Abstract
Purpose
The objective of this study was to compare the effects of 12 weeks of resistance training combined with either 5:2 intermittent fasting or continuous energy restriction on body composition, muscle size and quality, and upper and lower body strength.
Methods
Untrained individuals undertook 12 weeks of resistance training plus either continuous energy restriction [20% daily energy restriction (CERT)] or 5:2 intermittent fasting [~ 70% energy restriction 2 days/week, euenergetic consumption 5 days/week (IFT)], with both groups prescribed a mean of ≥ 1.4 g of protein per kilogram of body weight per day. Participants completed 2 supervised resistance and 1 unsupervised aerobic/resistance training combination session per week. Changes in lean body mass (LBM), thigh muscle size and quality, strength and dietary intake were assessed.
Results
Thirty-four participants completed the study (CERT = 17, IFT = 17). LBM was significantly increased (+ 3.7%, p < 0.001) and body weight (− 4.6%, p < 0.001) and fat (− 24.1%, p < 0.001) were significantly reduced with no significant difference between groups, though results differed by sex. Both groups showed improvements in thigh muscle size and quality, and reduced intramuscular and subcutaneous fat assessed by ultrasonography and peripheral quantitative computed tomography (pQCT), respectively. The CERT group demonstrated a significant increase in muscle surface area assessed by pQCT compared to the IFT group. Similar gains in upper and lower body strength and muscular endurance were observed between groups.
Conclusion
When combined with resistance training and moderate protein intake, continuous energy restriction and 5:2 intermittent fasting resulted in similar improvements in body composition, muscle quality, and strength. ACTRN: ACTRN12620000920998, September 2020, retrospectively registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Energy-restricted diets are becoming increasingly popular amongst individuals for a variety of reasons, including improving body composition and general health and wellbeing. Regardless of the reason, these diets commonly lead to weight loss in the form of both fat and lean body mass (LBM) [1]. While fat loss is usually desirable, reductions in skeletal muscle mass (a major component of LBM) may lead to a number of deleterious short- and long-term consequences, such as hyperphagia and reduced basal metabolic rate, which may compromise long term weight loss success [2]; increased risk of strength loss and disability, especially in older adults [3, 4]; and potential metabolic issues incumbent with low muscle mass [5].
The mechanisms behind weight-loss-induced reductions in LBM are not fully understood, however; the impact of energy restriction on protein turnover and net muscle protein balance may be a contributing factor [6]. Skeletal muscle mass is determined by a balance between muscle protein synthesis (MPS) and muscle protein breakdown (MPB), which remains equal during energy balance [7]. Conversely, during short-term, continuous energy restriction, both post-prandial and post-absorptive MPS are reduced [8], which may lead to an overall negative protein balance, higher protein catabolism to supply amino acids and reductions in muscle mass [6]. Whether this also occurs over extended periods of energy restriction is unclear [9]. Notwithstanding, higher protein intakes, and/or performing resistance training have been shown to partially or completely attenuate these reductions in MPS [6, 10]. Moreover, these strategies, as well as others including slower rates of weight loss, have been utilised to successfully mitigate LBM loss during longer periods of energy restriction [1, 11].
Recently, interest in how the pattern of energy restriction affects changes in LBM during weight loss has increased. Compared to traditional energy-restricted diets that are characterised by moderate daily energy restriction (i.e. continuous energy restriction), alternative patterns such as intermittent fasting where periods of severe energy restriction are interspersed with regular dietary or ad libitum consumption might provide greater protection against LBM loss. Although evidence to support this is currently lacking [12], it seems plausible that short-term periods of energy balance or surplus, especially in close proximity to resistance training, may promote greater maintenance and accrual of LBM than continuous periods of energy restriction/deficit. This could be via greater output during training due to increased energy availability, or differences in acute changes in MPS and anabolic hormonal responses during periods of energy balance/surplus compared to energy deficit [8, 13].
A popular variation of intermittent fasting is the 5:2 fasting diet, which generally involves 2 days per week of severe (consumption of ~ 1600–3000 kJ/day) or complete energy restriction, paired with 5 days of ad libitum or euenergetic consumption [14, 15]. Despite widespread public popularity of the 5:2 intermittent fasting model, little research has investigated its effects on LBM compared to a continuous energy restriction diet, especially when combined with a resistance training program and higher protein intake [16]. Moreover, only a handful of intermittent fasting studies have utilised more sensitive assessments of muscle hypertrophy (e.g. ultrasonography) to simultaneously assess changes in muscle growth [17,18,19,20]. Thus, the purpose of this study was to investigate and compare the effects of 12 weeks of resistance training combined with either a 5:2 intermittent fasting or continuous energy restriction style diet matched for energy and protein intake on body composition (especially LBM), indicators of muscle hypertrophy and quality, and upper and lower body strength. The primary outcome of this study was a change in LBM. It was hypothesised that 5:2 intermittent fasting would result in maintenance or greater accrual of LBM compared with continuous energy restriction.
