i.e. 21 g/day) associated with a reduced risk of mortality (Fig. 2A). Contrastingly, a higher intake of high-fat dairy before diagnosis tended to be associated with an increased risk of all-cause mortality (HRQ4 vs Q1: 1.41, 95% CI 0.98–2.01; PRCS: 0.030). Pre-diagnostic high-fat dairy intake was not associated with recurrence. A higher yoghurt intake before diagnosis seemed associated with a lower risk of all-cause mortality (HRQ4 vs Q1: 0.70, 95% CI 0.50–0.99; PRCS: 0.09), but not with recurrence. No associations were observed between total milk or cheese intake before diagnosis and recurrence or all-cause mortality.
Associations between pre-diagnostic (A) and post-diagnostic (B) intake of low- and high-fat dairy and colorectal cancer prognosis. Solid lines are restricted cubic splines, and dashed lines are 95% confidence intervals. The reference values were set at the median of the first quartile of dairy intake. Knots were located at the 5th, 50th and 95th percentile, and the graphs were truncated at the 1st and 99th percentile. Analyses are adjusted for age, sex, disease stage and energy intake
Post-diagnostic dairy intake in relation to recurrence and all-cause mortality
As shown in Table 3 and Supplementary Fig. 1, post-diagnostic total dairy intake was not associated with recurrence or all-cause mortality. A higher intake of low-fat dairy after diagnosis tended to be associated with a lower risk of all-cause mortality (HRQ4 vs Q1: 0.76, 95% CI 0.53–1.08; PRCS: 0.011; Table 3 and Fig. 2B). RCS revealed a significant non-linear association between post-diagnostic low-fat dairy intake and all-cause mortality, with intakes higher than the median of the first quartile (i.e. 20 g/day) associated with a reduced risk of mortality (Fig. 2B). Post-diagnostic low- and high-fat dairy intakes were not associated with recurrence. A higher intake of high-fat dairy after diagnosis was associated with an increased risk of all-cause mortality (HRQ4 vs Q1: 1.60, 95% CI 1.10–2.33; PRCS: 0.006). Post-diagnostic milk, yoghurt, and cheese intake were not associated with recurrence or all-cause mortality.
Except for pre- and post-diagnostic low-fat dairy in relation to all-cause mortality, we observed no evidence of non-linearity in our RCS analyses, and findings of these analyses were in line with the Cox proportional hazard regression analyses (Fig. 2 and Supplementary Figure 1).
Discussion
This study demonstrated that a higher low-fat dairy intake was associated with a reduced risk of all-cause mortality in people with stage I-III CRC, whereas a higher intake of high-fat dairy was associated with an increased risk of all-cause mortality, both before and after diagnosis. Furthermore, a higher pre-diagnostic intake of yoghurt was associated with a reduced risk of all-cause mortality. Also, to our knowledge, this is the first study to demonstrate that higher pre-diagnostic intakes of total and low-fat dairy were associated with a reduced risk of recurrence.
Our findings on post-diagnostic low- and high-fat dairy intake in relation to all-cause mortality are in line with the results of a recent pooled analysis of the Nurses’ Health Study and Health Professionals Follow-up Study in people with stage I-IV CRC, that also demonstrated a reduced risk of all-cause mortality with higher post-diagnostic low-fat dairy intakes, and an increased risk with higher post-diagnostic high-fat dairy intakes [7]. Previous large cohort studies observed no statistically significant associations between pre- [5, 6] or post-diagnostic [6, 7] total dairy intake and all-cause mortality. Therefore, we stress the importance of considering low- and high-fat dairy separately when studying health effects of dairy.
