Abstract
Purpose
Whether anemia type modifies the risk of pregnancy and newborn outcomes and the effectiveness of iron supplementation is unclear. We examined the association of iron deficiency anemia (IDA) and non-iron deficiency anemia (NIDA) on the risks of these outcomes and the extent to which anemia type modifies the impact of prenatal iron supplementation.
Methods
This was a secondary analysis of a placebo-controlled trial of iron supplementation among 1450 HIV-negative women in Tanzania. Eligibility criteria included gestational age < 27 weeks, hemoglobin > 85 g/L, and ferritin > 12 µg/L. Individuals were categorized as non-anemia, IDA or NIDA using hemoglobin, ferritin and CRP. Analyses were conducted using regression models and likelihood ratio tests.
Results
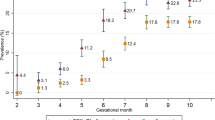
Compared to the non-anemia group, delivery hemoglobin was lower by 15 g/L (95% CI 10.9, 19.3) in the baseline IDA group, and 7.3 g/L (95% CI 3.1, 11.5) in the baseline NIDA group. The RRs of anemia severity, iron deficiency, placental malaria, stillbirths, perinatal mortality, birthweight, and preterm birth were not different among women in the baseline NIDA group (vs. non-anemia) compared to the baseline IDA group (vs. non-anemia). The difference in the mean delivery hemoglobin for iron supplementation and placebo arms was 8 g/L (95% CI 6, 11) in the non-anemia group, 7 g/L (95% CI 2, 13) in the NIDA group, and 16 g/L (95% CI 10, 22) in the IDA group.
Conclusion
Iron supplementation is effective even among pregnant women with NIDA.
Trial registration
NCT01119612 (May 7, 2010).

Similar content being viewed by others
Abbreviations
- ACD:
-
Anemia of chronic disease
- AI:
-
Anemia of inflammation
- AIDS:
-
Acquired Immune Deficiency Syndrome
- ART:
-
Antiretroviral therapy
- BMI:
-
Body Mass Index
- CBC:
-
Complete blood count
- CI:
-
Confidence Interval
- CKD:
-
Chronic kidney disease
- CRP:
-
C-reactive protein
- ELISA:
-
Enzyme Linked Immunosorbent Assay
- HAART:
-
Highly Active Antiretroviral Therapy
- HAND:
-
HIV-associated neurocognitive disorder
- HIV:
-
Human Immunodeficiency Virus
- HR:
-
Hazard ratio
- ID:
-
INTERGROWTH: International Fetal and Newborn Growth Consortium for the 21st Century
- IDA:
-
Iron deficiency anemia
- IQR:
-
Interquartile range
- IRA:
-
Iron-restricted anemia
- LMIC:
-
Low and Middle Income Countries
- MRC:
-
Medical Research Council
- NIDA:
-
Non-Iron Deficiency anemia
- NTBI:
-
Non-transferrin bound iron
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- PLWHIV:
-
People living with HIV
- RCT:
-
Randomized controlled trial
- RR:
-
Relative risk
- SD:
-
Standard deviation
- SE:
-
Standard error
- SGA:
-
Small-for-gestational age
- sTfR:
-
Soluble Transferrin receptor
- TB:
-
Tuberculosis
- TIBC:
-
Total Iron Binding Capacity
- ZPP:
-
Zinc protoporphyrin
References
Gardner W, Kassebaum N (2020) Global, regional, and national prevalence of anemia and its causes in 204 countries and territories, 1990–2019. Curr Develop Nutr 4(2):830–830
Weze K, Abioye AI, Obiajunwa C, Omotayo M (2021) Spatio-temporal trends in anemia among pregnant women, adolescents and preschool children in sub-Saharan Africa. Public Health Nutrition 24(12):3648–3661
Msuya SE, Hussein TH, Uriyo J, Sam NE, Stray-Pedersen B (2011) Anaemia among pregnant women in northern Tanzania: prevalence, risk factors and effect on perinatal outcomes. Tanzan J Health Res 13(1):33–39
Petry N, Olofin I, Hurrell RF, Boy E, Wirth JP, Moursi M, Donahue Angel M, Rohner F (2016) The Proportion of anemia associated with iron deficiency in low, medium, and high human development index countries: a systematic analysis of national surveys. Nutrients. https://doi.org/10.3390/nu8110693
Shaw JG (2011) Friedman JF Iron deficiency anemia: focus on infectious diseases in lesser developed countries. Anemia 260380:1–10
Leenstra T, Acosta LP, Langdon GC, Manalo DL, Su L, Olveda RM, McGarvey ST, Kurtis JD, Friedman JF (2006) Schistosomiasis japonica, anemia, and iron status in children, adolescents, and young adults in Leyte. Philippines Am J Clin Nutr 83(2):371–379