Methods
Participants
Participants were recruited through advertising on social media channels targeting current and past university students in Victoria, Australia. A total of 194 individuals responded to the advertisement and underwent initial screening. Only 44 were deemed eligible and were recruited for the study. Participants were eligible for inclusion if they: (i) were aged between 18 and 45 years; (ii) had a body mass index (BMI) of 22.0–35.0 kg/m2; (iii) had a body fat percentage > 18% for males or > 25% for females as measured via dual x-ray absorptiometry (DXA); (iv) had not followed a structured resistance training program in the previous 6 months and; (v) had been weight stable for 3 months prior to the study (< 5% weight loss or weight gain). Participants were excluded if they: (i) were smokers; (ii) had diabetes; (iii) had a history of cardiovascular disease; (iv) were taking dietary supplements and were unwilling to cease these for the duration of the study; (v) were taking glucose or lipid lowering, or weight loss medication; (vi) had a current physical condition that may have been exacerbated by resistance training as determined by their general practitioner, (vii) were pregnant or intended to become pregnant in the following 3–4 months; (viii) were menopausal or post-menopausal; (ix) had a history of disordered eating; (x) had a current or previous respiratory condition likely to be exacerbated by the intervention; (xi) had a current or previous gastrointestinal disorder likely to be exacerbated by the intervention; (xii) had any allergy to any components of the supplement product to be supplied; (xiii) were unable to commit to fasting on assigned days if randomised to the intermittent fasting group; (xiv) did not speak English at a level at which they were able to understand and complete the requirements of the study or; (xv) disclosed any other chronic disease or condition, or were taking any other medication that investigators deemed would contraindicate the study intervention.
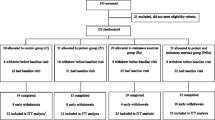
Randomisation and study overview
Participants who were eligible for the study were stratified by age, sex and BMI before being randomised by coin toss into either the intermittent fasting plus training (IFT) or continuous energy restriction plus training (CERT) groups for 12 weeks. The random allocation sequence was not explicitly concealed. Participants in the IFT group undertook a 5:2 style-fasting protocol, while those in the CERT group undertook a continuous energy restriction style feeding pattern. Both groups completed supervised resistance training twice per week, and resistance/aerobic combination training once per week. The intervention took place from February to November 2019, spread across 6 groups, starting 2–4 weeks apart. A flow chart showing participant movement through the study can be seen in Fig. 1. This study was approved by the Swinburne University of Technology Human Research Ethics Committee (project #2018/322).
Diet protocol
Basal energy requirements for all participants were calculated using the Mifflin St. Jeor equation [21], with total energy requirements calculated by applying an activity factor of 1.4 representing a recreational level of activity (based on prescribed exercise). At the beginning of the intervention period, all participants were provided with example meal plans that would result in mean consumption of approximately 80% of estimated energy requirements and 1.4 g of protein per kilogram of body weight per day (g/kg/day) over the 12 week intervention. Meal plans were customised based on food preferences for each individual and provided by a dietitian along with brief education on the Australian healthy eating guidelines [22]. As participants in the IFT group had limited energy available on fasting days to reach recommended protein intakes, they were provided with protein shakes and high protein soups to get as close to daily protein intake recommendations as possible. Participants were also instructed on how to use the Easy Diet Diary (Xyris Software, Australia, 2019) smartphone application to record their food, and substitute other foods of their choosing into the meal plans while maintaining the same energy and protein intake.
Intermittent fasting diet protocol
All participants in the IFT group were instructed to consume 100% of their energy requirements for 5 days per week (non-fasting days). On two non-consecutive and non-training days, participants consumed approximately 30% of their estimated energy requirements (~ 2100 kJ for females and ~ 2500 kJ for males) (fasting days), consistent with previous research [23, 24]. On fasting days, participants were prescribed a diet consisting of whey-based protein shakes (Formulite), high-protein soups and steamed/raw vegetables. The macronutrient composition of these supplements and the recommended intake on fasting days can be seen in Table 1. On fasting days, participants were asked to consume all energy during a 6 h window between 12.00 pm and 6.00 pm, to ensure an extended fasting period, but also allow flexibility of consumption to promote compliance. Further, they were allowed ad libitum consumption of non-energy providing beverages on fasting days. To match protein intakes across dietary groups as closely as possible, those in the IFT group were instructed to consume approximately 1.5 g/kg/day of protein on non-fasting days, as their fasting day diets only provided ~ 1.1–1.2 g/kg/day. This design resulted in the prescription of a 20% energy deficit and a mean intake of protein of 1.4 g/kg/day, designed to be isoenergetic and isonitrogenous with the CERT group to explore the differences between patterns of dietary intake while controlling for overall intake as much as possible.
Continuous energy restriction
Those randomised to the CERT group were instructed to consume ~ 80% of their total energy requirements daily for the duration of the 12 week intervention. This group represented a best practice ‘control’ group, as moderate energy restriction (15–30%) is most commonly recommended for weight loss [25, 26]. Furthermore, participants were also prescribed consumption of 1.4 g/kg/day of protein. Participants in this group also received customised meal plans and the same education as those in the IFT group.
