Abstract
Purpose
Dietary patterns (DPs) during pregnancy have been well researched. However, little is known about maternal diet after pregnancy. The aim of the study was to explore maternal DPs longitudinally, examine trajectories over 12 years after pregnancy and identify associated factors.
Methods
Of 14,541 pregnant women enrolled in the Avon Longitudinal Study of Parents and Children (ALSPAC) complete dietary information was available for 5336 women. Principal components analysis (PCA) was used to derive DPs. DP scores at each time point were used to create DP trajectories using group-based trajectory modelling (GBTM). Multinomial logistic regression assessed the association with maternal factors.
Results
A total of six distinct DPs were identified over time with different numbers of DPs at each time point. The “healthy” and “processed” DPs persisted over the 12-year post-pregnancy. Three trajectories of “healthy” and “processed” DPs were identified from GBTM. Half the women were on the moderately healthy DP trajectory with 37% on the lower trajectory and 9% on the higher healthy DP trajectory. 59% of women were on the lower processed DP trajectory with 38% on the moderate trajectory and 3.3% on the higher processed DP trajectory. Low educational attainment, low social class and smoking in pregnancy were independently associated with being on a less favourable DP trajectory over the 12 years.
Conclusion
Health professionals should provide support on smoking cessation along with healthy eating advice during ante-natal counselling. Continued support on eating healthily after pregnancy would be beneficial for mothers and families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Diet is an important modifiable risk behaviour that has significant links with a range of non-communicable diseases (NCDs) and related health conditions, including obesity [1]; type 2 diabetes [2]; metabolic syndrome [3]; atherosclerosis [4]; carotid artery stenosis [5]; and cancer [6]. Dietary choices that include whole grains, plenty of fruits and vegetables, unsaturated fats and low-fat dairy products and which limit sugar and salt, reduce the risk of all types of NCDs throughout the life-course [7]. The intake of a healthy, energy-balanced diet during pregnancy is crucial to achieving recommended gestational weight gain and reducing adverse pregnancy outcomes [8]. Additionally, the risk of developing long-term, adverse health outcomes such as obesity, high cholesterol levels and high blood sugar levels may increase in women after pregnancy [9]. It is therefore very important for women to eat a healthy diet during pregnancy and continue with this after delivery.
Much research has focussed on diet during pregnancy and its effects on offspring’s health [10,11,12,13], however, effect of maternal post-pregnancy diet has received less attention. Maternal healthy dietary intake after pregnancy is critical for breastfeeding newborn babies for the first 4–6 months of life and suppling key nutrients to the newborn through breastmilk [14]. Eating healthy following pregnancy and long-term health benefit in breastfed infants and future wellbeing of women including their reproductive health has been reported, but research on nutrition of women after delivery and metabolic programming outcome of their infants in later life is scarce [14,15,16]. Despite a few studies on maternal dietary intake after pregnancy, longitudinal studies on post-pregnancy dietary changes and stability have received very little attention [17, 18], highlighting a significant research gaps regarding the topic.
Changes in dietary habits among women from before to during pregnancy have been systematically examined [19]. Suggesting short-term changes in a few food items may occur, including an increased intake of fruits and vegetables, a decrease in fried and fast-foods, egg, tea and coffee consumption without any intervention [19]. A systematic review by Lee et al. evaluating changes and stability in maternal diet during and immediately after pregnancy reported mixed findings for changes in energy and micronutrient intakes [20]. Findings from these 17 studies suggested significant decreases in fruit and vegetable consumption, diet quality and healthy dietary patterns during the transition from pregnancy to early post-pregnancy, alongside increases in processed foods and fat intakes [20]. However, most of the studies included in the review had short follow-up durations from pregnancy to 6 months post-pregnancy, thus more longitudinal research on tracking of dietary patterns from pregnancy to post-pregnancy was recommended.
In the review of Lee et al., there were two studies that had analysed DPs longitudinally from pregnancy to 5 years post-pregnancy [17, 21] and three studies had tracked dietary patterns from pregnancy to post-pregnancy [17, 22, 23]. Out of two longitudinal studies, one study reported changes in energy and micronutrient intakes [21] and other study reported both stability for four DPs (“health conscious,” “processed,” “confectionery,” and “vegetarian”) and changes in DPs (“traditional”) that did not observed at 4 years post-pregnancy [17]. Overall, the review finding for the tracking of DPs suggested that maternal dietary patterns were stable and did not change significantly from pregnancy to post-pregnancy [17, 22, 23]. In addition, a recent study by Dalrymple et al. examined dietary trajectories longitudinally using diet quality index (DQI) from preconception to mid-childhood among mothers and children and reported stable diet quality trajectories across the early life of the child [24]. The study also reported that poorer dietary trajectory was associated with lower maternal age, education, higher maternal pre-pregnancy BMI, multiparity and smoking [24].
In the general population, some studies have investigated DPs longitudinally examining their stability over time [25, 26], and their impact on health-related risk factors and chronic diseases [27,28,29,30]. For example one study reported a sharp increase in a fast food based “modern” DP over two decades and its positive associations with cardio-metabolic risks in an adult population in China [30]. Group-based trajectory modelling (GBTM) has been undertaken to explore long-term changes and stability in DPs among different populations and to identify trajectories of DPs over time [27, 29, 31,32,33]. However, this method has not been used widely to track maternal dietary trajectories from pregnancy into later life [24]. There is a clear research gap in assessing maternal DPs longitudinally and following trajectories of diet into later life. Therefore, the aim of this study was to (1) extend the duration of follow up of maternal DPs to 12 years post-pregnancy, (2) identify trajectories of dietary patterns over time and (3) examine the maternal factors associated with dietary trajectories using data from the Avon Longitudinal Study of Parents and Children (ALSPAC).
