Abstract
Purpose
Food insecurity and multimoribidity (i.e., ≥ 2 chronic conditions) may be linked bidirectionally, but there are no studies on this topic from LMICs. Therefore, the aim of the present study was to examine the association between food insecurity and physical multimorbidity in a large representative sample of older adults from six LMICs.
Methods
Cross-sectional, community-based data on adults aged ≥ 50 years from the World Health Organization’s Study on Global AGEing and Adult Health (SAGE) conducted in China, Ghana, India, Mexico, Russia, and South Africa were analyzed. A total of 11 chronic physical conditions were assessed. Past 12 month food insecurity was assessed with two questions on frequency of eating less and hunger due to lack of food. Multivariable logistic regression analysis was conducted to assess the associations.
Results
Data on 34,129 adults aged ≥ 50 years [mean (SD) age 62.4 (16.0) years; age range 50–114 years; 47.9% males] were analyzed. After adjustment for potential confounders, in the overall sample, compared to being food secure, moderate and severe food insecurity were associated with 1.29 (95% CI 1.06–1.56) and 1.56 (95% CI 1.13–2.16) times higher odds for multimorbidity, respectively
Conclusion
Food insecurity was associated with greater odds for multimorbidity in older adults from LMICs. Addressing food insecurity in the general population may reduce risk for multimorbidity, while screening for food insecurity and addressing it among those with multimorbidity may lead to better clinical outcomes, pending future longitudinal research
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multimorbidity is often defined as “the coexistence of two or more chronic diseases” in the same individual [1]. Multimorbidity is a growing global public health challenge, as populations age and the prevalence of long-term conditions rise [2, 3]. This is of concern as multimorbidity is associated with poorer health outcomes (e.g., functional limitations, falls, premature mortality) and increased use of health and social care services with associated costs [4,5,6,7,8]. Such burden may be most pronounced in low- and middle-income countries (LMICs) where 80% of chronic diseases occur [9], and where the health and social care systems are under resourced, and perform poorly in comparison to high-income countries (HICs) [10]. It is thus important to identify correlates of multimorbidity in LMICs to inform targeted interventions.
One potential correlate of multimorbidity that has been little studied to date is food insecurity. Food insecurity may be defined as the disruption of food intake or eating patterns due to lack of money and other resources [11], and is most pronounced in LMICs [12,13,14]. Malnutrition, as a result of food insecurity, is strongly associated with vitamin deficiency, and in turn, this is associated with multiple chronic diseases such as osteoporosis, osteomalacia, and cardiovascular disease [15, 16]. Furthermore, when food becomes scarce, people tend to shift to more affordable but less nutritious food (e.g., high fat and carbohydrates), and this can also lead to an increased risk for cardiovascular diseases, for example [17]. Finally, it is also possible that multimorbidity leads to an increased risk for food insecurity, possibly due to financial burden as a consequence of suffering from multiple conditions [18, 19]. This implies a vicious cycle where people experiencing food insecurity may be at increased risk of multimorbidity due to poor nutrition, and multimorbidity may further exacerbate food insecurity via impoverishment. This vicious cycle may be particularly pronounced in many LMICs where universal health coverage is scarce, and where out-of-pocket expenditure and even catastrophic health expenditure are common.
However, to date, there is a scarcity of research on the association between food insecurity and multimorbidity. In one cross-sectional study of 2048 US older adults, compared to those without multimorbidity (i.e., 0–1 chronic conditions), food insecurity was positively associated with multiple chronic conditions (RRR 1.60, 95% CI 1.08–2.36, for 2–3 conditions; RRR 2.59, 95% CI 1.55–4.33 for 4–10 chronic conditions) [20]. Another cross-sectional study found that food insecurity was associated with greater than three times higher odds of multimorbidity in a sample of older US women (n = 279) receiving home-delivered meals [21]. Two other cross-sectional studies from the US and the US and Canada found that those with multimorbidity are at an increased risk of food insecurity [18, 19]. Specifically, in the study carried out in the US (n = 3552), compared to those with 0–1 conditions, respondents with multiple chronic conditions were significantly more likely to report food insecurity, with the adjusted odds ratio (OR) for those with 2–4 conditions being 2.12 (95% CI 1.45–3.09) and for those with five or more conditions being 3.64 (95% CI 2.47–5.37) [18]. In the study carried out in the US and Canada (n = 77,053), compared with adults with no chronic conditions, the odds for household food insecurity were 1.43 (95% CI 1.28–1.59), 1.86 (95% CI 1.62–2.14), and 3.44 (95% CI 3.02–3.93) times higher among adults with 1, 2, and 3 or more chronic conditions, respectively. To date, to the best of our knowledge, no other study exists on this topic.