The mechanisms linking dairy consumption to prognostic outcomes in CRC are not clear and current hypotheses are largely derived from research focussing on CRC aetiology [3, 4]. Calcium has been suggested to reduce CRC risk via binding secondary bile acids and free fatty acids in the colonic lumen, thereby reducing oxidative stress and reactive proliferation of the epithelium [19, 20]. Also, clinical trials have demonstrated that calcium can alter molecular pathways that lead to direct inhibition of cell proliferation, promotion of cell differentiation, and induction of apoptosis in tumour cells [20,21,22,23,24,25]. Other dairy components, such as conjugated linoleic acid, lactic acid-producing bacteria in fermented dairy, lactoferrin, and vitamin D in fortified dairy foods, may also reduce CRC risk [2, 3, 21, 26, 27]. Previous work from our group showed that, although no clear associations were observed, the HRs for recurrence and all-cause mortality tended to be lower for those with a higher dietary calcium intake [28]. The present study includes a larger study population and more events for recurrence and all-cause mortality. To provide insight into whether observed associations in the current study are independent of dietary calcium intake, we carried out additional exploratory analyses where we adjusted our models for dietary calcium intake (data not shown). Except for the association between cheese intake and risk of recurrence, which changed to a more positive, but still non-significant association, the observed associations did not substantially change. Furthermore, considering the current uncertainty about the biological mechanism linking dairy to CRC outcomes, this study focuses on food groups rather than micronutrients, which is closer to people’s perception of the diet and easier to translate into dietary guidelines.
Our study suggests that pre-diagnostic, but not post-diagnostic, intake of low-fat dairy is associated with a reduced risk of recurrence. A potential explanation for this time-dependent finding could be that pre-diagnostic consumption may well reflect habitual dietary consumption in the decades before cancer diagnosis, implying low-fat dairy may directly or indirectly influence carcinogenesis early in the CRC continuum [9]. Also, methodological issues, such as differences in number of events and duration of follow-up time, or differences in dairy intake could explain this time-dependent finding. For post-diagnostic intake, our study showed only associations with all-cause mortality, not with recurrence, which may suggest that post-diagnostic dairy consumption influences CRC prognosis via other ways than recurrence, such as risk of cardiovascular disease [29].
In our study, a higher pre-diagnostic intake of yoghurt intake was associated with a reduced risk of all-cause mortality. Previous large prospective cohort studies showed no statistically significant association between pre-diagnostic yoghurt consumption and CRC-specific mortality [5, 9]. Possibly, yoghurt consumption influences cardiovascular risk factors rather than CRC [30], explaining why yoghurt may be associated with all-cause mortality in the current study, but not with CRC-specific mortality in other studies. Therefore, future studies should include cause-specific death information when studying associations between yoghurt consumption and CRC prognosis.
We observed no associations between pre- or post-diagnostic total milk or cheese intake and CRC prognosis. Previous studies on milk intake demonstrated a marginal positive [5] or no association [6, 7] between pre-diagnostic total milk intake and mortality. For post-diagnostic intake, the two US cohorts observed a reduced risk of all-cause mortality with higher intakes of low-fat milk [7] and total milk [6]. In contrast to the milk studied in the US cohorts [6, 7], Dutch milk is not fortified with vitamin D. As higher concentrations of 25-hydroxyvitamin D in the blood have previously been associated with improved survival in CRC [31], this might explain the discrepancy between findings. Also, compared to an estimated median milk intake of ~ 100–150 g/day in previous studies, our study population had a relatively low milk intake with a median intake of around 50 g/day. However, our study population contained many non-consumers of milk, and mean intakes were in line with the most recent national food consumption survey [32]. Only two previous cohorts studied cheese separately, and also demonstrated no association between pre- [5] or post-diagnostic [7] cheese intake and mortality in CRC. Future studies should investigate unfortified low-fat milk intake in relation to mortality in CRC.