Methods
Study design and participants
Avon Longitudinal Study of Parents and Children (ALSPAC) is a population-based, prospective, longitudinal British cohort of pregnant women, their partners and offspring established in the 1990s to investigate the development of health and potential diseases from the time of pregnancy in the women to the adulthood of offspring [34]. Pregnant women residing in three health districts of the county of Avon, around Bristol, in southwest England with an estimated date of delivery between April 1, 1991 and December 31, 1992, were eligible and invited to join the study [34]. A cohort of 14,541 pregnancies was established and 13,988 infants survived to 1 year of age [35, 36]. Full details of the study have been described elsewhere [37, 38]. The study had the approval of the ALSPAC Law and Ethics Committee and Local Research Ethics Committees.
Dietary assessment
Food frequency questionnaires (FFQ) were used to collect dietary data from the women at 32 weeks of pregnancy and then at 4, 8 and 12 years post-pregnancy [39]. Full details of the dietary data assessment and analysis have been reported elsewhere [17, 40]. Briefly, each questionnaire was posted to the women for self-completion at home [41]. At each time point, they were asked to report their current consumption of a wide variety of food and drink types listed in the FFQ using categorical frequencies to indicate how often ‘nowadays’ they consumed each food: (i) never or rarely; (ii) once in 2 weeks; (iii) 1–3 times a week; (iv) 4–7 times a week; (v) more than once a day. More detailed questions were asked about daily intakes of basic foods such as bread (the number of slices per day), low calorie drinks, cola, tea and coffee (the number of cups). The type of milk (full-fat, semi-skimmed, other), bread (white, wholemeal, other) and fat spreads (butter, margarine, other) usually consumed were also recorded.
The data on frequency of consumption were numerically transformed into times consumed per week, to give a quantitative meaning to the frequency categories, as follows: (i) 0; (ii) 0.5; (iii) 2; (iv) 5.5 (v) 10 times per week. Daily foods were converted to times per week and recoded accordingly to keep similar quantitative values. All variables used in the analysis were standardised by subtracting the mean and dividing by the standard deviation for each variable [42]. The questionnaires were modified slightly over time due to changes in the availability of various foods [17]. Separate categories were created at later ages for coated poultry and fish products, vegetarian pies and tuna, which had previously been included in other categories. Therefore, as time progressed, additional foods and drinks were included in the analysis. Before entry into the PCA, some food groups were combined and a detailed list of food groups is presented in the Supplementary File in Table 1. Thus, the number of food items included in the analysis varied by time points e.g. pregnancy (43 items), 4 years (51 items), 8 years (49 items) and 12 years post-pregnancy (48 items).
Maternal diet from pregnancy to post-pregnancy 12-years
Maternal dietary patterns at 32 weeks of gestation and at 4 years of child’s age have been previously identified in this cohort using principal component analysis (PCA) with varimax rotation. Detail of the identified dietary patterns has been described elsewhere [17, 42]. In brief, five DPs were identified in pregnancy and four DPs at 4 years post-pregnancy. The DPs identified had high positive loading on the following foods and were labelled accordingly: ‘‘Health conscious/healthy’’: salad, fresh fruit, rice, pasta, fish, pulses and non-white bread. ‘‘Traditional’’: all types of vegetables and some items of poultry and red meat. ‘‘Processed’’: white bread, meat pies, sausages, burgers, roasted potatoes, chips, crisps, baked beans. ‘‘Vegetarian’’: meat substitutes, pulses, nuts, herbal tea, with high negative loadings on all meats. ‘‘Confectionery’’: chocolate, sweets, biscuits, cakes, puddings. The traditional dietary pattern component was not extracted at 4-years post-pregnancy [17]. The mothers completed two additional FFQ at 8- and 12-years post-pregnancy. These FFQs were again administered via self-completion questionnaires and an identical analytical technique to that used for the pregnancy and 4-years data was applied. This was PCA with varimax rotation used to analyse standardised food items, described in detail elsewhere [42].
Covariates
Covariates were selected based on previous relevant studies; they were obtained from self-completed postal questionnaires sent during pregnancy [42,43,44]. These include maternal social characteristics at the time of pregnancy i.e. maternal age, educational attainment, social class, marital status and ethnicity, maternal behavioural characteristics i.e. smoking and alcohol intake; and perinatal characteristics i.e. number of previous pregnancies (parity), and pre-pregnancy body mass index (BMI). Maternal educational attainment was assessed in three categories, Low: (None/Vocational or < O level), Medium: O level (school certificate obtained at age 16 years) and High: (A level (examination obtained aged at 18 years) or degree or above). Social class was categorised according to maternal occupation using standard UK classifications of occupation including class I (highest), II, III-non-manual, III-manual, IV and V (lowest) [45] and grouped into three categories (high, middle and low social class). Employment status was categorised as “unemployed” or “employed”; women were classified as “unmarried” or “ever married”, and ethnic group was dichotomised into “white” and “non-white”.