The existing literature has some clear limitations. First, all studies were carried out in HICs (US and Canada), and the magnitude of this association in LMICs, where the prevalence of food insecurity is high, and where health services can be fragmented, under resourced and underperform, is not known [10]. Furthermore, disease profiles in LMICs are often different from those of high-income countries, and thus, findings from HICs are unlikely to be generalizable to LMICs. Finally, all existing studies have focused on one or two HICs. Multi-country studies from a variety of settings are important as they allow for the comparison of standardized estimates across settings. Given this background, the aim of the present study was to examine the cross-sectional association between food insecurity and physical multimorbidity in a sample of 34,129 adults aged ≥ 50 years from six LMICs spanning multiple continents. We hypothesized that food insecurity will be associated with higher odds for physical multimorbidity in LMICs.
Methods
Data from the Study on Global Ageing and Adult Health (SAGE) were analyzed. These data are publically available through https://apps.who.int/healthinfo/systems/surveydata/index.php/catalog/sage/about
This survey was undertaken in China, Ghana, India, Mexico, Russia, and South Africa between 2007 and 2010. Based on the World Bank classification at the time of the survey, Ghana was the only low-income country, and China and India were lower middle-income countries although China became an upper middle-income country in 2010. The remaining countries were upper middle-income countries. Details of the survey methodology have been published elsewhere [22]. Briefly, in order to obtain nationally representative samples, a multistage clustered sampling design method was used. The sample consisted of adults aged ≥ 18 years with oversampling of those aged ≥ 50 years. Trained interviewers conducted face-to-face interviews using a standard questionnaire. Standard translation procedures were undertaken to ensure comparability between countries. Half of the interviews in China were completed using a computer-assisted personal interview (CAPI) and the other half used paper and pencil. Mexico used CAPI and the other four countries used paper and pencil format for all interviews. The survey response rates were: China 93%; Ghana 81%; India 68%; Mexico 53%; Russia 83%; and South Africa 75%. Sampling weights were constructed to adjust for the population structure as reported by the United Nations Statistical Division. Ethical approval was obtained from the WHO Ethical Review Committee and local ethics research review boards (ethical approval numbers not available). Written informed consent was obtained from all participants.
Chronic physical conditions and physical multimorbidity
We included all 11 chronic physical conditions for which data were available in the SAGE. Chronic back pain was defined as having had back pain everyday during the last 30 days. Respondents who answered affirmatively to the question “Have you lost all of your natural teeth?” were considered to have edentulism. The participant was considered to have hearing problems if the interviewer observed this condition during the survey. Hypertension was defined as having at least one of the following: systolic blood pressure ≥ 140 mmHg; diastolic blood pressure ≥ 90 mmHg; or self-reported diagnosis. Visual impairment was defined as having severe/extreme difficulty in seeing and recognizing a person that the participant knows across the road [23]. Diabetes and stroke were solely based on lifetime self-reported diagnosis. For other conditions, the participant was considered to have the condition in the presence of either one of the following: self-reported diagnosis; or symptom-based diagnosis based on algorithms. We used these algorithms, which have been used in previous studies using the same dataset, to detect undiagnosed cases [24, 25]. Specifically, the validated Rose questionnaire was used for angina [26], and other previously validated symptom-based algorithms were used for arthritis, asthma, and chronic lung disease [24]. Further details on the definition of chronic physical conditions can be found in Table S1 (Appendix). The total number of chronic physical conditions was calculated and multimorbidity was defined as ≥ 2 chronic physical conditions, in line with previously used definitions [25].