Leenstra T, Coutinho HM, Acosta LP, Langdon GC, Su L, Olveda RM, McGarvey ST, Kurtis JD, Friedman JF (2006) Schistosoma japonicum reinfection after praziquantel treatment causes anemia associated with inflammation. Infect Immun 74(11):6398–6407. https://doi.org/10.1128/IAI.00757-06
van den Broek NR, Letsky EA (2000) Etiology of anemia in pregnancy in south Malawi. Am J Clin Nutr 72(1 Suppl):247S-256S
Bourassa MW, Osendarp SJM, Adu-Afarwuah S, Ahmed S, Ajello C, Bergeron G, Black R, Christian P, Cousens S, de Pee S, Dewey KG, Arifeen SE, Engle-Stone R, Fleet A, Gernand AD, Hoddinott J, Klemm R, Kraemer K, Kupka R, McLean E, Moore SE, Neufeld LM, Persson L-Å, Rasmussen KM, Shankar AH, Smith E, Sudfeld CR, Udomkesmalee E, Vosti SA (2019) Review of the evidence regarding the use of antenatal multiple micronutrient supplementation in low- and middle-income countries. Ann N Y Acad Sci 1444(1):6–21. https://doi.org/10.1111/nyas.14121
Noor RA, Abioye AI, Ulenga N, Msham S, Kaishozi G, Gunaratna NS, Mwiru R, Smith E, Dhillon CN, Spiegelman D (2017) Large–scale wheat flour folic acid fortification program increases plasma folate levels among women of reproductive age in urban Tanzania. PLoS ONE 12(8):e0182099
Allen LH (2000) Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr 71(5):1280S-1284S. https://doi.org/10.1093/ajcn/71.5.1280s
Abioye AI, McDonald EA, Park S, Ripp K, Bennett B, Wu HW, Pond-Tor S, Sagliba MJ, Amoylen AJ, Baltazar PI, Tallo V (2019) Maternal anemia type during pregnancy is associated with anemia risk among offspring during infancy. Pediatr Res 86(3):396–402
Abioye AI, Park S, Ripp K, McDonald EA, Kurtis JD, Wu H, Pond-Tor S, Sharma S, Ernerudh J, Baltazar P, Acosta LP (2018) Anemia of inflammation during human pregnancy does not affect newborn iron endowment. J Nutrition 148(3):427–436
Nemeth E, Rivera S, Gabayan V, Keller C, Taudorf S, Pedersen BK, Ganz T (2004) IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Investig 113(9):1271–1276
PrabhuDas M, Bonney E, Caron K, Dey S, Erlebacher A, Fazleabas A, Fisher S, Golos T, Matzuk M, McCune JM, Mor G, Schulz L, Soares M, Spencer T, Strominger J, Way SS, Yoshinaga K (2015) Immune mechanisms at the maternal-fetal interface: perspectives and challenges. Nat Immunol 16(4):328–334. https://doi.org/10.1038/ni.3131
Ganz T, Nemeth E (2009) Iron sequestration and anemia of inflammation. Semin Hematol 46(4):387–393. https://doi.org/10.1053/j.seminhematol.2009.06.001
Weiss G, Ganz T, Goodnough LT (2019) Anemia of inflammation. Blood 133(1):40–50
Liu C, Luo D, Wang Q, Ma Y, Ping L, Wu T, Tang J, Peng D (2020) Serum homocysteine and folate concentrations in early pregnancy and subsequent events of adverse pregnancy outcome: the Sichuan Homocysteine study. BMC Pregnancy Childbirth 20(1):1–13
Etheredge AJ, Premji Z, Gunaratna NS, Abioye AI, Aboud S, Duggan C, Mongi R, Meloney L, Speigleman D, Roberts D, Hamer DH, Fawzi WW (2015) Iron supplementation among iron-replete and non-anemic pregnant women: a randomized placebo-controlled trial in Tanzania. JAMA Pediatr 169(10):947–955
Mwakyusa DH, Mukama W, MOHSW-Tanzania (2008) The national road map strategic plan to accelerate reduction of maternal, newborn and child deaths in Tanzania 2008–2015. Ministry of Health and Social Welfare, Tanzania, Dar es Salaam. http://advancefamilyplanning.org/sites/default/files/resources/RMNCH%20Plan%202014%20to%202015.pdf. Accessed 28 Oct 2022
Abioye AI, Aboud S, Premji Z, Etheredge AJ, Gunaratna NS, Sudfeld CR, Mongi R, Meloney L, Darling AM, Noor RA (2016) Iron supplementation affects hematologic biomarker concentrations and pregnancy outcomes among iron-deficient Tanzanian women–. J Nutr 146(6):1162–1171
World Health Organization (WHO) (2011) Haemoglobin concentration for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. WHO, Geneva. https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf. Accessed 28 Oct 2022