Mothers were asked to report alcohol consumption before their current pregnancy by questionnaire at 18 weeks of gestation as: never, < 1 glass/week, at least 1 glass/week, 1–2 glasses/day, at least 3–9 glasses/day and at least 10 glasses/day. The total glasses/week or day were grouped (never/ < 1 glass/week, 1 + glass/week and 1 or more glasses/day) [46]. Women were categorised into non-smokers, light smokers (less than 10 cigarettes per day) and heavy smokers (more than 10 cigarettes per day) based on their report at 32 weeks of pregnancy [47]. Maternal pre-pregnancy weight and height were self-reported and BMI was calculated as weight (kg)/height (m2). Pre-pregnancy BMI was categorised according to the World Health Organization as “underweight (< 18.5 kg/m2)”, “normal (18.5 and < 25 kg/m2)”, “overweight (> 25.0 and < 30 kg/m2),” and “obesity (≥ 30 kg/m2)” [48].
Statistical analysis
Using the DP scores constructed at each time point, group-based trajectory modelling (GBTM) was applied to evaluate trajectories of DPs [49]. This method identifies distinct groups of DPs over the four time points [50]. In brief, GBTM is a latent class growth model (LCGM) designed to identify subgroups within the study population that share a similar developmental trajectory for an outcome over time; that means, grouping individuals following analogous trajectories on specific DPs over time [50]. This study modelled DPs trajectories among mothers who had information at all four time points for the two dietary patterns which persisted; “healthy” and “processed”. First, a base model of trajectory was constructed to determine the number of groups, the order of the polynomial functions and group membership of the participants at each time point. Then, model fitting and inference were carried out via GBMT with the “Traj” plugin command in Stata [51] which implements a Newton–Raphson optimization algorithm for maximum likelihood estimation [52]. The model selection exercise was based on the Bayesian information criterion (BIC) and polynomial order.
A censored normal distribution appropriate to continuous data was used to generate representative trajectory curves that best fit the distinct trajectory groups for the overall study population [49]. It cannot be assumed in GBTM that all trajectories follow the same longitudinal changes in DPs, therefore, the shape of trajectory can be modelled as either intercept, linear, quadratic and cubic during model fitting exercise [24]. The number of trajectory groups and the polynomial order, which determines the shape of each trajectory, were selected based on several criteria, including: (i) the model’s BIC, (ii) the statistical significance of the polynomial coefficients; (iii) the sample size in each group; (iv) a close correspondence between the estimated probability of group membership presented as an average posterior probability (> 0.7) and the odds of correct classification (> 5) for all groups [50, 53]. A three-group model with polynomial distribution satisfied the theoretical and statistical criteria and was selected for inclusion in the main model. Output from the polynomial distributions is presented in the Supplementary file Table S1 and Table S2. Two separate trajectories were constructed one for each DP.
The distribution of maternal characteristics (collected during pregnancy) were presented as frequencies and percentages and the distribution of categorical variables were compared using chi-squared tests. Multinomial logistic regression was used to examine the relationship between these mutually adjusted characteristics and membership of the dietary trajectories. The likelihood of a woman following a specific DP trajectory in relation to maternal characteristics, was expressed using relative risk ratios (RRR). The characteristics investigated were maternal age, education, employment status, marital status, social class, ethnicity, parity, pre-pregnancy BMI, smoking and alcohol behaviours. All statistical analyses were carried out using Stata/SE (STATA, Version 16.0, StataCorp, College Station, TX, USA).
Results
A total of 12,191 women had dietary data at 32 weeks of gestation, 9598 women at 4 years, 7822 women at 8 years and 6932 women at 12 years post-pregnancy. Complete data at all four time points was available for 5336 women. Table 1 presents the baseline socio-demographic, behavioural and perinatal characteristics of the women at 32 weeks of gestation for those with and without complete data. The women included in the analysis were more likely to have higher educational attainment, belong to a higher social class and have been older at the birth of the child than those excluded (Table 1). They were more likely to be employed, married, of white ethnicity, be non-smokers, consume alcohol, have a BMI within the normal range and be experiencing their first pregnancy.
Three dietary patterns were chosen to best describe the DPs of mothers at 8 and 12 years post-pregnancy compared to 5 and 4 DPs extracted in pregnancy and 4 years post-pregnancy, respectively [17, 42]. More details of the DPs identified in this study are shown in Supplementary Table S3. Two DPs very similar to those in pregnancy were extracted at both 8 and 12 years. At all four time points from pregnancy to post-pregnancy, the first component loaded highly on brown/wholemeal bread, rice, pasta, fresh fruit, salad, fruit juice, fish, poultry, cheese, pulses, plain potatoes, leafy green and other vegetables, carrots, root vegetables, fresh fruits and whole grain breakfast cereal and negatively on white bread and was labelled as “healthy”. The “processed” pattern was identified as third or second components during pregnancy and later time points. This pattern had high factor loadings for white bread, coated poultry products, breaded and battered white fish, biscuits, baked beans, puddings, ice-cream, cakes/buns, meat pies, sausages, pizza, eggs, chips and roast potatoes, sweets, chocolate and fried foods. These two dietary patterns persistently emerged across all time points for women after pregnancy. A new pattern was observed at both later ages, labelled as “high meat”, it had high factor loadings for poultry, red meats, cold meats, coated poultry products and meat pies. The “confectionery”, “traditional”, and “vegetarian” patterns observed at previous timepoints were not evident at later ages.
The correlations between the DP scores at each time point are summarized in Table 2. The “healthy” dietary pattern correlated relatively strongly across all time points, the correlation between pregnancy and 8 years being the lowest (0.34) and between 8 and 12 years being the highest (0.61). The “processed” DPs showed slightly lower correlation coefficients over time ranging from 0.22 between pregnancy and 12 years to 0.57 between 4 and 8 years. For the most part the “healthy” and “processed” DPs were either uncorrelated or very weakly negatively correlated with each other at different time points, however the “healthy” DP in pregnancy showed moderate negative correlations with the “processed” DP at 4 (− 0.31) and 8 (− 0.27) years post-pregnancy. The four-remaining patterns were not consistently derived and showed various correlations, the most notable being negative correlations between the “vegetarian” DPs at the first two time points and the “high meat” DP at the fourth (− 0.41 and − 0.48, respectively).
