Abstract
Background
Increased fish consumption reduces the risk of dementia. However, it is unknown whether fish consumption reduced all-cause mortality in people with dementia. The purpose of the study is to investigate the association of fish consumption with all-cause mortality in older people with dementia versus those without dementia.
Methods
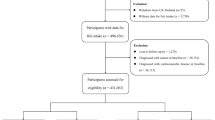
Using a standard method of the Geriatric Mental State, we interviewed 4165 participants aged ≥ 60 years who were randomly recruited from five provinces in China during 2007–2009 to collect the baseline data of socio-demography, disease risk factors, histories of disease, and details of dietary intakes, and diagnosed dementia (n = 406). They were followed up for vital status until 2012.
Results
The cohort follow-up documented 329 deaths; 61 were in participants with dementia (55.3 per 1000 person-years) and 224 were those without dementia (22.3). In all participants, the risk of all-cause mortality was reduced with fish intake at “ ≥ twice a week” (multivariate-adjusted hazard ratio 0.58, 95% CI 0.34–0.96) and at “once a week or less” (0.79, 0.53–1.18) compared to “never eat” over the past two years. In participants without baseline dementia, the corresponding HRs for all-cause mortality were 0.57 (0.33–0.98) and 0.85 (0.55–1.31), while in participants with dementia were 1.36 (0.28–6.60) and 1.05 (0.30–3.66), respectively.
Conclusion
This study reveals that consumption of fish in older age reduced all-cause mortality in older people without dementia, but not in people with dementia. Fish intake should be increased in older people in general, prior to the development of dementia in the hope of preventing dementia and prolonging life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Consumption of fish reduces incidence of cardiovascular disease (CVD) [1], respiratory diseases [2], cancers [3], diabetes [4, 5], and mental illness [6]. Our recent study also demonstrated that increased consumption of fish was associated with a reduced risk of dementia [7]. However, it is unknown whether fish intake reduced mortality in people with dementia, and improved survival in older population. Previous studies showed that increased consumption of fish reduced all-cause mortality [8, 9]. Almost all previous studies [8] were carried out in young and middle-aged populations. A few studies have examined the impact of fish intake in older age on all-cause mortality, while the dietary patterns between young-middle and older population are different (e.g., older people had reduced fish consumption [10, 11]). Furthermore, most studies examining the impact of fish intake on mortality were undertaken in high-income countries (HICs), and the findings may not be generalisable to those in low- and middle-income countries (LMICs), where socioeconomic deprivation, cardiovascular disease and risk factors (CVDRFs), social support, and health inequalities are different from those in HICs [12]. China is the largest LMIC with population ageing and has 241 million older people. There have been 15 million Chinese living with dementia [13, 14]. In this study, we examined the data of a community-based cohort study of older people living in China, to assess the impact of fish intake in older age on all-cause mortality in older people with and without dementia.
Methods
Study populations and baseline survey
The study population was derived from the Anhui province cohort (the third-wave health survey) and the four provinces' health survey study in China [15]. Their methods of the baseline survey and follow-up have been fully described in previous publications [15, 16].
Briefly, in the Anhui cohort study, we recruited a random sample of 1810 older people aged ≥ 65 years who had lived for at least 5 years in Yiming subdistrict of Hefei city in 2001, and 1709 older people aged ≥ 60 years from all 16 villages in Tangdian District of Yingshang County in 2003. Our trained survey team from the Anhui Medical University used the standard methods of the Geriatric Mental State (GMS) questionnaire [17] and a general health and risk factors record [12] to interview 3336 participants (1736 from the urban sample in 2001 and 1600 from the rural in 2003) for baseline data collection (wave 1). After completing the wave 2 interview involving 2608 participants in the year 2002 for the urban participants and in 2004 for the rural participant [18, 19], we carried out the third-wave survey during 2007–2009 and successfully re-interviewed 1757 participants, obtaining a response rate of 82.4% of surviving cohort members [15, 19]. In the wave 3 survey, apart from the GMS and the general health and risk factors record which was derived partly from the Minimum Data Set (MDS) of the Medical Research Council Ageing in Liverpool Project-Health Aspects (MRC-ALPHA) study [20, 21] and the Scottish MONICA surveys [22], we included other components of the 10/66 algorithm dementia research package [23] and dietary intake questionnaire [7, 15] for interview. Permission for interview and informed consent were obtained from each participant or, if that was not possible, from the closest responsible adult. We recorded details relating to socio-demography, lifestyles, social networks and support, CVDRFs, dietary intakes, and histories of chronic diseases for each participant. All participants were asked to state their dietary intake frequencies which included meat, fish, egg, fresh vegetables, fruits, over the past 2 years in a choice of (1) Never eat, (2) Once a week or less, (3) > Once a week and < daily, (4) Once a day, and (5) > Daily in a simple food frequency questionnaire [7]. According to standard procedures [22], we measured systolic and diastolic blood pressure, height, weight, and waist circumference in each participant. We performed a computer program-assisted diagnosis, the Automated Geriatric Examination for Computer Assisted Taxonomy (AGECAT) [17], to assess the information from the GMS to identify the principal mental disorders and diagnose depression and dementia in the participants [12, 18, 24].