Namaste SM, Rohner F, Huang J, Bhushan NL, Flores-Ayala R, Kupka R, Mei Z, Rawat R, Williams AM, Raiten DJ (2017) Adjusting ferritin concentrations for inflammation: biomarkers reflecting inflammation and nutritional determinants of anemia (BRINDA) project. Am J Clin Nutr 106(1):359S-371S
World Health Organization (WHO) (2020) WHO Guideline: Use of ferritin concentrations to assess iron status in individuals and populations. https://www.who.int/docs/default-source/micronutrients/ferritin-guideline/ferritin-guidelines-brochure.pdf?sfvrsn=76a71b5a_4. Accessed June 3 2020
Weiss G, Goodnough LT (2005) Anemia of chronic disease. N Engl J Med 352(10):1011–1023. https://doi.org/10.1056/NEJMra041809
Skikne BS, Punnonen K, Caldron PH, Bennett MT, Rehu M, Gasior GH, Chamberlin JS, Sullivan LA, Bray KR, Southwick PC (2011) Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: a prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am J Hematol 86(11):923–927. https://doi.org/10.1002/ajh.22108
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Gravett MG, Purwar M, Frederick IO, Noble AJ, Pang R, Barros FC, Chumlea C, Bhutta ZA, Kennedy SH (2014) International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st Project. Lancet (Lond Engl) 384(9946):857–868. https://doi.org/10.1016/S0140-6736(14)60932-6
Spiegelman D, Hertzmark E (2005) Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol 162(3):199–200
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706
Hertzmark E, Spiegelman D (2010) The SAS ROBREG9 Macro.1–15
Hosmer DW Jr, Lemeshow S, Sturdivant RX (2013) Applied logistic regression, vol 398. John Wiley and Sons
Black AK, Allen LH, Pelto GH, de Mata MP, Chávez A (1994) Iron, vitamin B-12 and folate status in Mexico: associated factors in men and women and during pregnancy and lactation. J Nutr 124(8):1179–1188
Cade JE, Moreton JA, O’Hara B, Greenwood DC, Moor J, Burley VJ, Kukalizch K, Bishop DT, Worwood M (2005) Diet and genetic factors associated with iron status in middle-aged women. Am J Clin Nutr 82(4):813–820
Spiegler J, Stichtenoth G, Weichert J, Konig IR, Schlaud M, VDW A, Olbertz D, Gurth H, Schiffmann JH, Bohnhorst B, Gortner L, Herting E, Gopel W (2013) Pregnancy risk factors for very premature delivery: what role do hypertension, obesity and diabetes play? Arch Gynecol Obstet 288(1):57–64. https://doi.org/10.1007/s00404-013-2739-6
McGregor JA, French JI, Richter R, Franco-Buff A, Johnson A, Hillier S, Judson FN, Todd JK (1990) Antenatal microbiologic and maternal risk factors associated with prematurity. Am J Obstet Gynecol 163(5 Pt 1):1465–1473
Cheong JL, Doyle LW (2012) Increasing rates of prematurity and epidemiology of late preterm birth. J Paediatr Child Health 48(9):784–788. https://doi.org/10.1111/j.1440-1754.2012.02536.x
Melku M, Addis Z, Alem M (2014) Enawgaw B (2014) Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: an institutional based cross-sectional study. Anemia 108593:9. https://doi.org/10.1155/2014/108593
Ou Z, Li Q, Liu W, Sun X (2011) Elevated hemoglobin A2 as a marker for BETA.-Thalassemia trait in pregnant women. Tohoku J Exp Med 223(3):223–226
RStudio Team (2015) RStudio: integrated development for R. RStudio, Inc, Boston, MA URL rstudio com 42:14
Wirth JP, Woodruff BA, Engle-Stone R, Namaste SM, Temple VJ, Petry N, Macdonald B, Suchdev PS, Rohner F, Aaron GJ (2017) Predictors of anemia in women of reproductive age: biomarkers reflecting inflammation and nutritional determinants of anemia (BRINDA) project. Am J Clin Nutr 106(Suppl 1):416s–427s. https://doi.org/10.3945/ajcn.116.143073
Nemeth E, Ganz T (2014) Anemia of inflammation. Hematol Oncol Clin North Am 28(4):671–681
Smith LE, Prendergast AJ, Turner PC, Humphrey JH, Stoltzfus RJ (2017) Aflatoxin exposure during pregnancy, maternal anemia, and adverse birth outcomes. Am J Trop Med Hyg 96(4):770–776
Lynch S, Pfeiffer CM, Georgieff MK, Brittenham G, Fairweather-Tait S, Hurrell RF, McArdle HJ, Raiten DJ (2018) Biomarkers of nutrition for development (BOND)-iron review. J Nutr. https://doi.org/10.1093/jn/nxx036