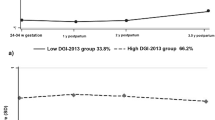
Figure 1 illustrates that women were allocated to three distinct DP trajectories for each of the two consistent DPs (“healthy” and “processed”) over the 12 years since pregnancy. For the healthy DP trajectory, women in Group 1 (n = 1971, 37.4%) had an initially negative DP score with a stable progression which remained negative across time (named “lower healthy DP trajectory”); women in Group 2 (n = 2918, 53.4%) had a moderate initial DP score with a slow decrease thereafter (named as “moderately healthy DP trajectory”); and, women in Group 3 (n = 447, 9.2%) had the highest DP score and increased over the time (named as “higher healthy DP trajectory”). Similarly, women were allocated to one of three trajectory groups for the processed DP: women in Group 1 (n = 3171, 58.6%) had a negative DP score initially, with a slight increase thereafter, but it remained negative across the time points (named as “lower processed DP trajectory”); women in Group 2 (n = 2011, 38.1%) had an initial moderate score with a slight increase and stable thereafter (named “moderately processed DP trajectory”); however, women in Group 3 (n = 154, 3.3%) had the highest processed DP score initially and rapidly increased over the time (labelled as “higher processed DP trajectory”). The distribution of maternal characteristics in women following the “healthy” and “processed” DP trajectories are presented in the Supplementary file Tables S4 and S5.
The associations between maternal baseline characteristics and DP trajectories are presented in Tables 3 and 4. For the healthy DP trajectories women following the ‘higher healthy DP trajectory’ were the reference group. In the fully adjusted models, women on the ‘lower healthy DP trajectory’ were more likely to be from the middle or low social class, with medium or low educational attainment and have smoked heavily in pregnancy and their child was less likely to have been first born compared to women on the ‘higher healthy DP trajectory’. Maternal characteristics did not differ between the ‘higher’ and ‘moderately’ healthy DP trajectories in the adjusted model. For the processed DPs, the comparisons were with women following the ‘lower processed DP trajectory’. Women who followed the ‘moderately processed DP trajectory’ were more likely to be in of middle or low social class, have low educational attainment and having been exposed to obesity prior to pregnancy. Additionally, these women were slightly more like to have been light smokers and more likely to have been aged over 20 years or to have been regular alcohol drinkers compared to women in the reference trajectory. Again, women in the ‘higher processed DP trajectory’ were more likely to have a medium or low educational attainment, to have been a heavy smoker during pregnancy and were slightly more likely to be in the middle social class compared to women on the ‘low processed DP trajectory’. However, they were less likely to have been aged over 30 years when pregnant.
Discussion
This study models group-based trajectories of longitudinal dietary patterns among British women from pregnancy across multiple timepoints post-pregnancy. Women’s dietary intakes were collected prospectively in ALSPAC four times from pregnancy to 12 years post-pregnancy. Six different dietary patterns were derived using PCA analysis over the four time points. A “healthy” and a “processed” DP were persistent at each time and used to explore the trajectories of the women’s diets across time. Three trajectories were identified for each of the two patterns.
For the “healthy” DP trajectories, the majority (53.4%) of women followed the “moderately healthy DP trajectory”. This implies that this group of women have a moderate score on the healthy DP at each time point. A further 37.4% of women followed a “lower healthy DP trajectory” where they had a lower score on the healthy DP at each time point. The remaining women (9.2%) were on a “higher healthy trajectory”, representing higher scores on the healthy DP across time. This is the smallest group and we can speculate that these women should have a better health profile than the group who had followed the “lower healthy DP trajectory” throughout the period of interest. Further research will be necessary to confirm this. For the “processed” trajectory, most women followed the “lower processed DP trajectory” (58.6%)”. These women had a lower score on the processed DP throughout. The “moderately processed DP trajectory” (38.1%) was the second largest trajectory group with women having moderate scores on the “processed” DP at all time points. While the “higher processed DP trajectory” was followed by only 3.3% of the women, this trajectory implies the consumption of a highly processed diet at each time point. Further research is necessary to understand the health effects on women who were following the “higher processed DP trajectory” over time.
Of the remaining DPs in pregnancy “confectionary” and “vegetarian” were not derived after 4 years post-pregnancy and the “traditional” DP only occurred in pregnancy. A new DP emerged at 8 years post-pregnancy and continued at 12 years it was named “high meat”. These findings suggest that some DPs emerged in this cohort were not necessarily stable over time. A shift toward a more meat-based diet among women supports the global view of nutritional transition towards animal-based diets which may be linked to increased risk of nutrition related NCDs [54,55,56]. Further investigation of these unstable patterns is warranted.