The methods employed in the four-province study have been fully described before [16, 24]. In brief, in 2008–2009, following our wave 3 survey of the Anhui cohort study [7, 15], we chose one urban and one rural community from each of four provinces (Guangdong, Heilongjiang, Shanghai, and Shanxi) as the study fields and sought to recruit 500 or more participants from each community. We employed a cluster random sampling method to select residential communities from each of the four provinces. The target population consisted of residents aged ≥ 60 years who had lived in the area for at least 5 years. Based on the residency lists of the district and village committees, we recruited a total of 4314 participants, with an overall response rate of 93.8%. The protocol of the interview was the same as that in the Anhui cohort wave 3 survey described above.
Follow-up of the multi-province cohort
We took 6071 participants (4314 from the four-province study and 1757 from the Anhui wave 3 survey) as baseline cohort members, since their interview included the dietary intake questionnaire. In 2010–2012, we followed up the cohort to monitor their vital status and re-interviewed surviving participants using the same questionnaires as those at baseline [16, 19, 25]. The interview team of each province visited the local residential areas to obtain the survival status of each of the cohort members through the resident committees, village/district leaders, and local police stations. There were 329 deaths documented in the cohort. A standard verbal autopsy questionnaire was employed to further identify causes of death from family members, relatives, neighbours, or friends of the deceased. We successfully re-interviewed 3836 surviving participants [16, 19, 25]. The overall follow-up rate of the cohort was 68.6%. Ethical approval for the study was obtained from the Research Ethics Committee, Anhui Medical University, China, and the Research Ethics Committee, University of Wolverhampton, UK (Ref. A1- Favourable, granted in 2010).
Data analysis
Descriptive statistics were used to examine the characteristics of the participants. Distributions of sociodemographic and risk factors between surviving and deceased were assessed by a t-test for continuous variables and a Chi-square test for category variables. Cox proportional hazards regression models were employed to assess all-cause mortality in relation to consumption of fish over the past two years at baseline. According to this cohort data, we divided the participants into three groups based on their consumption of fish at baseline; (1) “Never eat”, (2) “A little” (including those of “Once a week or less”), and (3) “A lot” (including those of “ > Once a week and < daily”, “Daily” and “ > Daily”). We computed the hazard ratios (HR) and 95% confidence intervals of all-cause mortality at each group level of fish consumption. In the models, we adjusted for different sets of confounding co-variables, including age, sex, province, urban–rural living, educational level, occupational class, income, smoking status, alcohol consumption, body mass index (BMI), marital status, frequency of visiting children or other relatives, activity of daily living (ADL), hypertension, heart disease, diabetes, depression, dementia, and consumption of meat, vegetables, and fruits. Following the data analysis for all participants, we stratified data of participants with and without dementia at baseline for analysis and tested the differences in HRs between two groups of participants according to those we did in previous papers [19].
All data analyses were conducted using SPSS version 26 software (IBM Co., Armonk, NY, USA).
Results
Of 4165 participants, the mean age (SD) was 72.1 (7.3) years, 55.3% were women, 58.5% lived in rural areas, and 47.6% were illiterate. The details of the baseline characteristics of the study participants are shown in Table 1. Compared to those surviving, participants who died were older, male, smoking, underweight, less educated, widowed and living alone, and had unsatisfactory income, higher levels of children/other relatives visiting > once a week, higher ADL (i.e., more dependent), hypertension, and dementia. They consumed less fish over the past two years (Table 1). Other factors in Table 1 showed no significant differences between deaths and survivals.