Food insecurity
Food insecurity was defined by the two following questions: “In the last 12 months, how often did you ever eat less than you felt you should because there wasn’t enough food?” and “In the last 12 months, were you ever hungry, but didn’t eat because you couldn’t afford enough food?” Both of these questions had as response options: every month (coded = 1); almost every month (coded = 2); some months, but not every month (coded = 3); only in one or 2 months (coded = 4); never (coded = 5). These items were based on similar items found in food security questionnaires such as the US Household Food Security Survey Module and National Health and Nutrition Examination Survey (NHANES) Food Security module. As in a previous SAGE study, those who answered one through three to both questions or answered one to either item were categorized as severely food insecure. Those who did not fulfill the criteria for severe food insecurity but answered two through four for either question were coded as moderately food insecure. Those who answered five to both items were categorized as food secure [27]. We also used the dichotomous variable of any food insecurity (i.e., moderate/severe or none) in some analyses.
Control variables
The selection of control variables was based on previous literature [28] and included age, sex, highest level of education achieved (≤ primary, secondary, tertiary), and wealth quintiles based on income.
Statistical analysis
The statistical analysis was done with Stata 14.2 (Stata Corp LP, College station, Texas). The analysis was restricted to those aged ≥ 50 years. Tetrachoric correlations were assessed between each pair of chronic conditions among those with any food insecurity (N = 5444). Using the overall sample, multivariable logistic regression analyses were conducted to assess the association of food insecurity level (i.e., food secure, moderate, severe) or any food insecurity (exposure variables) with individual chronic conditions or multimorbidity (i.e., ≥ 2 chronic conditions) as the outcomes. The analysis on food insecurity and multimorbidity was also stratified by country. All regression analyses were adjusted for age, sex, education, wealth, and country, with the exception of the country-wise analysis which was not adjusted for country. Adjustment for country was done by including dummy variables for each country in the model as in previous SAGE publications. The sample weighting and the complex study design were taken into account in all analyses. Results from the regression analyses are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The level of statistical significance was set at P < 0.05.
Results
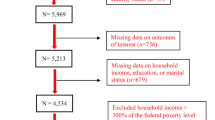
The final sample consisted of 34,129 adults aged ≥ 50 years [mean (SD) age 62.4 (16.0) years; age range 50–114 years; 47.9% males]. The sample characteristics are provided in Table 1. Overall, the prevalence of multimorbidity was 45.5%, while 6.7 and 5.1% had moderate and severe food insecurity, respectively. The most common chronic condition was hypertension (55.0%), followed by arthritis (29.5%), and angina (17.6%). The strongest pairwise correlations among those with any food insecurity was observed for chronic lung disease and angina or asthma (Table 2). Overall, the prevalence of multimorbidity increased with increasing severity of food insecurity (Fig. 1). However, not all countries showed similar trends. For example, increasing trends were not shown in Ghana and Mexico. After adjustment for potential confounders, any food insecurity was significantly associated with higher odds for arthritis, asthma, chronic lung disease, hearing problems, and visual impairment (Table 3). Compared to moderate food insecurity, severe food insecurity was more strongly associated with all these conditions. In the overall sample, compared to being food secure, moderate and severe food insecurity were associated with 1.29 (95% CI 1.06–1.56) and 1.56 (95% CI 1.13–2.16) times higher odds for multimorbidity, respectively (Table 4). Any food insecurity was significantly associated with multimorbidity in China, India, Russia, and South Africa but not in Ghana and Mexico.
Discussion
Main findings
In this large nationally representative sample of 34,129 adults aged ≥ 50 years, we found that compared to being food secure, moderate and severe food insecurity were associated with 1.29 (95% CI 1.06–1.56) and 1.56 (95% CI 1.13–2.16) times higher odds for multimorbidity, respectively. In terms of individual chronic conditions, any food insecurity was significantly associated with higher odds for arthritis, asthma, chronic lung disease, hearing problems, and visual impairment. However, country-wise analysis showed that food insecurity may not be associated with multimorbidity in all settings. Specifically, no significant associations were found in Mexico and Ghana.
Interpretation of the findings
The findings of our study are broadly in line with previous studies on this topic from HICs, which have found a positive association between food insecurity and multimorbidity [20, 21]. There are several plausible pathways that likely explain the relationship between food insecurity and multimorbidity. First, food insecurity is associated with vitamin and mineral deficiency, and this may lead to the development of multiple chronic conditions via several biophysiological mechanisms (e.g., increased levels of inflammation) [29, 30].