Our study found that women were more likely to have consistently low or moderate scores on a DP across time than consistently high scores on that pattern. Only a small number of women who started with a high “healthy” DP score, remained high over time, thus having a “healthy” dietary pattern throughout. This was also true for the “processed” DP trajectories. Women with medium or low educational attainment were more likely to follow the “lower healthy” and “higher processed” DP trajectories in this cohort. This level of stability in dietary trajectories and association with the educational attainment of women, was similar to another British study the Southampton Women’s Survey (SWS) that examined longitudinal changes in dietary quality trajectories in women from pre-pregnancy to 8–9 years post-pregnancy [24]. The stability of DP trajectories identified in our study are also in line with studies reporting dietary shifts over time among Chinese adults, although the identified dietary patterns differed from those in our study [27, 32, 57]. This may suggest that the studies that identified changes in dietary intake from pregnancy to post-pregnancy may be due to short-term changes related to maternal motivation to make changes during pregnancy and while breastfeeding their newborn [20].
A limited number of studies have investigated changes in DPs among adult populations using group-based trajectory modelling over long time periods and diverse dietary trajectories have emerged [27, 28, 32, 57,58,59]. DP trajectories have been found to vary between studies in relation to the sex of the participants, socioeconomic background, ethnic group and by cultural diversity. Variations in DPs between studies are likely to be due to cultural differences in dietary habits, different analytical approaches used to identify the DPs as well as differences in the number and type of food items included in the analysis [60]. A large variation in DP trajectories has been reported both between and within populations [27, 32]. Thus, earlier studies that have demonstrated divergence in DP trajectories may not be directly comparable with our study [32, 59]. Given the paucity of evidence, more research is needed among women after pregnancy to understand maternal dietary trajectories across the life course.
Compared to women following the “higher healthy DP trajectory”, maternal characteristics in pregnancy did not differ in those following the “moderately healthy DP trajectory”. However, women following the “lower healthy DP trajectory” were more likely to have smoked heavily in pregnancy. A similar difference occurred between women following the “higher processed DP trajectory” compared those following the “lower processed DP trajectory”. These results suggest that smoking in pregnancy was associated with having a less favourable DP at all time points. These findings are consistent with previous studies showing an association between smoking and unhealthy dietary intake among women [24, 61,62,63,64]. Again, a study on smoking and dietary intake among Norwegian pregnant women found that women who smoked during pregnancy consumed significantly less healthy foods and more unhealthy foods compared to non-smoking women [62]. Importantly, women who smoked tended to have a less nutritious dietary intake [62], a higher fat and energy intake and increased craving for highly palatable foods [63, 64] compared to non-smokers throughout pregnancy.
There were social class differences between women following the different DP trajectories. Women who belonged to the lower social class had a higher chance of following the “lower healthy DP trajectory” compared to following either the higher or moderately healthy DP trajectories. Furthermore, women with a low or middle social class background were more likely to follow the “moderately” or “higher processed DP trajectory” rather than following the “lower processed DP trajectory”. People with lower social status are likely to have less disposable income and evidence suggests that lower income groups tend to fall into lower quintiles for food expenditure [65]. Another study also found that lower quality diets tended to be consumed by economically disadvantage populations [66]. Our findings align with British SWS cohort which also reported that women following a poor diet quality trajectory were more likely to be in a lower social class [24]. These associations may be due to the high price of healthy foods, limits on budgets for food, constraints of work-life balance making it more difficult to cook from scratch and leading to the purchase of ready-packed foods often of low nutritional quality [32, 65,66,67,68].
The major strength of this study is its prospective cohort design, over 12 years of follow-up (from pregnancy to post-pregnancy) and complete dietary information from more than 5000 women. The ALSPAC cohort provided a unique opportunity to explore longitudinal dietary patterns and dietary trajectories because of its large sample size and long follow-up. The use of dietary patterns at 4 time points from pregnancy allowed the assessment of dietary stability over time and the development of dietary trajectories among British women. Additionally, GBMT modelling proved to be an important technique when classifying the dietary patterns into interpretable trajectories. A wide range of potential confounders was available to the study.
Nevertheless, this study has some limitations that need to be recognised. Firstly, data on dietary intake was self-reported and hence may be susceptible to measurement bias and inaccuracies. However, the use of FFQs is well-accepted for dietary assessment in observational nutritional science [69]. Secondly, the number of food items and PCA loading scores were slightly different at each time point, due to slight modifications of the FFQ over time e.g. additional food and drink items [17, 70]. Further, some number of women who completed the pregnancy questionnaire failed to complete follow-up questionnaires thus reducing the size and changing the composition of the cohort. This led to the decision to only use data from women with complete dietary data across four time points in this study while providing Table 1, pointing out the likely biases due to the reduced sample size so that the reader can take them into consideration. The biases in our study were very similar to those in SWS a British cohort study in a different part of the country [24] and the fact that the findings were very similar should provide confidence that they are generalisable in a British context. Although our study identified some unstable DPs in the mothers’ diets, we were unable to explore these fully in this analysis.
Conclusion
Following pregnancy, continuing with a healthy and optimal diet during post-pregnancy is important to support maternal health and wellbeing and for the child to learn healthy eating practices. In our study, maternal DPs were found to have some variability from pregnancy to later time points, with some evidence of a move towards higher consumption of a meat-based diet. However, within the persistent “healthy” and “processed” DPs, dietary trajectories were relatively stable over the 12 years post-pregnancy. Our findings add to the evidence for strengthening and improving maternal care during pregnancy and for continued counselling to mothers regarding healthy eating and smoking cessation while bringing up their children.
Our findings suggest that it is advisable that health professionals target smoking cessation at the same time as promoting a healthy diet in antenatal care. If resources allowed healthy eating and ante-smoking education that started well before pregnancy may prove even more beneficial to family health. Also, follow up support for healthy eating after the birth of the child which is likely to benefit the mother and her family. To increase effectiveness, introducing a triage system to prioritise socially and economically disadvantaged women with risk behaviours would be beneficial for promoting life course healthy eating among women.