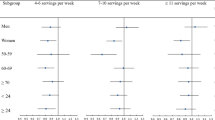
Table 2 shows numbers, mortality rates, and adjusted HRs among the three groups of participants with different levels of fish consumption. There were significant differences in mortality rate among these groups (p = 0.011): 34.4 per 1000 person-years in participants who “never eat” fish over the past two years, 28.4 in participants with “a little” fish intake and 20.8 in participants with “a lot” fish intake. Compared to those with “never eat” fish over the past two years, the age-sex adjusted HR of all-cause mortality in participants with “a little” fish consumption was 0.70 (95% CI 0.53–0.93) and in “a lot” 0.56 (0.42–0.74). After further adjustment for socioeconomic status, social support, lifestyles, and BMI, these HRs were slightly increased (Model 2 in Table 2). Adding co-morbidities, meat, vegetables, and fruits consumption for further adjustment (Model 3), the matched HRs were 0.79 (0.53–1.18) and 0.58 (0.34–0.96), respectively. In the model, there were no significant interaction effects of fish consumption with dementia on all-cause mortality.
The findings of a separate data analysis by baseline dementia can be seen in Tables 3 and 4. Table 3 shows numbers, mortality rates, and adjusted HRs among the three groups of non-demented participants with different levels of fish consumption; fully adjusted HR of all-cause mortality was 0.85 (0.55–1.31) in fish consumption of “a little” and 0.57 (0.33–0.98) at “a lot” compared to those that “never eat” over the past two years. Reduced HRs of mortality by increased consumption of fish in participants without dementia were similar to those in all participants (Table 2).
However, the data from 405 participants with dementia at baseline showed no association of fish intake with all-cause mortality (Table 4); age-sex HR was 0.94 (0.41–2.15) in those with consumption of fish at “a little” and 0.97 (0.45–2.09) at “a lot” compared to those “never eat”, while with more confounders adjusted for, the association between consumption of fish and all-cause mortality became positive, but not statistically significant, and the fully adjusted HR of all-cause mortality was 1.05 (0.30–3.66) in fish consumption of “a little” and 1.36 (0.28–6.60) at “a lot” compared to those that “never eat” over the past 2 years. There were no significant differences in the HRs between participants with and without dementia; ratio of HRs in the fish consumption of “a little” was 1.24 (95% CI 0.33–4.64), p = 0.754, and in “a lot” fish consumption 2.39 (0.45–12.69), p = 0.308.
Discussion
Our community-based cohort study from the five provinces of China revealed that older people with increased fish intake had reduced all-cause mortality. The association is independent of other factors. Stratifying data analysis for the dementia status showed that the impact of fish consumption on survival was more obvious in people who were free of dementia, and there was no association of fish consumption with all-cause mortality in people with dementia.
Previous studies examining the association between consumption of fish and reduced all-cause mortality were mostly undertaken in HICs and in young and middle age groups of populations [8]. Many [8, 9, 26], but not all [27, 28] showed an inverse relationship between fish consumption and all-cause mortality. In a US Chicago Western Electric Study of 1822 male participants aged 40 to 55 years with a follow-up period of 30 years, Daviglus et al. [29] found a non-significant reduction in the risk of all-cause mortality (RR 0.85, 0.64–1.10) when the highest fish consumption was compared with the lowest fish consumption. A non-significant inverse association of fish consumption with all-cause mortality was also found among 17,611 participants aged 32–46 years with 22 years follow-up period in a US National Health and Nutrition Examination Survey (NHANES III), when the highest fish consumption level was compared with the lowest consumption level (HR 0.93, 0.78–1.11) [30]. Other studies including mixed-age groups of population showed more significant association of fish intake with reduced all-cause mortality [31,32,33]. The US Southern Community Cohort Study (SCCS) followed up 77,604 participants aged 40–79 years for 5.5 years and showed a significant inverse association of total fish consumption with all-cause mortality (adjusted HR 0.92, 0.84–1.00 in the highest quintile of fish consumption versus the lowest quintile) [32]. In a US Vitamins and Lifestyle cohort Study (VITAL Study) of 70,495 participants aged 50–76 years with a follow-up period of 5 years, Bell et al. [31] found a significant reduction in the risk of all-cause mortality (HR 0.86, 0.76–0.98) when the highest fish consumption was compared with the lowest fish consumption. The discrepancies in the findings of the association between fish consumption and all-cause mortality among these studies conducted in HICs could be related to various characteristics within the study population (e.g., age, socioeconomic status), sample size, follow-up duration, confounding adjustment, and data analysis. Furthermore, few of them examined the consumption of fish in older age associated with all-cause mortality, particularly in LMICs. The data of our cohort study in China showed the inverse association between fish consumption in older age and all-cause mortality. The impact of fish intake on reduced all-cause mortality could be from the effects of readily available omega-3 Poly Unsaturated Fatty Acid (PUFA) constituents contained in fish on multiple chronic diseases (such as CVD [1, 34], diabetes [4, 5], respiratory diseases [2], mental illnesss [6], and dementia [7]), resulting from their anti-inflammatory [35], anti-atherosclerotic, antithrombotic [36], and antiarrhythmic and antiatherogenic properties [37, 38] These would help to prevent the development of those chronic diseases and then reduce mortality. The finding of the current study has contributed and filled the gaps in the literature.