Sangkhae V, Fisher AL, Chua KJ, Ruchala P, Ganz T, Nemeth E (2020) Maternal hepcidin determines embryo iron homeostasis in mice. Blood 136(19):2206–2216
McDonald EA, Gundogan F, Olveda RM, Bartnikas TB, Kurtis JD, Friedman JF (2022) Iron transport across the human placenta is regulated by hepcidin. Pediatr Res 92(2):396–402
Gambling L, Czopek A, Andersen HS, Holtrop G, Srai SK, Krejpcio Z, McArdle HJ (2009) Fetal iron status regulates maternal iron metabolism during pregnancy in the rat. Am J Physiol Regul Integr Comp Physiol 296(4):R1063-1070. https://doi.org/10.1152/ajpregu.90793.2008
Moormann AM, Sullivan AD, Rochford RA, Chensue SW, Bock PJ, Nyirenda T, Meshnick SR (1999) Malaria and pregnancy: placental cytokine expression and its relationship to intrauterine growth retardation. J Infect Dis 180(6):1987–1993
Abioye AI, McDonald EA, Park S, Joshi A, Kurtis JD, Wu H, Pond-Tor S, Sharma S, Ernerudh J, Baltazar P (2019) Maternal, placental and cord blood cytokines and the risk of adverse birth outcomes among pregnant women infected with Schistosoma japonicum in the Philippines. PLoS Negl Trop Dis 13(6):e0007371
Boga C, Ozdogu H (2016) Pregnancy and sickle cell disease: a review of the current literature. Crit Rev Oncol Hematol 98:364–374
Green R, Allen LH, Bjørke-Monsen A-L, Brito A, Guéant J-L, Miller JW, Molloy AM, Nexo E, Stabler S, Toh B-H (2017) Vitamin B 12 deficiency. Nat Rev Dis Primers 3(1):1–20
Ganz T (2019) Anemia of inflammation. N Engl J Med 381(12):1148–1157
Mwangi MN, Prentice AM, Verhoef H (2017) Safety and benefits of antenatal oral iron supplementation in low-income countries: a review. Br J Haematol 177(6):884–895. https://doi.org/10.1111/bjh.14584
McArdle HJ, Gambling L, Kennedy C (2014) Iron deficiency during pregnancy: the consequences for placental function and fetal outcome. Proc Nutr Soc 73(1):9–15. https://doi.org/10.1017/s0029665113003637
Oxman AD, Guyatt GH (1992) A consumer’s guide to subgroup analyses. Ann Intern Med 116(1):78–84
Sun X, Briel M, Walter SD, Guyatt GH (2010) Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ 30:340
Verhoef H, Veenemans J, Mwangi MN, Prentice AM (2017) Safety and benefits of interventions to increase folate status in malaria-endemic areas. Br J Haematol 177(6):905–918. https://doi.org/10.1111/bjh.14618
Funding
This study was supported by a grant from the National Institute of Child Health and Human Development (NICHD U01 HD061232).CD was supported in part by K24DK104676 and 2P30 DK040561. The NIH did not have any role in the design of the study, data collection, data analysis, data interpretation, or writing of this report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
394_2022_3029_MOESM1_ESM.docx
Supplementary file1 Supplement 1. Anemia type with maternal and newborn outcomes among HIV-negative pregnant women in both arms of a recent randomized trial Dar es Salaam, Tanzania, 2010–2013 (N=1,479). Supplement 2. Association of anemia type and adverse maternal and newborn outcomes among HIV-negative women with singleton pregnancies in the placebo arm of a recent randomized trial in Dar es Salaam, Tanzania, 2010–2013. Supplement 3. Flow chart for the differential diagnosis of iron deficiency anemia and anemia of inflammation—using sTfR. Supplement 4. Association of anemia type and adverse maternal and newborn outcomes among HIV-negative pregnant women in the placebo arm of a recent randomized trial in Dar es Salaam, Tanzania, 2010–2013. Supplement 5. Effect modification of the effectiveness of iron supplementation on the risk of adverse maternal and child outcomes by anemia type among HIV-negative pregnant women in Dar es Salaam, Tanzania, 2010–2013 (DOCX 90 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abioye, A.I., Hughes, M.D., Sudfeld, C.R. et al. The effect of iron supplementation on maternal iron deficiency anemia does not differ by baseline anemia type among Tanzanian pregnant women without severe iron deficiency anemia. Eur J Nutr 62, 987–1001 (2023). https://doi.org/10.1007/s00394-022-03029-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-03029-0