It is also important to note that vitamin deficiency exacerbates chronic diseases [30], potentially leading to greater severity and an increased likelihood of diagnosis. For example, in the case of asthma, an unhealthy diet resulting from household food insecurity may influence systemic inflammation that contributes to asthma. Moreover, low levels of fruit and vegetable consumption, and the resultant reduction in antioxidants might reduce airway inflammation [31]. Second, food insecurity increases levels of chronic stress, and stress can increase visceral fat accumulation and risk for chronic diseases. Specifically, under severe stress conditions, both the hypothalamus–pituitary–adrenal axis and reward pathways can contribute to the release of cortisol, neuropeptide Y, and other substances, causing a desire to consume high energy-dense foods, and altered metabolism [32]. In turn, this may increase risk for chronic diseases, in particular, cardiovascular diseases. Apart from these biological mechanisms, this shift to poor diets in food insecurity can also be related with financial reasons (i.e., low-cost high energy foods) [33] and may increase risk for overconsumption of energy and resultant obesity, which is a risk factor of a variety of non-communicable diseases [33]. Furthermore, food insecurity may exacerbate existing health conditions for older adults due to financial challenges in decisions between purchasing food versus medication that can subsequently lead to poorer disease management, greater subsequent health care needs, and worse overall health [34].
On the other hand, it is also possible that having chronic health conditions can remove one from the labor market, and without stable income, this may result in food insecurity. Further, having multiple chronic health conditions may also be expensive (e.g., treatments, medications, caretakers) especially without reliable health insurance, causing an economic burden on individuals and families, which includes food insecurity. Finally, multimorbidity when accompanied by disability can limit self-efficacy, social interactions, and social functioning, and this may increase risk for food insecurity [35]. Therefore, it is likely that the relationship between food insecurity and multimorbidity is bi-directional.
In our study, significant associations between food insecurity and multimorbidity was not found in Mexico and Ghana, suggesting that this association may be context specific. Although the reasons for the non-significance in these two countries can only be speculated, this may be due to difference in quality of health care, universal health coverage, availability of low-cost high energy food, or multimorbidity patterns [25] that may differ between countries. For example, Mexico had a high prevalence of diabetes and edentulism, which were not associated with food insecurity. Alternatively, it is possible for people with multimorbidity to be more health conscious following the advice of doctors, and this may lead to an increased effort to avoid food insecurity in people with multimorbidity in some settings. However, clearly, further studies are necessary on this issue to clarify why food insecurity is not associated with multimorbidity in some settings.
Public health implications
Findings from the present study suggest that addressing food insecurity in LMICs may lead to reduction in multimorbidity, or that among those with multimorbidity, addressing food insecurity may be important to improve clinical outcomes. Foodbanks have been found to provide immediate solutions to severe food deprivation and have the potential to improve food security outcomes in HICs [36]. In LMICs, such as African countries, the food bank model is still developing [37]. It may be prudent for governments and aid organizations to focus time and resource on developing the food bank model in LMICs to address food insecurity, which may have the additional benefit of reducing multimorbidity at a population level. Screening for food insecurity and addressing it among patients with multimorbidity in the clinical scene may also be an effective targeted strategy that may also improve clinical outcomes in these patients. For example, treatment may become incomplete in people who are food insecure for giving financial priority to food acquisition than treatment.
Strengths and limitations
The large sample size consisting of multiple nationally representative surveys from LMICs, where no data on food insecurity and multimorbidity exist, are clear strengths of the study. Furthermore, our results are important given the current COVID-19 pandemic, where food insecurity is increasing particularly among low-income adults, and treatment for chronic diseases has become suboptimal in many LMICs [38]. However, our findings must be interpreted in light of several limitations. First, the study was cross-sectional in nature and thus, temporal associations could not be established although in the context of food insecurity and multimorbidity, the association is likely to be bidirectional. Second, most data were self-reported potentially introducing social desirability and recall bias into the findings. Third, our measure of food insecurity was based on two questions and did not constitute a comprehensive food insecurity measure. Finally, our list of chronic diseases included a variety of diseases which are highly prevalent in LMICs, but lacked some diseases, such as cancer which is associated with particularly high costs to treat. Thus, it is possible for the results to have changed with a different set of chronic conditions.