Exercise protocol
All participants were required to undertake 3 training sessions each week: 2 resistance training sessions and 1 bodyweight aerobic/resistance training combination session. Training frequency of 3 times per week was seen as practical for the untrained participants, allowing adequate time for recovery, but also the stimulus for muscle growth. The two resistance training sessions were conducted at Swinburne University’s Hawthorn campus, and were supervised by an accredited strength and conditioning coach (who was also the study dietitian). The 2 supervised sessions consisted of variations of the following exercises: push-ups, squats, rows, lunges, bicep curls and dips (Supplemental Fig. 1). The exercises utilised were chosen due to their lack of technical difficulty given the untrained population being researched. Participants completed these exercises in a superset style workout, aiming to complete 12–15 repetitions of each exercise. Once participants were able to complete 3 sets of 15 repetitions in any individual exercise, the weight was increased or exercise variation made more difficult, adhering to the principles of progressive overload. The one bodyweight aerobic/resistance training combination session per week was completed by participants at home using bodyweight exercises consisting of planks, mountain climbers, crunches, burpees, lying side toe-touches and hip bridges. These exercises were also completed using a superset format with 2 min breaks, however, were timed instead of counting repetitions. When participants reached their time goal with good form (self-assessed), they were instructed to increase this by 5 s. All exercise sessions were conducted on non-fasting days in the IFT group to promote maximal energy availability and avoid any detrimental effects of fasting on exercise performance.
Assessments
Bodyweight and body composition analysis
Weekly weight measurements were taken in light clothing using bioelectrical impedance scales [Multifrequency segmental body composition analyser; MC-780 Tanita Corporation (Tokyo, Japan)]. Lean body mass, fat mass and body fat percentage were assessed utilising dual x-ray absorptiometry [DXA; Hologic Horizon (Bedford MA)] at baseline and after the intervention period, as previously detailed [27]. The DXA was calibrated for bone mineral density, muscle and fat masses on the morning of each assessment in accordance with manufacturer guidelines using spine and whole-body phantoms, respectively. Short and long-term coefficient of variation for these measurements were well within the acceptable level set by the manufacturer (< 5%).
Ultrasound
Muscle thickness, cross-sectional area (CSA) and muscle quality [echogenicity (EI)], were measured using ultrasound (SonoSite M-Turbo, SonoSite Australasia Pty Ltd, New South Wales, Australia) with a linear array transducer (5–2 MHz) for the rectus femoris (RF) and vastus intermedius (VI) of the non-dominant leg at baseline and post intervention (Supplemental Fig. 2). All images were acquired and analysed by the same technician. A fidelity check of the image acquisition and analysis was conducted by a health professional with over 10 years of experience in ultrasound imaging and analysis. Varying depths were required to obtain full visualisation of the RF in some instances, however, the gain was kept consistent across measurements. Measurements were acquired with participants in a supine position, with their knee in passive extension. Ultrasound gel was applied to the transducer, which was placed perpendicular to the long axis of the anterior thigh, at a distance of two-thirds from the anterior, superior iliac spine to the superior patellar border, consistent with previous studies [28]. Muscle thickness and CSA were measured in real-time with the on-board functions of the M-turbo, utilising the straight line and tracing functions, respectively. Images were also saved onto the on-board hard drive before being transferred onto a personal computer for EI analysis using ImageJ software (NIH, Bethesda, MD) [29]. EI for RF and VI were measured utilising a standard square of 100 × 100 pixels, or where the predefined square did not fit within the cross section of the muscle, the largest square that fit within the anatomic boundaries of the muscle was utilised, a method which has shown good inter-observer reliability regardless of the level of expertise [30].
Peripheral quantitative computed tomography (pQCT)
pQCT was utilised to measure the surface area of muscle, intramuscular fat and subcutaneous fat at baseline and post intervention (Supplemental Fig. 3). A single 2.5 mm transverse pQCT; (Stratec XCT3000, Stratec Medizintechnik GmbH, Pforzheim, Germany) scan with a voxel size of 0.4 mm was obtained at mid-thigh region of the non-dominant leg. The mid-thigh was defined as midway between the tip of the greater trochanter and medial edge of the tibial plateau, located by deep palpation. The images were exported and further analyzed by Slice-O-Matic™ (Tomovision, Montreal, CA) to determine the muscle, intramuscular fat and subcutaneous fat volumes as previously described [31,32,33]. After visual checks; where due to beam hardening artefacts the tissue was not segmented (“tagged”) optimally, the assignment of individual voxels or small voxel islands were changed into the correct tissue manually, at the discretion of the operator. The pQCT was calibrated using the manufacturer’s phantom daily, with a coefficient of variation of 0.2%, as described previously [34].
All imaging and image analyses were carried out by a single experienced image analysis specialist (EB) or under his direct supervision.
Strength testing
Strength testing was undertaken prior to the diet intervention and at the end of week 12. A 3 repetition maximum (3RM) test and strength endurance test were performed for both bench press and leg press. While these exercises were not included within the resistance training program, these were chosen as a standardised method of strength testing using similar movements to those included. After a brief 5 min warm up, participants were instructed on correct lifting and breathing techniques before practicing these using submaximal loads for 10–15 repetitions. Weight was gradually added and repetitions reduced to serve as a functional warm up. Participants then completed a set of 3 repetitions at a self-selected weight close to their perceived capacity, followed by a 3 min rest, with weight being continually added to each subsequent attempt. 3RM was recorded as the last successful attempt before form breakdown, or failure to complete the lift without assistance. The 3RM of each participant was determined within 5 attempts. After the 3RM test, participants were allowed a 5 min rest before undergoing a strength endurance test. These were tested in order such that 3RM bench press was followed by the bench press endurance test, and 3RM leg press was followed by the leg press endurance test. Participants were required to complete as many repetitions as possible of each exercise utilising 70% of their estimated 1 repetition maximum (1RM), calculated from the attained 3RM utilising the Brzycki formula [35] {weight lifted/[1.0278 – (0.0278 × repetitions performed)]}. Failure was determined as the first repetition where the participant required assistance. Repetitions where form was considered inadequate were not counted; however, participants were not stopped from completing subsequent repetitions if this occurred. Volume was calculated as the number of repetitions completed at 70% of 1RM multiplied by the weight lifted.