On analysing the data of older people with and without dementia separately, we found that the impact of fish intake on reduced all-cause mortality was more obvious in people without dementia at baseline. This may support the pathway of the impact via preventing chronic diseases, including dementia [7]. However, in people with dementia, we have not observed such an inverse association between fish consumption and all-cause mortality, and in contrast found a non-significant association of fish consumption with increased mortality, which could be due to a possible reverse association between dementia severity (or more co-morbidities) and fish consumption or the potential adverse effects of fish intake (e.g., heavy metal contamination). This requires further exploration. As far as we know, no study has been done to examine the impact of fish consumption on all-cause mortality in people with dementia. Previously, a meta-analysis study [39] examined the impact of fish consumption on all-cause mortality among diabetic patients and found a reduced risk of all-cause mortality in the highest category of fish consumption versus the lowest (0.86, 0.76–0.96). A lack of an association between fish consumption and all-cause mortality in older people with dementia may reflect the nature of dementia, i.e., its prognosis would be deteriorating with no effective treatment and intervention. Our data suggest that future research should stratify data analysis according to co-morbidities, particularly dementia, to examine the impact of fish intake on all-cause mortality in populations.
Strengths and limitations of the study
The main contribution of this study is to identify the impact of increased consumption of fish on all-cause mortality in older people from LMICs, particularly including rural areas in China. To the best of our knowledge, it is the first study in the world to examine the association of fish consumption with all-cause mortality in people with dementia. Our study included many important confounders for adjustment and the findings would be robust. Our study has some limitations. First, in the baseline health survey, participants’ self-reported frequencies of dietary information on the consumption of fish were used for analysis. This may have caused a misclassification of the level of fish intake, which would make our findings of the association to tend towards the null hypothesis. Second, our cohort study did not collect baseline data for types of fish (e.g., lean, fatty-fish, and seafood), quantity of fish, and the omega-3 supplements consumed, like some other studies [40, 41]. Thus, we cannot infer which types and quantity of fish were associated with all-cause mortality. Future research is required to assess which types of fish intake in older age would be significantly associated with all-cause mortality in people with and without dementia. Third, due to the absence of the total energy intake in the data collection, we could not adjust for it and its residual effect could not be excluded from the association between fish consumption and all-cause mortality. However, we adjusted for the consumption of meat and vegetable/fruit and the residual effect would be minimised. Future research is needed to include the total energy intake for adjustment to confirm the association of fish consumption with all-cause mortality in older people and in people with dementia.
Conclusion
This study has demonstrated an inverse association of fish intake at older age with all-cause mortality in older people, but not in people with dementia. The findings suggest that it would be better to increase the consumption of fish in older people in general, prior to the development of dementia in the hope of preventing dementia and prolonging life.