Conclusion
In conclusion, food insecurity was significantly associated with higher odds for multimorbidity in our study on older adults from LMICs, although significant associations were not found in all countries. Future longitudinal studies that assess the temporal association, and experimental studies that examine the underlying mechanisms, as well as qualitative studies to identify the reasons for the between-country heterogeneity are warranted to inform targeted interventions.
Change history
11 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00394-022-03082-9
References
Diederichs C, Berger K, Bartels DB (2011) The measurement of multiple chronic diseases—a systematic review on existing multimorbidity indices biomedical sciences and medical sciences. J Gerontol Ser A. https://doi.org/10.1093/gerona/glq208
Uijen AA, van de Lisdonk EH (2008) Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. https://doi.org/10.1080/13814780802436093
Fortin M, Stewart M, Poitras M, Almirall J, Maddocks H (2012) A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. https://doi.org/10.1370/afm.1337
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B (2012) Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. https://doi.org/10.1016/S0140-6736(12)60240-2
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Meinow B, Fratiglioni L (2011) Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. https://doi.org/10.1016/j.arr.2011.03.003
Zhao YW, Haregu TN, He L, Lu S, Katar A, Wang H, Yao Z, Zhang L (2021) The effect of multimorbidity on functional limitations and depression amongst middle-aged and older population in China: a nationwide longitudinal study. Age Ageing. https://doi.org/10.1093/ageing/afaa117
Afrin N, Honkanen R, Koivumaa-Honkanen H, Lukkala P, Rikkonen T, Sirola J, Williams LJ, Kröger H (2016) Multimorbidity predicts falls differentially according to the type of fall in postmenopausal women. Matur. https://doi.org/10.1016/j.maturitas.2016.05.004
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA (2016) Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. https://doi.org/10.1016/j.archger.2016.07.008
World Health Organization (2005) Chronic diseases in low and middle income countries. In: https://www.who.int/chp/chronic_disease_report/media/Factsheet3.pdf. Accessed 18 Sep 2022.
Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, Schwarz D, Hirschhorn LR (2019) Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. https://doi.org/10.1136/bmjgh-2019-001551
Nord M, Andrews M, Carlson S (2006) Household Food Security in the United States, 2005. United States Department of Agriculture; USDA, Washington, D.C.
World Health Organization (2019) The state of food security and nutrition in the world 2019: safeguarding against economic slowdowns and downturns. Food Agriculture Org.
Fares K, Barada D, Hoteit M, Abou Haidar M (2020) Prevalence and correlates of food insecurity among Lebanese University students of Hadath Campus. Atena J Public Health. https://www.atenajournals.com/ajph/article/view/22
El Haddad RF, Yahfoufi N, Abou Haidar M, Hoteit M (2020) Knowledge, Attitude and Practices of Lebanese Married Women towards Food Safety. Atena J Public Health. https://atenajournals.com/ajph/article/view/7
Judd SE, Tangpricha V (2009) Vitamin D deficiency and risk for cardiovascular disease. Am J Med Sci. https://doi.org/10.1097/MAJ.0b013e3181aaee91
Woteki CE, Thomas PR (1993) Eat for Life. The Food and Nutrition Board’s Guide to Reducing Your Risk of Chronic Disease. Clin Nutr Insight. https://doi.org/10.17226/1365
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee I, Lichtenstein AH, Loria CM, Millen BE (2014) 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. https://doi.org/10.1161/01.cir.0000437740.48606.d1
Jih J, Stijacic-Cenzer I, Seligman HK, Boscardin WJ, Nguyen TT, Ritchie CS (2018) Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. https://doi.org/10.1017/S1368980017004062
Tarasuk V, Mitchell A, McLaren L, McIntyre L (2013) Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr. https://doi.org/10.3945/jn.113.178483
Leung CW, Kullgren JT, Malani PN, Singer DC, Kirch M, Solway E, Wolfson JA (2020) Food insecurity is associated with multiple chronic conditions and physical health status among older US adults. Prev Med Rep. https://doi.org/10.1016/j.pmedr.2020.101211