Dietary intake
Participants were required to keep a 3 day food diary at baseline and in week 1, 6 and 12 using the Easy Diet Diary (Xyris Software, Australia, 2019) phone application. This software has been shown to produce results similar to other, more time-intensive methods of dietary data collection such as 24 h recalls [36]. Participants recorded all food and drink intake on non-consecutive days that included 2 weekdays and 1 weekend day. Food records were kept on non-fasting days for those in the IFT group. On fasting days, participants were asked to note down any extra food or drink consumed, and whether they had consumed their recommended supplements. Intake on these days was estimated from these records.
Statistical analysis
Changes in LBM were considered the primary outcome of this study. Sample size calculations were conducted using GPower version 3.1 [37] based on previous research showing a 2.4 kg loss of LBM in response to similar study methodology to that of the current study in a comparable population [38]. This was contrasted with research into intermittent fasting plus resistance or endurance training that has shown a minimal effect on LBM, albeit with smaller reductions in weight [16, 23]. It was calculated that using an α error probability of 0.05 and power of 80%, 22 participants would be required to detect a 2.4 kg difference in LBM between groups. Assuming a 33% attrition rate, total estimated sample size requirements were 29 participants. Results are presented as mean (± SD). Normality was assessed using the Shapiro–Wilk test and visual inspection of Q–Q plots. Assumptions of normality were violated for intramuscular fat only. Intramuscular fat was log10 transformed, resulting in normality. A linear mixed model with restricted maximum likelihood method was established based on a first-order autoregressive structure and used to analyse variables for main effects for time, group and sex, and all possible 2-way and 3-way interactions, with BMI and age included as random effects due to their inclusion as stratification variables. Differences between groups at baseline were analysed using independent t tests. Bivariate correlations using Pearson’s correlation co-efficient were calculated to assess relationships between variables and changes in LBM. All analyses were performed using SPSS version 25 (IBM Corp, Armonk, NY, 2017). A p < 0.05 was considered significant for all tests.
Results
Participant characteristics
There were a total of 17 completers in each group, with a nearly even split of males and females (IFT = 9 males and 8 females, CERT = 8 males and 9 females). Overall, 10 participants (n = 8 female and n = 2 male) failed to complete the interventions (CERT = 5, IFT = 5). Of these 10, 3 were unable to commit to the exercise sessions, 2 were unable to commit to the dietary protocol (IFT = 1, CERT = 1), and the remaining 5 dropped out due to unrelated medical issues or relocation. Baseline characteristics for participants are presented in Table 2. No significant differences were found at baseline between groups as a whole, or when split by sex (Supplementary Table 1).
Bodyweight and body composition analysis
Bodyweight and body composition measured before and after the intervention are presented in Table 3. There was a main effect for time for weight, BMI, body fat mass, body fat percentage and LBM, with significant reductions in weight, BMI, body fat mass and body fat percentage observed in both dietary groups, whereas LBM was significantly increased in both groups. There was also a main effect for sex for weight, LBM, fat mass and body fat percentage, with lower weight and LBM, but higher fat mass and body fat percentage noted for females. A significant time x sex interaction was evident for weight, BMI and LBM, with larger reductions in weight and BMI observed in males, but greater increases in LBM observed in females. Individual changes in weight, LBM and body fat can be seen in Supplementary Fig. 4.
Mid-thigh muscle surface area and intramuscular and subcutaneous fat analysis
pQCT
Muscle surface area and intramuscular and subcutaneous fat measured before and after the intervention via pQCT are reported in Table 3. A main effect for time was found for subcutaneous fat and log10 intramuscular fat with significant reductions occurring in both groups over time. A main effect for sex was also found for muscle surface area and subcutaneous fat, with larger muscle surface area, but lower subcutaneous fat noted for males. There was a time x group effect for muscle surface area, with those in the CERT group experiencing a mean increase in muscle surface area compared to the IFT group.
Ultrasound
RF thickness, CSA and EI, and VI thickness and EI measured before and after the intervention via ultrasound are presented in Table 3. A main effect for time for RF thickness, RF CSA and RF EI was noted, with RF thickness and CSA significantly increased in both groups over time, whereas RF EI significantly decreased in both groups over time. A main effect for sex was also found for RF thickness, RF CSA and RF EI, with larger RF thickness and CSA, but lower RF EI in males observed. There were no other significant interactions or main effects identified for RF measurements and/or all VI assessments.