This study has several strengths, including the prospective study design and the availability of detailed information on cancer treatment, recurrence and both pre- and post-diagnostic dietary intake and supplement use data. Furthermore, considering the current global transition towards more plant-based diets [33,34,35], it is highly relevant to study potential health effects of dairy in cancer survivorship. A limitation of the current study is the lack of information on the specific causes of death. However, we believe all-cause mortality is a highly relevant study outcome with strong clinical relevance besides the risk of recurrence, as people with CRC are also more prone to develop other chronic diseases compared to the general population [29]. A second potential limitation is the possibility of underestimation of self-reported dietary intake data inherent to the chosen dietary assessment method. However, FFQs are commonly used in cohort studies for feasibility reasons, and literature has previously shown to capture intake of dairy reasonably well by FFQs in general [36,37,38]. Also, even though we tested for confounding of many different lifestyle factors, we cannot exclude the possibility of residual confounding. Lastly, our participants were primarily Caucasian, limiting the generalizability of our study. Future studies should make an effort to recruit a diverse range of ethnicities.
Conclusion
This study found that higher pre- and post-diagnostic intakes of low-fat dairy were associated with a reduced risk of all-cause mortality in people with stage I-III CRC, whereas higher intakes of high-fat dairy were associated with an increased risk of all-cause mortality. We also demonstrated that a higher pre-diagnostic intake of low-fat dairy was associated with a reduced risk of recurrence in persons diagnosed with stage I-III CRC. Future research should differentiate between low-and high-fat dairy when investigating associations with recurrence and mortality. When replicated in other large prospective cohorts and ultimately intervention studies, our results can contribute to specific dietary guidelines for CRC survivors who aim to improve their prognosis via lifestyle change.
Availability of data and materials
Because the data consist of identifying cohort information, some access restrictions apply, and therefore they cannot be made publicly available. Data will be shared with permission from the acting committee of the COLON study. Requests for data can be sent to dr. Fränzel van Duijnhoven, Division of Human Nutrition and Health, Wageningen University & Research, Netherlands (e-mail: franzel.vanduijnhoven@wur.nl).
Change history
12 August 2023
Spacing in table 1 has been corrected
References
Jin S, Kim Y, Je Y (2020) Dairy consumption and risks of colorectal cancer incidence and mortality: a meta-analysis of prospective cohort studies. Cancer Epidemiol Biomarkers Prev 29(11):2309–2322. https://doi.org/10.1158/1055-9965.Epi-20-0127
World Cancer Research Fund/American Institute for Cancer Research (2018) Diet, nutrition, physical activity and colorectal cancer
Norat T, Riboli E (2003) Dairy products and colorectal cancer. A review of possible mechanisms and epidemiological evidence. Eur J Clin Nutr 57(1):1–17. https://doi.org/10.1038/sj.ejcn.1601522
World Cancer Research Fund/American Institute for Cancer Research (2018) Diet, nutrition, physical activity and cancer: a global perspective