Sharkey JR (2003) Risk and presence of food insufficiency are associated with low nutrient intakes and multimorbidity among homebound older women who receive home-delivered meals. J Nutr. https://doi.org/10.1093/jn/133.11.3485
Kowal P, Chatterji S, Naidoo N, Biritwum R, Fan W, Lopez Ridaura R, Maximova T, Arokiasamy P, Phaswana-Mafuya N, Williams S (2012) Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidemiol. https://doi.org/10.1093/ije/dys210
Freeman EE, Roy-Gagnon M, Samson E, Haddad S, Aubin M, Vela C, Zunzunegui MV (2013) The global burden of visual difficulty in low, middle, and high income countries. PLoS ONE. https://doi.org/10.1093/jn/133.11.3485
Arokiasamy P, Kowal P, Capistrant BD, Gildner TE, Thiele E, Biritwum RB, Yawson AE, Mensah G, Maximova T, Wu F (2017) Chronic noncommunicable diseases in 6 low-and middle-income countries: findings from wave 1 of the world health organization’s study on global ageing and adult health (SAGE). Am J Epidemiol. https://doi.org/10.1093/aje/kww125
Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, Lara E, Koskinen S, Tobiasz-Adamczyk B, Ayuso-Mateos JL (2016) Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol Ser A. https://doi.org/10.1093/gerona/glv128
Rose GA (1962) The diagnosis of ischaemic heart pain and intermittent claudication in field surveys. Bull World Health Organ 27(6):45–62
Schrock JM, McClure HH, Snodgrass JJ, Liebert MA, Charlton KE, Arokiasamy P, Naidoo N, Kowal P (2017) Food insecurity partially mediates associations between social disadvantage and body composition among older adults in india: Results from the study on global AGE ing and adult health (SAGE). Am J Hum Biol. https://doi.org/10.1002/ajhb.23033
Seligman HK, Laraia BA, Kushel MB (2010) Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. https://doi.org/10.3945/jn.109.112573
Gowda C, Hadley C, Aiello AE (2012) The association between food insecurity and inflammation in the US adult population. Am J Public Health. https://doi.org/10.2105/AJPH.2011.300551
Tulchinsky TH (2010) Micronutrient deficiency conditions: global health issues. Public Health Rev. https://doi.org/10.1007/BF03391600
Park S, Park B, Jung D, Kwon Y (2019) Association between household food insecurity and asthma in korean adults. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16122115
Laraia BA (2013) Food insecurity and chronic disease. Adv Nutr. https://doi.org/10.3945/an.112.003277
Pan L, Sherry B, Njai R, Blanck HM (2012) Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. https://doi.org/10.1016/j.jand.2012.06.011
Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC (2013) Food insecurity and metabolic control among US adults with diabetes. Diabetes Care. https://doi.org/10.2337/dc13-0570
Heflin CM, Altman CE, Rodriguez LL (2019) Food insecurity and disability in the United States. Disabil health J 12(2):20–26
Bazerghi C, McKay FH, Dunn M (2016) The role of food banks in addressing food insecurity: a systematic review. J Community Health. https://doi.org/10.1007/s10900-015-0147-5
The Global FoodBanking Network (2020) Food banks are needed more than ever. In: https://www.foodbanking.org/stateofglobalfoodbanking/food-banking-today.html. Accessed 18 July 2022
Carducci B, Keats EC, Ruel M, Haddad L, Osendarp S, Bhutta ZA (2021) Food systems, diets and nutrition in the wake of COVID-19. Nat Food. https://doi.org/10.1038/s43016-021-00233-9
Acknowledgements
This paper uses data from WHO’s Study on Global Ageing and Adult Health (SAGE). SAGE is supported by the U.S. National Institute on Aging through Interagency Agreements OGHA 04034785, YA1323–08-CN-0020, Y1-AG-1005–01 and through research grants R01-AG034479 and R21-AG034263.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. Dr. Guillermo F. López Sánchez is funded by the European Union—Next Generation EU.
Author information
Authors and Affiliations
Contributions
LS, JIS, LJ, GFLS, FS, MAT, HO, NV, PS, LB, YB, AK are responsible for design, writing, and final content. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author have not disclosed any conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smith, L., Shin, J.I., Jacob, L. et al. Food insecurity and physical multimorbidity among adults aged ≥ 50 years from six low- and middle-income countries. Eur J Nutr 62, 489–497 (2023). https://doi.org/10.1007/s00394-022-02999-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02999-5