Dietary intake analysis
Participant dietary intake data measured before and during the intervention are summarised in Table 4. There was a main effect for time for overall mean absolute daily energy intake in kJ, relative energy intake in kJ/kg, relative protein intake in g/kg, relative carbohydrate intake in g/kg and relative fat in g/kg, with significant reductions in energy (both absolute and relative), relative carbohydrate and fat intake identified across all groups, and a significant increase in relative protein intake. There was also a main effect for sex for mean absolute daily energy intake in kJ, with lower consumption in females. A significant time x sex interaction was found for relative energy intake (kJ/kg) and relative carbohydrate intake (g/kg), with females demonstrating greater reductions in energy and carbohydrate intake compared to males during the intervention period. Average energy restriction for those in the IFT and CERT groups were 31.0 ± 5.9% and 29.3 ± 6.5% for males and 33.9 ± 7.1% and 28.1 ± 6.1% for females respectively, with no significant difference between groups overall (IFT = 32.4 ± 6.4% versus CERT = 28.7 ± 6.1%).
Fasting versus non-fasting days in IFT participants
Differences in dietary energy and protein intake on fasting and non-fasting days for the IFT group are presented in Table 5. Energy intake on fasting days for females was significantly lower in week 12 compared to week 1. No other significant differences between time points on fasting or non-fasting days were found.
Upper body and lower body 3RM strength and endurance volume analysis
Changes in the bench press and leg press 3RM, and bench press and leg press endurance test volume are reported in Table 6. There were main effects for time for bench press 3RM, bench press volume, leg press 3RM and leg press volume, with increases noted in each of these variables across the intervention. There were also main effects for sex for bench press and leg press 3RM, and bench press and leg press volume, with lower values reported in females. No other significant interactions or main effects were identified for strength or endurance variables.
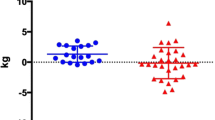
Correlations between variables and changes in LBM
Figure 2 shows the correlation between relative changes in body weight and body fat and LBM. There was a significant, moderate positive correlation between changes in LBM and weight in both groups overall (r = 0.63, p < 0.001), indicating that as weight loss increased, gains in LBM reduced. When split by intervention group, this relationship was strengthened in the CERT group (r = 0.86, p < 0.001), while no significant relationship was seen for the IFT group (r = 0.23, p = 0.38), with all but one IFT group participant increasing LBM regardless of percentage weight loss. Similarly, there was a moderate, significant correlation between the percentage of overall fat mass lost with changes in LBM in the CERT group (r = 0.53, p = 0.03), but not in the IFT group (r = − 0.21, p = 0.41). Change in LBM was negatively correlated with absolute relative energy (kJ/kg) (r = − 0.40, p = 0.02) and carbohydrate (g/kg) intake (r = − 0.36, p = 0.03) during the intervention and positively correlated with percent change in pQCT muscle area (r = 0.51, p = 0.003). Relative change (percent) in bench press 3RM (r = 0.48, p = 0.004) and leg press 3RM (r = 0.55, p = 0.001) were also positively correlated with changes in LBM. No other measurements were found to have significant correlations with change in LBM.
Discussion
To the authors’ knowledge, this is the first randomised trial to have compared the effects of 5:2 intermittent fasting and continuous energy restriction on body composition and strength adaptations when concurrently undertaking resistance training. Our findings suggest that when overall dietary energy and protein intake are similar, both energy-restricted diets induced comparable increases in LBM and strength, and reductions in weight and fat when combined with a 12 week resistance training program. In contrast, some differences were noted between groups in local assessments of the thigh muscle. Sex-dependent differences were also observed in both groups, specifically in weight and LBM responses, with males demonstrating greater weight loss, but less gains in LBM. This could be a reflection of weight-loss-induced impairment of LBM accrual, however; this concept requires further exploration.
In the current study, both dietary intervention groups experienced significant reductions in body fat (mean − 7.2 kg; 95% CI − 8.4 kg, − 6.0 kg) and increases in LBM (mean + 1.7 kg; 95% CI + 1.1 kg, + 2.3 kg) suggesting weight lost was exclusively from fat. While whole-body composition changes were similar between groups, increases in LBM have previously been more commonly reported in studies of individuals undertaking resistance training with continuous energy restriction than with intermittent fasting [39,40,41,42,43]. This could be a reflection of differences in daily energy restriction amounts but also study design, especially the training program. Studies demonstrating increases in LBM while utilising continuous energy restriction have commonly employed more frequent and/or intense training protocols (i.e. 5–7 days/week) compared to the common 3 days/week model typically used in intermittent fasting studies [16] and the present study. However, a 3 day/week training program could have important practical implications given it may be more appealing/realistic to undertake for a significant proportion of the general population. To our knowledge, only one other study has demonstrated significant increases in LBM when intermittent fasting and resistance training were combined [19]. In this study, per-protocol analysis showed an increase of 1.4 and 1.0 kg in LBM in trained women undertaking resistance training with and without β-hydroxy β-methylbutyrate (HMB), respectively. However, as no concomitant changes in weight were observed, it is likely that participants were in energy balance. This could explain why these participants gained LBM, in contrast to other studies which have demonstrated small to moderate reductions in weight (− 1.0 kg to − 3.3 kg) alongside small losses, no change, or statistically non-significant increases in LBM (− 0.4 kg to + 0.6 kg) [17, 18, 20, 39]. The paucity of studies investigating intermittent fasting with resistance training makes it difficult to ascertain if LBM can be gained when both are combined in conjunction with a concomitant energy deficit [16]. Moreover, intermittent fasting is a broad concept, and while alternate day fasting, time-restricted feeding and 5:2 all fit under this umbrella, there are significant differences in how these diets are applied. For example, while time-restricted feeding uses extended periods of fasting each day (16–20 h), if an energy deficit is prescribed, it is generally on a daily basis. On the other hand, while alternate day fasting and 5:2 IF are similar in that they generally prescribe severe restrictions on fasting days and no restrictions on non-fasting days, the number of fasting days each week is different. Therefore, it is difficult to make direct comparisons between these results and those of previous studies, even if the diets used are all broadly classified as intermittent fasting.