Dik VK, Murphy N, Siersema PD, Fedirko V, Jenab M, Kong SY, Hansen CP, Overvad K, Tjønneland A, Olsen A, Dossus L, Racine A, Bastide N, Li K, Kühn T, Boeing H, Aleksandrova K, Trichopoulou A, Trichopoulos D, Barbitsioti A, Palli D, Contiero P, Vineis P, Tumino R, Panico S, Peeters PH, Weiderpass E, Skeie G, Hjartåker A, Amiano P, Sánchez MJ, Fonseca-Nunes A, Barricarte A, Chirlaque MD, Redondo ML, Jirström K, Manjer J, Nilsson LM, Wennberg M, Bradbury KE, Khaw KT, Wareham N, Cross AJ, Riboli E, Bueno-de-Mesquita HB (2014) Prediagnostic intake of dairy products and dietary calcium and colorectal cancer survival–results from the EPIC cohort study. Cancer Epidemiol Biomarkers Prev 23(9):1813–1823. https://doi.org/10.1158/1055-9965.Epi-14-0172
Yang B, McCullough ML, Gapstur SM, Jacobs EJ, Bostick RM, Fedirko V, Flanders WD, Campbell PT (2014) Calcium, vitamin D, dairy products, and mortality among colorectal cancer survivors: the cancer prevention study-II nutrition cohort. J Clin Oncol 32(22):2335–2343. https://doi.org/10.1200/jco.2014.55.3024
Liu X, Yang W, Wu K, Ogino S, Wang W, He N, Chan AT, Zhang Z-F, Meyerhardt JA, Giovannucci E, Zhang X (2021) Postdiagnostic dairy products intake and colorectal cancer survival in US males and females. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab059
Barrubés L, Babio N, Becerra-Tomás N, Rosique-Esteban N, Salas-Salvadó J (2019) Association between dairy product consumption and colorectal cancer risk in adults: A systematic review and meta-analysis of epidemiologic studies. Adv Nutr 10(suppl 2):S190-s211. https://doi.org/10.1093/advances/nmy114
Michels KB, Willett WC, Vaidya R, Zhang X, Giovannucci E (2020) Yogurt consumption and colorectal cancer incidence and mortality in the Nurses’ Health Study and the health professionals follow-up study. Am J Clin Nutr 112(6):1566–1575. https://doi.org/10.1093/ajcn/nqaa244
Cho E, Smith-Warner SA, Spiegelman D, Beeson WL, van den Brandt PA, Colditz GA, Folsom AR, Fraser GE, Freudenheim JL, Giovannucci E, Goldbohm RA, Graham S, Miller AB, Pietinen P, Potter JD, Rohan TE, Terry P, Toniolo P, Virtanen MJ, Willett WC, Wolk A, Wu K, Yaun SS, Zeleniuch-Jacquotte A, Hunter DJ (2004) Dairy foods, calcium, and colorectal cancer: a pooled analysis of 10 cohort studies. J Natl Cancer Inst 96(13):1015–1022. https://doi.org/10.1093/jnci/djh185
Winkels RM, Heine-Bröring RC, van Zutphen M, van Harten-Gerritsen S, Kok DE, van Duijnhoven FJ, Kampman E (2014) The COLON study: colorectal cancer: longitudinal, observational study on nutritional and lifestyle factors that may influence colorectal tumour recurrence, survival and quality of life. BMC Cancer 14:374. https://doi.org/10.1186/1471-2407-14-374
Verkleij-Hagoort AC, de Vries JH, Stegers MP, Lindemans J, Ursem NT, Steegers-Theunissen RP (2007) Validation of the assessment of folate and vitamin B12 intake in women of reproductive age: the method of triads. Eur J Clin Nutr 61(5):610–615. https://doi.org/10.1038/sj.ejcn.1602581
Feunekes IJ, Van Staveren WA, Graveland F, De Vos J, Burema J (1995) Reproducibility of a semiquantitative food frequency questionnaire to assess the intake of fats and cholesterol in The Netherlands. Int J Food Sci Nutr 46(2):117–123. https://doi.org/10.3109/09637489509012539
National Institute for Public Health and the Environment (2019) NEVO online version 2011/3.0
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65(4 suppl):1220–1228. https://doi.org/10.1093/ajcn/65.4.1220S
Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D (2003) Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol 56(12):1163–1169. https://doi.org/10.1016/s0895-4356(03)00220-8
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS (2011) 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43(8):1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