References
Bechthold A, Boeing H, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, De Henauw S, Michels N, Devleesschauwer B, Schlesinger S (2019) Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr 59:1071–1090. https://doi.org/10.1080/10408398.2017.1392288
Yang H, Xun P, He K (2013) Fish and fish oil intake in relation to risk of asthma: a systematic review and meta-analysis. PLoS One 8:e80048. https://doi.org/10.1371/journal.pone.0080048
Dai Y, Bai Y, Zhang X (2017) Fish consumption and prostate cancer risk: a meta-analysis of 37 studies. Int J Clin Exp Med 10:9891–9900
Zheng JS, Huang T, Yang J, Fu YQ, Li D (2012) Marine N-3 polyunsaturated fatty acids are inversely associated with risk of type 2 diabetes in Asians: a systematic review and meta-analysis. PLoS One 7:e44525. https://doi.org/10.1371/journal.pone.0044525
Xun P, He K (2012) Fish consumption and incidence of diabetes: meta-analysis of data from 438,000 individuals in 12 independent prospective cohorts with an average 11-year follow-up. Diabetes Care 35:930–938. https://doi.org/10.2337/dc11-1869
Sanchez-Villegas A, Henríquez P, Figueiras A, Ortuño F, Lahortiga F, Martínez-González MA (2007) Long chain omega-3 fatty acids intake, fish consumption and mental disorders in the SUN cohort study. Eur J Nutr 46:337–346. https://doi.org/10.1007/s00394-007-0671-x
Bakre AT, Chen R, Khutan R, Wei L, Smith T, Qin G, Danat IM, Zhou W, Schofield P, Clifford A (2018) Association between fish consumption and risk of dementia: a new study from China and a systematic literature review and meta-analysis. Public Health Nutr 21:1921–1932. https://doi.org/10.1017/S136898001800037X
Wan Y, Zheng J, Wang F, Li D (2017) Fish, long chain omega-3 polyunsaturated fatty acids consumption, and risk of all-cause mortality: a systematic review and dose-response meta-analysis from 23 independent prospective cohort studies. Asia Pac J Clin Nutr 26:939–956. https://doi.org/10.6133/apjcn.072017.01
Zhao L, Sun J, Yang Y, Ma X, Wang Y, Xiang Y (2016) Fish consumption and all-cause mortality: a meta-analysis of cohort studies. Eur J Clin Nutr 70:155–161. https://doi.org/10.1038/ejcn.2015.72
Grieger JA, Miller M, Cobiac L (2012) Knowledge and barriers relating to fish consumption in older Australians. Appetite 59:456–463. https://doi.org/10.1016/j.appet.2012.06.009
Can MF, Günlü A, Can HY (2015) Fish consumption preferences and factors influencing it. Food Sci Technol 35:339–346. https://doi.org/10.1590/1678-457X.6624
Chen R, Wei L, Hu Z, Qin X, Copeland JR, Hemingway H (2005) Depression in older people in rural China. Arch Intern Med 165:2019–2025. https://doi.org/10.1001/archinte.165.17.2019
Chan KY, Wang W, Wu JJ, Liu L, Theodoratou E, Car J, Middleton L, Russ TC, Deary IJ, Campbell H (2013) Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet 381:2016–2023. https://doi.org/10.1016/S0140-6736(13)60221-4
Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, Li Y, Zhu M, Jiao H, Song Y (2020) Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health 5:e661–e671. https://doi.org/10.1016/S2468-2667(20)30185-7
Chen R, Wilson K, Chen Y, Zhang D, Qin X, He M, Hu Z, Ma Y, Copeland JR (2013) Association between environmental tobacco smoke exposure and dementia syndromes. Occup Environ Med 70:63–69. https://doi.org/10.1136/oemed-2012-100785
Chen R, Lang L, Clifford A, Chen Y, Hu Z, Han TS (2016) Demographic and socioeconomic influences on community-based care and caregivers of people with dementia in China. JRSM Cardiovasc Dis 5:2048004016652314. https://doi.org/10.1177/2048004016652314
Copeland JR, Prince M, Wilson K, Dewey M, Payne J, Gurland B (2002) The geriatric mental state examination in the 21st century. Int J Geriatr Psychiatry 17:729–732. https://doi.org/10.1002/gps.667
Chen R, Hu Z, Wei L, Ma Y, Liu Z, Copeland JR (2011) Incident dementia in a defined older Chinese population. PLoS One 6:e24817. https://doi.org/10.1371/journal.pone.0024817