Ultrasound assessment showed a non-significantly (p = 0.05) greater increase in RF thickness in the CERT compared to the IFT group (CERT = + 0.18 cm; 95% CI + 0.13 cm, + 0.24 cm versus IFT = + 0.10 cm; 95% CI + 0.01 cm, + 0.19 cm), with similar non-significant (p = 0.07) findings for RF CSA (CERT = + 0.95 cm2; 95% CI + 0.65 cm2, + 1.25 cm2 versus IFT = + 0.58 cm2; 95% CI + 0.09 cm2, + 1.07 cm2). Similarly, pQCT demonstrated significantly (p = 0.03) greater increases in muscle area in the CERT group compared to IFT group (CERT = + 4.75 cm2; 95% CI + 1.76 cm2, + 7.73 cm2 versus IFT = − 0.69 cm2; 95% CI − 4.67 cm2, + 3.29 cm2). Observed differences between groups at the local musculature level could be due to a number of reasons. Firstly, it is known that muscle hypertrophy in response to resistance training does not occur uniformly throughout the body, with a upper body more responsive than lower body muscle mass [40,41,42] and thus it is likely that we missed changes in the upper body musculature by only assessing the thigh muscle. In support of this, it was noted that when examining DXA-derived regional differences in LBM, the IFT group showed greater relative increases in the upper body compared to those in the CERT group, albeit marginally, while the opposite was true for the lower body (Supplementary Table 2). Secondly, our small, uneven sample size may have been insufficient to identify real differences between diet groups when utilising more sensitive assessments of muscle, especially given the known large inter-individual variability in adaptations to resistance training [43]. Despite the differences, change in muscle surface area as measured by pQCT was positively correlated with changes in whole-body LBM (r = 0.51) for both groups combined, suggesting muscular hypertrophy may have underpinned the increases in LBM. These findings support the notion that muscle accrual can occur together with reductions in fat mass when energy deficits are combined with resistance training and protein intakes above standard daily recommendations [44,45,46,47,48].
Notable differences between sexes in terms of the magnitude of LBM change were evident in the present study. Female participants gained significantly more LBM on average (+ 2.5 kg; 95% CI + 1.7 kg, + 3.3 kg versus + 0.9 kg; 95% CI + 0.2 kg, + 1.6 kg) compared to males, but experienced less weight loss (− 2.2 kg; 95% CI − 3.8 kg, − 0.7 kg versus − 5.5 kg; 95% CI − 6.7 kg, − 4.4 kg). A number of sex-specific factors may explain the disparity in weight and fat reduction between males and females. First, although all participants were prescribed similar relative energy deficits (20–23%—with slight variation due to the standardised nature of fasting days), comparatively larger lean mass in males (and therefore higher energy requirements) would have led to a greater absolute energy deficit for males by ~ 600 kJ/day. Given that the reported energy deficit for both sexes was ~ 10% more than prescribed (~ 30%), the absolute difference between sexes was most likely greater than this. When combined with the fact that females may require a greater absolute energy deficit per unit of weight-loss [49], are more likely to under-report energy intake [50] and may be impacted by hormones that promote weight retention [51, 52], it is not surprising that males experienced greater weight and fat loss in the current study. Additionally, differences in total amounts (and therefore overall rate) of weight loss between sexes could partially explain the greater LBM gains in females compared to males. Previous research has shown that slower rates of weight loss may be beneficial for LBM preservation, though this finding is not ubiquitous in the literature [53]. Congruent with this, when all weight loss and LBM changes for both sexes were pooled together in the current study, there was a moderate, positive correlation between change in weight and change in LBM (r = 0.63). That is, as weight loss increased, LBM gains were reduced and potentially compromised. However, when split by diet, this relationship strengthened in the CERT group (r = 0.86), but weakened in the IFT group to be statistically non-significant (r = 0.23). This trend was also seen when comparing a relative overall fat loss with changes in LBM. These findings may suggest that when paired with resistance training, the 5:2 style diet could be protective/promote gains in LBM compared with continuous energy restriction when greater amounts of weight loss occur. However, given the contrasting observations in pQCT and ultrasound assessments, which favoured the CERT group in some measurements, this concept is speculative and requires further investigation.
Upper and lower body muscle strength and endurance were significantly increased over the 12 week period, regardless of dietary intervention. There was a moderate, positive correlation between increases in LBM and 3RM for both bench press (r = 0.48) and leg press (r = 0.55), suggesting that some of this increase may be attributable to growth in LBM, although given the untrained population studied, it is probable that neuromuscular adaptations also contributed significantly [42]. Regardless, this provides evidence that when combined with resistance training, both diets appeared to support increases in strength in a comparable manner.