Data availability
ALSPAC data used in this paper are available upon application to the Executive of ALSPAC (alspac-exec@bristol.ac.uk). The ALSPAC study website contains details of all the data that is available through a fully searchable data dictionary and variable search tool (http://www.bristol.ac.uk/alspac/researchers/our-data/). The ALSPAC data management plan and details of the policy regarding data sharing are also publicly available (http://www.bristol.ac.uk/alspac/researchers/dataaccess/documents/alspac-data-management-plan.pdf).
References
Togo P, Osler M, Sørensen T, Heitmann B (2004) A longitudinal study of food intake patterns and obesity in adult Danish men and women. Int J Obes 28(4):583–593
McNaughton SA, Mishra GD, Brunner EJ (2008) Dietary patterns, insulin resistance, and incidence of type 2 diabetes in the Whitehall II Study. Diabetes Care 31(7):1343–1348
Sonnenberg L, Pencina M, Kimokoti R, Quatromoni P, Nam BH, D’agostino R, Meigs JB, Ordovas J, Cobain M, Millen B (2005) Dietary patterns and the metabolic syndrome in obese and non-obese Framingham women. Obes Res 13(1):153–162
Millen BE, Quatromoni PA, Nam B-H, O’Horo CE, Polak JF, D’Agostino RB (2002) Dietary patterns and the odds of carotid atherosclerosis in women: the Framingham Nutrition Studies. Prev Med 35(6):540–547
Nettleton JA, Schulze MB, Jiang R, Jenny NS, Burke GL, Jacobs DR Jr (2008) A priori-defined dietary patterns and markers of cardiovascular disease risk in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 88(1):185–194
Nanri A, Mizoue T, Shimazu T, Ishihara J, Takachi R, Noda M, Iso H, Sasazuki S, Sawada N, Tsugane S (2017) Dietary patterns and all-cause, cancer, and cardiovascular disease mortality in Japanese men and women: the Japan public health center-based prospective study. PLoS ONE 12(4):e0174848
WH Organization (2003) Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation, vol 916. WHO World Health Organization, Geneva
Itani L, Radwan H, Hashim M, Hasan H, Obaid RS, Al Ghazal H, Al Hilali M, Rayess R, Mohamed HJJ, Hamadeh R (2020) Dietary patterns and their associations with gestational weight gain in the United Arab Emirates: results from the MISC cohort. Nutr J 19(1):1–12
Bayol S, Simbi B, Bertrand J, Stickland N (2008) Offspring from mothers fed a ‘junk food’diet in pregnancy and lactation exhibit exacerbated adiposity that is more pronounced in females. J Physiol 586(13):3219–3230
Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM (2020) Adherence to the Healthy Eating Index–2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr 150(2):312–321
Monthé-Drèze C, Rifas-Shiman SL, Aris IM, Shivappa N, Hebert JR, Sen S, Oken E (2021) Maternal diet in pregnancy is associated with differences in child body mass index trajectories from birth to adolescence. Am J Clin Nutr 113(4):895–904
van den Broek M, Leermakers ET, Jaddoe VW, Steegers EA, Rivadeneira F, Raat H, Hofman A, Franco OH, Kiefte-de Jong JC (2015) Maternal dietary patterns during pregnancy and body composition of the child at age 6 y: the Generation R Study. Am J Clin Nutr 102(4):873–880
Chia A-R, Chen L-W, Lai JS, Wong CH, Neelakantan N, van Dam RM, Chong MF-F (2019) Maternal dietary patterns and birth outcomes: a systematic review and meta-analysis. Adv Nutr 10(4):685–695
Koletzko B, Godfrey KM, Poston L, Szajewska H, Van Goudoever JB, De Waard M, Brands B, Grivell RM, Deussen AR, Dodd JM (2019) Nutrition during pregnancy, lactation and early childhood and its implications for maternal and long-term child health: the early nutrition project recommendations. Ann Nutr Metab 74(2):93–106
de Waard M, Brands B, Kouwenhoven SM, Lerma JC, Crespo-Escobar P, Koletzko B, Zalewski BM, van Goudoever JB (2017) Optimal nutrition in lactating women and its effect on later health of offspring: a systematic review of current evidence and recommendations (EarlyNutrition project). Crit Rev Food Sci Nutr 57(18):4003–4016
Marshall NE, Abrams B, Barbour LA, Catalano P, Christian P, Friedman JE, Hay WW Jr, Hernandez TL, Krebs NF, Oken E (2022) The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol 226(5):607–632
Northstone K, Emmett PM (2008) A comparison of methods to assess changes in dietary patterns from pregnancy to 4 years post-partum obtained using principal components analysis. Br J Nutr 99(5):1099–1106
Poulain T, Spielau U, Vogel M, Dathan-Stumpf A, Körner A, Kiess W (2021) Changes in diet from pregnancy to one year after birth: a longitudinal study. BMC Pregnancy Childbirth 21(1):1–10
Hillier SE, Olander EK (2017) Women’s dietary changes before and during pregnancy: a systematic review. Midwifery 49:19–31
Lee YQ, Loh J, Ang RSE, Chong MF-F (2020) Tracking of maternal diet from pregnancy to postpregnancy: a systematic review of observational studies. Curr Dev Nutr 4(8):nzaa118
Murrin C, Shrivastava A, Kelleher C (2013) Maternal macronutrient intake during pregnancy and 5 years postpartum and associations with child weight status aged five. Eur J Clin Nutr 67(6):670–679
Cuco G, Fernandez-Ballart J, Sala J, Viladrich C, Iranzo R, Vila J, Arija V (2006) Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr 60(3):364–371
Sotres-Alvarez D, Herring AH, Siega-Riz A-M (2013) Latent transition models to study women’s changing of dietary patterns from pregnancy to 1 year postpartum. Am J Epidemiol 177(8):852–861