Chen R, Hu Z, Wei L, Wilson K (2014) Socioeconomic status and survival among older adults with dementia and depression. Br J Psychiatry 204:436–440. https://doi.org/10.1192/bjp.bp.113.134734
Wilson K, Taylor S, Copeland J, Chen R, McCracken C (1999) Socio-economic deprivation and the prevalence and prediction of depression in older community residents. Br J Psychiatry 175:549–553. https://doi.org/10.1192/bjp.175.6.549
Chen R, Hu Z, Wei L, Qin X, McCracken C, Copeland JR (2008) Severity of depression and risk for subsequent dementia: cohort studies in China and the UK. Br J Psychiatry 193:373–377. https://doi.org/10.1192/bjp.bp.107.044974
Chen R, Tunstall-Pedoe H (2005) Socioeconomic deprivation and waist circumference in men and women: the Scottish MONICA surveys 1989–1995. Eur J Epidemiol 20:141–147. https://doi.org/10.1007/s10654-004-4498-y
Prince MJ, De Rodriguez JL, Noriega L, Lopez A, Acosta D, Albanese E, Arizaga R, Copeland JR, Dewey M, Ferri CP (2008) The 10/66 Dementia Research Group’s fully operationalised DSM-IV dementia computerized diagnostic algorithm, compared with the 10/66 dementia algorithm and a clinician diagnosis: a population validation study. BMC Public Health 8:219–231. https://doi.org/10.1186/1471-2458-8-219
Chen R, Ma Y, Wilson K, Hu Z, Sallah D, Wang J, Fan L, Chen R, Copeland JR (2012) A multicentre community-based study of dementia cases and subcases in older people in China-”the GMS-AGECAT prevalence and socio-economic correlates. Int J Geriatr Psychiatry 27:692–702. https://doi.org/10.1002/gps.2767
Zhou W, Chen R, Hopkins A, Wang Y, Tang J, Chen X, Clifford A, Pan Y, Forthby K, Ni J, Wang D, Brunner E (2020) Association between socioeconomic status and incident stroke in China. J Epidemiol Community Health 74(6):519–526. https://doi.org/10.1136/jech-2019-213515
Jayedi A, Shab-Bidar S, Eimeri S, Djafarian K (2018) Fish consumption and risk of all-cause and cardiovascular mortality: a dose-response meta-analysis of prospective observational studies. Public Health Nutr 21:1297–1306. https://doi.org/10.1017/S1368980017003834
Nakamura Y, Ueshima H, Okamura T, Kadowaki T, Hayakawa T, Kita Y, Tamaki S, Okayama A, NIPPON DATA80 Research Group (2005) Association between fish consumption and all-cause and cause-specific mortality in Japan: NIPPON DATA80, 1980–99. Am J Med 118:239–245. https://doi.org/10.1016/j.amjmed.2004.12.016
Osler M, Andreasen AH, Hoidrup S (2003) No inverse association between fish consumption and risk of death from all-causes, and incidence of coronary heart disease in middle-aged, Danish adults. J Clin Epidemiol 56:274–279. https://doi.org/10.1016/S0895-4356(02)00600-5
Daviglus ML, Stamler J, Orencia AJ, Dyer AR, Liu K, Greenland P, Walsh MK, Morris D, Shekelle RB (1997) Fish consumption and the 30-year risk of fatal myocardial infarction. N Engl J Med 336:1046–1053. https://doi.org/10.1056/NEJM199704103361502
Kappeler R, Eichholzer M, Rohrmann S (2013) Meat consumption and diet quality and mortality in NHANES III. Eur J Clin Nutr 67:598–606. https://doi.org/10.1038/ejcn.2013.59
Bell GA, Kantor ED, Lampe JW, Kristal AR, Heckbert SR, White E (2014) Intake of long-chain ω-3 fatty acids from diet and supplements in relation to mortality. Am J Epidemiol 179:710–720. https://doi.org/10.1093/aje/kwt326
Villegas R, Takata Y, Murff H, Blot W (2015) Fish, omega-3 long-chain fatty acids, and all-cause mortality in a low-income US population: results from the Southern Community Cohort Study. Nutr Metab Cardiovasc Dis 25:651–658. https://doi.org/10.1016/j.numecd.2015.04.006
Gillum RF, Mussolino M, Madans JH (2000) The relation between fish consumption, death from all causes, and incidence of coronary heart disease: the NHANES I Epidemiologic Follow-up Study. J Clin Epidemiol 53:237–244. https://doi.org/10.1016/S0895-4356(99)00149-3
Bonaccio M, Ruggiero E, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Cerletti C, Donati M, de Gaetano G, Iacoviello L (2017) Fish intake is associated with lower cardiovascular risk in a Mediterranean population: prospective results from the Moli-sani study. Nutr Metab Cardiovasc Dis 27:865–873. https://doi.org/10.1016/j.numecd.2017.08.004