There were a number of strengths of the current study. First, participants were supervised for the majority of their training sessions, allowing standardisation of form and effort. Second, frequent access to the study dietitian may have helped improve motivation and compliance. Third, we utilised non-invasive and reliable methods of assessment to measure changes in muscle size and quality alongside whole body LBM (pQCT and ultrasound), both of which have shown utility in clinical settings [54, 55].
Our study was also subject to a number of limitations. First, while frequent supervision and feedback for training and diet may have helped with study validity, this may not be practical for the general population. Second, although we collected detailed dietary data, the limitations of self-reported dietary intake are well known [56], and our ability to make strong inferences based on dietary data were limited. However, reported intake did reflect the aims of our study (i.e. increased intake on non-fasting days for the IFT compared to the CERT group). Third, it is unclear how the provision of supplements to the IFT group on fasting days may have affected compliance, or whether the supplements themselves may have contributed to the results. Fourth, as we did not record menstrual cycle for females, it is unclear whether this may have affected our results. Finally, the sample size calculation used in the present study was based on research using similar population demographics and study designs available at the time [16, 23, 38]. However, the effect size determined by the magnitude of difference in the primary outcome measure (i.e. LBM) does appear to be larger than those observed in more contemporary studies that focus on intermittent fasting and resistance training. Thus, the final sample size in the current study may have been too low to detect smaller (but potentially clinical meaningful) differences in LBM that could arise from similar interventions, and future research may benefit from including greater numbers to overcome this limitation.
In summary, 5:2 intermittent fasting or continuous energy restriction combined with moderate protein intake and resistance training over 12 weeks led to comparable LBM gains, weight and body fat loss, and improvements in muscle strength, endurance and quality. However, there were clear sexual dimorphic differences in a number of these outcomes, and some disparities between groups when the measurement of whole-body changes were compared to localised muscle changes. Future studies should investigate the longer-term impacts of 5:2 fasting in comparison to continuous energy restriction, but importantly, explore the relationship between transient changes in energy balance and protein turnover, weight loss and muscle mass accrual.
Abbreviations
- CSA:
-
Cross-sectional area
- CERT:
-
Continuous energy restriction plus training group
- DXA:
-
Dual x-ray absorptiometry
- EI:
-
Echogenicity
- IFT:
-
Intermittent fasting plus training group
- LBM:
-
Lean body mass
- MPB:
-
Muscle protein breakdown
- MPS:
-
Muscle protein synthesis
- pQCT:
-
Peripheral quantitative computed tomography
- RF:
-
Rectus femoris
- VI:
-
Vastus intermedius
- 1RM:
-
1-Repetition maximum
- 3RM:
-
3-Repetition maximum
References
Chaston TB, Dixon JB, O’Brien PE (2007) Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes 31:743–750
Dulloo AG (2017) Collateral fattening: when a deficit in lean body mass drives overeating. Obesity 25:277–279
Zibellini J, Seimon RV, Lee CMY et al (2016) Effect of diet-induced weight loss on muscle strength in adults with overweight or obesity—a systematic review and meta-analysis of clinical trials. Obes Rev Off J Int Assoc Study Obes 17:647–663. https://doi.org/10.1111/obr.12422
Santilli V, Bernetti A, Mangone M, Paoloni M (2014) Clinical definition of sarcopenia. Clin Cases Miner Bone Metab 11:177
Wolfe RR (2006) The underappreciated role of muscle in health and disease. Am J Clin Nutr 84:475–482. https://doi.org/10.1093/ajcn/84.3.475
Hector AJ, McGlory C, Damas F et al (2018) Pronounced energy restriction with elevated protein intake results in no change in proteolysis and reductions in skeletal muscle protein synthesis that are mitigated by resistance exercise. FASEB J 32:265–275
Burd NA, Tang JE, Moore DR, Phillips SM (2009) Exercise training and protein metabolism: influences of contraction, protein intake, and sex-based differences. J Appl Physiol 106:1692–1701
Areta JL, Burke LM, Camera DM et al (2014) Reduced resting skeletal muscle protein synthesis is rescued by resistance exercise and protein ingestion following short-term energy deficit. Am J Physiol-Endocrinol Metab 306:E989–E997
Carbone JW, McClung JP, Pasiakos SM (2019) Recent advances in the characterization of skeletal muscle and whole-body protein responses to dietary protein and exercise during negative energy balance. Adv Nutr 10:70–79
Pasiakos SM, Cao JJ, Margolis LM et al (2013) Effects of high-protein diets on fat-free mass and muscle protein synthesis following weight loss: a randomized controlled trial. FASEB J 27:3837–3847
Washburn RA, Szabo AN, Lambourne K et al (2014) Does the method of weight loss effect long-term changes in weight, body composition or chronic disease risk factors in overweight or obese adults? A systematic review. PLoS ONE 9:e109849