Dalrymple KV, Vogel C, Godfrey KM, Baird J, Harvey NC, Hanson MA, Cooper C, Inskip HM, Crozier SR (2022) Longitudinal dietary trajectories from preconception to mid-childhood in women and children in the Southampton Women’s Survey and their relation to offspring adiposity: a group-based trajectory modelling approach. Int J Obes 46(4):758–766
Batis C, Sotres-Alvarez D, Gordon-Larsen P, Mendez MA, Adair L, Popkin B (2014) Longitudinal analysis of dietary patterns in Chinese adults from 1991 to 2009. Br J Nutr 111(8):1441–1451
Zhang J, Wang Z, Du W, Huang F, Jiang H, Bai J, Zhang X, Zhang B, Wang H (2021) Twenty-five-year trends in dietary patterns among Chinese adults from 1991 to 2015. Nutrients 13(4):1327
Cao Y, Xu X, Shi Z (2020) Trajectories of dietary patterns, sleep duration, and body mass index in china: a population-based longitudinal study from china nutrition and health survey, 1991–2009. Nutrients 12(8):2245
Batis C, Mendez MA, Sotres-Alvarez D, Gordon-Larsen P, Popkin B (2014) Dietary pattern trajectories during 15 years of follow-up and HbA1c, insulin resistance and diabetes prevalence among Chinese adults. J Epidemiol Community Health 68(8):773–779
Gao M, Wang F, Shen Y, Zhu X, Zhang X, Sun X (2018) Trajectories of Mediterranean diet adherence and risk of hypertension in China: results from the CHNS study, 1997–2011. Nutrients 10(12):2014
Li M, Shi Z (2017) Dietary pattern during 1991–2011 and its association with cardio metabolic risks in Chinese adults: the China health and nutrition survey. Nutrients 9(11):1218
Smithers LG, Golley RK, Mittinty MN, Brazionis L, Northstone K, Emmett PM, Lynch JW (2013) Do dietary trajectories between infancy and toddlerhood influence IQ in childhood and adolescence? Results from a prospective birth cohort study. PLoS ONE 8(3):e58904
Zhang J, Wang H, Wang Z, Huang F, Zhang X, Du W, Su C, Ouyang Y, Li L, Bai J (2021) Trajectories of dietary patterns and their associations with overweight/obesity among Chinese Adults: China Health and Nutrition Survey 1991–2018. Nutrients 13(8):2835
Lipsky LM, Haynie DL, Liu D, Chaurasia A, Gee B, Li K, Iannotti RJ, Simons-Morton B (2015) Trajectories of eating behaviors in a nationally representative cohort of US adolescents during the transition to young adulthood. Int J Behav Nutr Phys Act 12(1):1–11
Ness AR (2004) The Avon Longitudinal Study of Parents and Children (ALSPAC)—a resource for the study of the environmental determinants of childhood obesity. Eur J Endocrinol 151(Suppl 3):U141–U149
Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Henderson J, Macleod J, Molloy L, Ness A (2013) Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol 42(1):97–110
Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G (2013) Cohort profile: the ‘children of the 90s’—the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol 42(1):111–127
Golding J, Pembrey M, Jones R (2001) ALSPAC–the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinatal Epidemiol 15(1):74–87
Northstone K, Lewcock M, Groom A, Boyd A, Macleod J, Timpson N, Wells N (2019) The Avon Longitudinal Study of Parents and Children (ALSPAC): an update on the enrolled sample of index children in 2019. Wellcome Open Res 4:51
Emmett P (2009) Dietary assessment in the Avon longitudinal study of parents and children. Eur J Clin Nutr 63(1):S38–S44
Northstone K, Emmett PM, Rogers I (2008) Dietary patterns in pregnancy and associations with nutrient intakes. Br J Nutr 99(2):406–415
Rogers I, Emmett P (1998) Diet during pregnancy in a population of pregnant women in South West England. Eur J Clin Nutr 52(4):246–250
Northstone K, Emmett P, Rogers I (2008) Dietary patterns in pregnancy and associations with socio-demographic and lifestyle factors. Eur J Clin Nutr 62(4):471–479
Northstone K, Emmett P (2010) Dietary patterns of men in ALSPAC: associations with socio-demographic and lifestyle characteristics, nutrient intake and comparison with women’s dietary patterns. Eur J Clin Nutr 64(9):978–986
Emmett PM, Jones LR, Golding J (2015) Pregnancy diet and associated outcomes in the Avon Longitudinal Study of Parents and Children. Nutr Rev 73(suppl 3):154–174
Censuses OoP, Surveys (1991) Standard Occupational Classification. Volume 3. Hmso London
Easey KE, Timpson NJ, Munafò MR (2020) Association of prenatal alcohol exposure and offspring depression: a negative control analysis of maternal and partner consumption. Alcohol Clin Exp Res 44(5):1132–1140
Howe LD, Matijasevich A, Tilling K, Brion M-J, Leary SD, Smith GD, Lawlor DA (2012) Maternal smoking during pregnancy and offspring trajectories of height and adiposity: comparing maternal and paternal associations. Int J Epidemiol 41(3):722–732
Sharp GC, Lawlor DA, Richmond RC, Fraser A, Simpkin A, Suderman M, Shihab HA, Lyttleton O, McArdle W, Ring SM (2015) Maternal pre-pregnancy BMI and gestational weight gain, offspring DNA methylation and later offspring adiposity: findings from the Avon Longitudinal Study of Parents and Children. Int J Epidemiol 44(4):1288–1304
Nagin DS (2010) Group-based trajectory modeling: an overview. Handbook of quantitative criminology. Springer, pp 53–67
Nagin DS, Odgers CL (2010) Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 6:109–138