Van Leersum NJ, Snijders HS, Henneman D, Kolfschoten NE, Gooiker GA, ten Berge MG, Eddes EH, Wouters MW, Tollenaar RA, Bemelman WA, van Dam RM, Elferink MA, Karsten TM, van Krieken JH, Lemmens VE, Rutten HJ, Manusama ER, van de Velde CJ, Meijerink WJ, Wiggers T, van der Harst E, Dekker JW, Boerma D (2013) The Dutch surgical colorectal audit. Eur J Surg Oncol 39(10):1063–1070. https://doi.org/10.1016/j.ejso.2013.05.008
Newmark HL, Wargovich MJ, Bruce WR (1984) Colon cancer and dietary fat, phosphate, and calcium: a hypothesis. J Natl Cancer Inst 72(6):1323–1325
Lamprecht SA, Lipkin M (2003) Chemoprevention of colon cancer by calcium, vitamin D and folate: molecular mechanisms. Nat Rev Cancer 3(8):601–614. https://doi.org/10.1038/nrc1144
Holt PR, Atillasoy EO, Gilman J, Guss J, Moss SF, Newmark H, Fan K, Yang K, Lipkin M (1998) Modulation of abnormal colonic epithelial cell proliferation and differentiation by low-fat dairy foods: a randomized controlled trial. JAMA 280(12):1074–1079. https://doi.org/10.1001/jama.280.12.1074
Fedirko V, Bostick RM, Flanders WD, Long Q, Sidelnikov E, Shaukat A, Daniel CR, Rutherford RE, Woodard JJ (2009) Effects of vitamin D and calcium on proliferation and differentiation in normal colon mucosa: a randomized clinical trial. Cancer Epidemiol Biomark Prev 18(11):2933–2941. https://doi.org/10.1158/1055-9965.Epi-09-0239
Holt PR, Wolper C, Moss SF, Yang K, Lipkin M (2001) Comparison of calcium supplementation or low-fat dairy foods on epithelial cell proliferation and differentiation. Nutr Cancer 41(1–2):150–155. https://doi.org/10.1080/01635581.2001.9680626
Ahearn TU, Shaukat A, Flanders WD, Rutherford RE, Bostick RM (2012) A randomized clinical trial of the effects of supplemental calcium and vitamin D3 on the APC/β-catenin pathway in the normal mucosa of colorectal adenoma patients. Cancer Prev Res (Phila) 5(10):1247–1256. https://doi.org/10.1158/1940-6207.Capr-12-0292
Rozen P, Lubin F, Papo N, Knaani J, Farbstein H, Farbstein M, Zajicek G (2001) Calcium supplements interact significantly with long-term diet while suppressing rectal epithelial proliferation of adenoma patients. Cancer 91(4):833–840. https://doi.org/10.1002/1097-0142(20010215)91:4%3c833::AID-CNCR1071%3e3.0.CO;2-9
Pufulete M (2008) Intake of dairy products and risk of colorectal neoplasia. Nutr Res Rev 21(1):56–67. https://doi.org/10.1017/s0954422408035920
Castro-Gómez P, Rodríguez-Alcalá LM, Monteiro KM, Ruiz AL, Carvalho JE, Fontecha J (2016) Antiproliferative activity of buttermilk lipid fractions isolated using food grade and non-food grade solvents on human cancer cell lines. Food Chem 212:695–702. https://doi.org/10.1016/j.foodchem.2016.06.030
Wesselink E, Kok DE, Bours MJL, de Wilt JHW, van Baar H, van Zutphen M, Geijsen A, Keulen ETP, Hansson BME, van den Ouweland J, Witkamp RF, Weijenberg MP, Kampman E, van Duijnhoven FJB (2020) Vitamin D, magnesium, calcium, and their interaction in relation to colorectal cancer recurrence and all-cause mortality. Am J Clin Nutr 111(5):1007–1017. https://doi.org/10.1093/ajcn/nqaa049
Baraghoshi D, Hawkins ML, Abdelaziz S, Park J, Wan Y, Fraser AM, Smith KR, Deshmukh V, Newman M, Rowe KG, Snyder J, Lloyd S, Samadder NJ, Hashibe M (2018) Long-term risk of cardiovascular disease among colorectal cancer survivors in a population-based cohort study. J Clin Oncol 36(7):113–113. https://doi.org/10.1200/JCO.2018.36.7_suppl.113
Cruijsen E, Jacobo Cejudo MG, Küpers LK, Busstra MC, Geleijnse JM (2021) Dairy consumption and mortality after myocardial infarction: a prospective analysis in the Alpha Omega Cohort. Am J Clin Nutr 114(1):59–69. https://doi.org/10.1093/ajcn/nqab026