Calder PC (2020) n-3 PUFA and inflammation: from membrane to nucleus and from bench to bedside. Proc Nutr Soc 79:404–416. https://doi.org/10.1017/S0029665120007077
Chapkin RS, Davidson LA, Ly L, Weeks BR, Lupton JR, McMurray DN (2007) Immunomodulatory effects of (n-3) fatty acids: putative link to inflammation and colon cancer. J Nutr 137:200S-204S. https://doi.org/10.1093/jn/137.1.200S
Kang JX, Leaf A (1996) Antiarrhythmic effects of polyunsaturated fatty acids: recent studies. Circulation 94:1774–1780. https://doi.org/10.1161/01.CIR.94.7.1774
De Caterina R, Madonna R, Zucchi R, La Rovere MT (2003) Antiarrhythmic effects of omega-3 fatty acids: from epidemiology to bedside. Am Heart J 146:420–430. https://doi.org/10.1016/S0002-8703(03)00327-2
Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S (2020) Fish consumption and the risk of cardiovascular disease and mortality in patients with type 2 diabetes: a dose-response meta-analysis of prospective cohort studies. Crit Rev Food Sci Nutr 61:1640–1650. https://doi.org/10.1080/10408398.2020.1764486
Takata Y, Zhang X, Li H, Gao Y, Yang G, Gao J, Cai H, Xiang Y, Zheng W, Shu X (2013) Fish intake and risks of total and cause-specific mortality in 2 population-based cohort studies of 134,296 men and women. Am J Epidemiol 178:46–57. https://doi.org/10.1093/aje/kws584
Wang MP, Thomas GN, Ho SY, Lai HK, Mak KH, Lam TH (2011) Fish consumption and mortality in Hong Kong Chinese-the LIMOR study. Ann Epidemiol 21:164–169. https://doi.org/10.1016/j.annepidem.2010.10.010
Chen A, Zhou W, Hou J, Nevill A, Ding YL, Wan YH, Jester R, Qin X, Hu Z, Chen R (2022) Impact of older age adiposity on incident diabetes: a community-based cohort study in China. Diabetes Metab J. https://doi.org/10.4093/dmj.2021.0215
Acknowledgements
The authors thank the participants and all who were involved in the five provinces’ cohort study.
Funding
The data collection of the five provinces’ cohort study was funded by the BUPA Foundation (Grants Nos. 45NOV06, and TBF-M09-05) and Alzheimer’s Research UK (Grant No. ART/PPG2007B/2). The data management and the final work of the manuscript were supported by the Research fund of Anhui Medical University, China (Grant No. 2021xkjT049). Professor Ruoling Chen and Dr James J Tang thank an EU H2020 MSCA Fellowship (Grant No. DEMAIRPO-799247) to investigate the risk of dementia in relation to air pollution mediated by fish intake.
Author information
Authors and Affiliations
Contributions
ATB: searched and reviewed the topic related literature, performed the data analysis, and drafted the manuscript. AC, XT, and JH: commented, revised, and wrote the manuscript for its 2nd version. YY, AN, and JJT: data management and data analysis supervision, and manuscript comments. JG, JN, and ZH: data collection and co-ordination, design of the cohort study, interpretation of data and manuscript comments. SR and JC: critically reviewed and revised the manuscript. RC: study concept and design, study supervision, manuscript revision, and a guarantor for this paper. All authors checked and approved the manuscript final version.
Corresponding authors
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Ethical approval
The ethical approval for the study was obtained from the Research Ethics Committee, Anhui Medical University, China (Ref. none, granted in 2010), and the Research Ethics Committee, the School of Health, University of Wolverhampton, UK (Ref. A1- Favourable, granted in 2010).
Consent to participate
Permission for interview and informed consent were obtained from each participant.
Consent for publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bakre, A.T., Chen, A., Tao, X. et al. Impact of fish consumption on all-cause mortality in older people with and without dementia: a community-based cohort study. Eur J Nutr 61, 3785–3794 (2022). https://doi.org/10.1007/s00394-022-02887-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02887-y