Jones BL, Nagin DS (2013) A note on a Stata plugin for estimating group-based trajectory models. Sociol Methods Res 42(4):608–613
Chu M-KM, Koval JJ (2014) Trajectory modeling of longitudinal binary data: application of the EM algorithm for mixture models. Commun Stat-Simul Comput 43(3):495–519
Wieczorek M, Rotonda C, Guillemin F, Rat A-C (2018) Trajectories of pain, physical function and physical activity components in patients with symptomatic knee and hip osteoarthritis: a group-based multi-trajectory approach. Rev Epidemiol Sante Publique 66:S322
Popkin B, Adair L, Ng S (2017) NOW AND THEN: the global nutrition transition: the pandemic of obesity in developing countries. Nutrients 58(1):1–10
Popkin BM (1993) Nutritional patterns and transitions. Popul Dev Rev 19:138–157
Otter C (2012) The British nutrition transition and its histories. Hist Compass 10(11):812–825
Wu F, Pahkala K, Juonala M, Rovio SP, Sabin MA, Rönnemaa T, Buscot M-J, Smith KJ, Männistö S, Jula A (2021) Dietary pattern trajectories from youth to adulthood and adult risk of impaired fasting glucose: a 31-year cohort study. J Clin Endocrinol Metab 106(5):e2078–e2086
Xu X, Byles J, Shi Z, McElduff P, Hall J (2016) Dietary pattern transitions, and the associations with BMI, waist circumference, weight and hypertension in a 7-year follow-up among the older Chinese population: a longitudinal study. BMC Public Health 16(1):743
Appannah G, Murray K, Trapp G, Oddy WH, Ambrosini GL (2020) Dietary pattern trajectories across adolescence and young adulthood and their determinants
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9
Haste F, Brooke O, Anderson H, Bland J (1991) The effect of nutritional intake on outcome of pregnancy in smokers and non-smokers. Br J Nutr 65(3):347–354
Trygg K, Lund-Larsen K, Sandstad B, Hoffman HJ, Jacobsen G, Bakketeig LS (1995) Do pregnant smokers eat differently from pregnant non-smokers? Paediatr Perinat Epidemiol 9(3):307–319
Pepino MY, Finkbeiner S, Mennella JA (2009) Similarities in food cravings and mood states between obese women and women who smoke tobacco. Obesity 17(6):1158–1163
Pepino MY, Mennella JA (2014) Cigarette smoking and obesity are associated with decreased fat perception in women. Obesity 22(4):1050–1055
Pechey R, Monsivais P (2016) Socioeconomic inequalities in the healthiness of food choices: exploring the contributions of food expenditures. Prev Med 88:203–209
Darmon N, Drewnowski A (2008) Does social class predict diet quality? Am J Clin Nutr 87(5):1107–1117
Wall CR, Gammon CS, Bandara DK, Grant CC, Atatoa Carr PE, Morton S (2016) Dietary patterns in pregnancy in New Zealand—influence of maternal socio-demographic, health and lifestyle factors. Nutrients 8(5):300
Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S (2020) Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr 124(11):1133–1144
Cui Q, Xia Y, Wu Q, Chang Q, Niu K, Zhao Y (2021) A meta-analysis of the reproducibility of food frequency questionnaires in nutritional epidemiological studies. Int J Behav Nutr Phys Act 18(1):1–18
Forbes LE, Graham JE, Berglund C, Bell RC (2018) Dietary change during pregnancy and women’s reasons for change. Nutrients 10(8):1032
Acknowledgements
The authors of this study are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The UK Medical Research Council and Wellcome (Grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. A full list of grant funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). This research was specifically supported by ARC Centre of Excellence for Children and Families over the Life Course and Institute for Social Science Research (ISSR). SP is supported by an Australian Government Research Training Program (RTP) Scholarship funded by the University of Queensland for PhD study. The study funders had no role in the study design, data collection or analysis, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
SP, PE and AAM formulated the research question, designed the study and were responsible for planning data analysis. SP compiled and prepared the analysis. SP analysed data with supervision from PE, YF and AAM. SP received additional input from KN on data analysis who derived the original dietary pattern scores. All authors (PE, NT, KN, DM, YF, MMH and AAM) contributed to interpretating of the results, manuscript writing and critically reviewed the manuscript. All authors read and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no potential conflict of interest.
Ethical approval
ALSPAC obtained ethical approval from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committee (ALEC) and conformed to the Declaration of Helsinki. Research Ethics Committee approval reference published by ALSPAC are available through the website (http://www.bristol.ac.uk/alspac/researchers/research-ethics/). This present study was approved by the Human Research Ethics Review Office, The University of Queensland [Approval number: 2022/HE000707].
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pervin, S., Emmett, P., Northstone, K. et al. Trajectories of dietary patterns from pregnancy to 12 years post-pregnancy and associated maternal characteristics: evidence from the Avon Longitudinal Study of Parents and Children. Eur J Nutr 62, 2763–2777 (2023). https://doi.org/10.1007/s00394-023-03185-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03185-x