Wu G, Xue M, Zhao Y, Han Y, Zhang S, Zhang J, Li C, Xu J (2020) Low circulating 25-hydroxyvitamin D level is associated with increased colorectal cancer mortality: a systematic review and dose-response meta-analysis. Biosci Rep. https://doi.org/10.1042/bsr20201008
National Institute for Public Health and the Environment (2020) The diet of the Dutch: results of the Dutch National Food Consumption Survey 2012–2016
Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood A, Jonell M, Clark M, Gordon LJ, Fanzo J, Hawkes C, Zurayk R, Rivera JA, De Vries W, Majele Sibanda L, Afshin A, Chaudhary A, Herrero M, Agustina R, Branca F, Lartey A, Fan S, Crona B, Fox E, Bignet V, Troell M, Lindahl T, Singh S, Cornell SE, Srinath Reddy K, Narain S, Nishtar S, Murray CJL (2019) Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. The Lancet 393(10170):447–492. https://doi.org/10.1016/S0140-6736(18)31788-4
Schmidt P (2018) Promoting healthy and sustainable diets in the EU. European Economic and Social Committee: Section for Agriculture, Rural Development and the Environment
Health Council of the Netherlands (2011) Guidelines for a healthy diet: the ecological perspective
Shu XO, Yang G, Jin F, Liu D, Kushi L, Wen W, Gao YT, Zheng W (2004) Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women’s Health Study. Eur J Clin Nutr 58(1):17–23. https://doi.org/10.1038/sj.ejcn.1601738
Steinemann N, Grize L, Ziesemer K, Kauf P, Probst-Hensch N, Brombach C (2017) Relative validation of a food frequency questionnaire to estimate food intake in an adult population. Food Nutr Res 61(1):1305193–1305193. https://doi.org/10.1080/16546628.2017.1305193
Haftenberger M, Heuer T, Heidemann C, Kube F, Krems C, Mensink GBM (2010) Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr J 9(1):36. https://doi.org/10.1186/1475-2891-9-36
Acknowledgements
The authors would like to thank all participants, the involved co-workers in the participating hospitals, and the COLON investigators at Wageningen University & Research. Also, the authors would like to thank the registration team of the Netherlands Comprehensive Cancer Organisation (IKNL) for the collection of data for the Netherlands Cancer Registry.
Funding
This work was supported by Wereld Kanker Onderzoek Fonds (WKOF) & World Cancer Research Fund International (WCRF International) as well as by funding (2014/1179, IIG_FULL_2021_022 and IIG_FULL_2021_023) obtained from the Wereld Kanker Onderzoek Fonds (WKOF) as part of the World Cancer Research Fund International grant programme; Alpe d’Huzes/Dutch Cancer Society (UM 2012–5653, UW 2013–5927, UW 2015–7946); and ERA-NET on Translational Cancer Research (TRANSCAN: Dutch Cancer Society (UW2013-6397, UW2014-6877) and the Netherlands Organization for Health Research and Development (ZonMw), the Netherlands) and the Regio Deal Foodvalley (162135). The funders had no role in the design of the study; the collection, analysis and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: ASL, DEK, EK, FJBD. Formal analysis: ASL. Funding acquisition: DEK, RMW, EK, FJBD. Investigation: ASL, DEK, RMW, EW, FJBD. Methodology: ASL, DEK, EK, FJBD. Project administration: ASL, DEK, EK, FJBD. Resources: HKH, JHWW. Supervision: DEK, EK, FJBD. Visualization: ASL. Writing—original draft: ASL. Writing: reviewing and editing: all co-authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Lanen, AS., Kok, D.E., Wesselink, E. et al. Pre- and post-diagnostic dairy intake in relation to recurrence and all-cause mortality in people with stage I-III colorectal cancer. Eur J Nutr 62, 2891–2904 (2023). https://doi.org/10.1007/s00394-023-03201-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03201-0