Roman YM, Dominguez MC, Easow TM et al (2019) Effects of intermittent versus continuous dieting on weight and body composition in obese and overweight people: a systematic review and meta-analysis of randomized controlled trials. Int J Obes 43:2017–2027
Murphy C, Koehler K (2020) Caloric restriction induces anabolic resistance to resistance exercise. Eur J Appl Physiol 120:1155–1164. https://doi.org/10.1007/s00421-020-04354-0
Harvie M, Wright C, Pegington M et al (2013) The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr 110:1534–1547
Catenacci VA, Pan Z, Ostendorf D et al (2016) A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Obes Silver Spring Md 24:1874–1883. https://doi.org/10.1002/oby.21581
Keenan S, Cooke MB, Belski R (2020) The effects of intermittent fasting combined with resistance training on lean body mass: a systematic review of human studies. Nutrients. https://doi.org/10.3390/nu12082349
Moro T, Tinsley G, Bianco A et al (2016) Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med 14:290
Tinsley GM, Forsse JS, Butler NK et al (2017) Time-restricted feeding in young men performing resistance training: a randomized controlled trial. Eur J Sport Sci 17:200–207
Tinsley GM, Moore ML, Graybeal AJ et al (2019) Time-restricted feeding plus resistance training in active females: a randomized trial. Am J Clin Nutr 110:628–640
Stratton MT, Tinsley GM, Alesi MG et al (2020) Four weeks of time-restricted feeding combined with resistance training does not differentially influence measures of body composition, muscle performance, resting energy expenditure, and blood biomarkers. Nutrients 12:1126
Mifflin MD, St Jeor ST, Hill LA et al (1990) A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 51:241–247
National Health and Medical Research Council (2013) Australian Dietary Guidelines. National Health and Medical Research Council, Canberra
Bhutani S, Klempel MC, Kroeger CM et al (2013) Alternate day fasting and endurance exercise combine to reduce body weight and favorably alter plasma lipids in obese humans. Obesity 21:1370–1379
Varady KA, Bhutani S, Klempel MC et al (2013) Alternate day fasting for weight loss in normal weight and overweight subjects: a randomized controlled trial. Nutr J 12:146
Yumuk V, Tsigos C, Fried M et al (2015) European guidelines for obesity management in adults. Obes Facts 8:402–424. https://doi.org/10.1159/000442721
Semlitsch T, Stigler FL, Jeitler K et al (2019) Management of overweight and obesity in primary care—a systematic overview of international evidence-based guidelines. Obes Rev Off J Int Assoc Study Obes 20:1218–1230. https://doi.org/10.1111/obr.12889
Hassan EB, Phu S, Vogrin S et al (2019) Diagnostic value of mid-thigh and mid-calf bone, muscle, and fat mass in osteosarcopenia: a pilot study. Calcif Tissue Int 105:392–402
Parry SM, El-Ansary D, Cartwright MS et al (2015) Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care 30:1151-e9
Abràmoff MD, Magalhaes P, Ram S (2004) Image processing with ImageJ. Biophotonics Int 11:36–42
Sarwal A, Parry SM, Berry MJ et al (2015) Interobserver reliability of quantitative muscle sonographic analysis in the critically ill population. J Ultrasound Med 34:1191–1200. https://doi.org/10.7863/ultra.34.7.1191
Bani Hassan E, Alderghaffar M, Wauquier F et al (2019) The effects of dietary fatty acids on bone, hematopoietic marrow and marrow adipose tissue in a murine model of senile osteoporosis. Aging 11:7938–7947. https://doi.org/10.18632/aging.102299
Bani Hassan E, Demontiero O, Vogrin S et al (2018) Marrow adipose tissue in older men: association with visceral and subcutaneous fat, bone volume, metabolism, and inflammation. Calcif Tissue Int 103:164–174. https://doi.org/10.1007/s00223-018-0412-6
Bani Hassan E, Ghasem-Zadeh A, Imani M et al (2019) Bone marrow adipose tissue quantification by imaging. Curr Osteoporos Rep 17:416–428. https://doi.org/10.1007/s11914-019-00539-5
Scott D, Shore-Lorenti C, McMillan L et al (2018) Associations of components of sarcopenic obesity with bone health and balance in older adults. Arch Gerontol Geriatr 75:125–131. https://doi.org/10.1016/j.archger.2017.12.006
Brzycki M (1998) A practical approach to strength training. McGraw-Hill
Ambrosini GL, Hurworth M, Giglia R et al (2018) Feasibility of a commercial smartphone application for dietary assessment in epidemiological research and comparison with 24-h dietary recalls. Nutr J 17:5. https://doi.org/10.1186/s12937-018-0315-4
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Wycherley TP, Noakes M, Clifton PM et al (2010) A high-protein diet with resistance exercise training improves weight loss and body composition in overweight and obese patients with type 2 diabetes. Diabetes Care 33:969–976. https://doi.org/10.2337/dc09-1974
Oh M, Kim S, An K-Y et al (2018) Effects of alternate day calorie restriction and exercise on cardio-metabolic risk factors in overweight and obese adults: an exploratory randomized controlled study. BMC Public Health 18:1124
Abe T, DeHoyos DV, Pollock ML, Garzarella L (2000) Time course for strength and muscle thickness changes following upper and lower body resistance training in men and women. Eur J Appl Physiol 81:174–180. https://doi.org/10.1007/s004210050027
Cureton KJ, Collins MA, Hill DW, McElhannon FM (1988) Muscle hypertrophy in men and women. Med Sci Sports Exerc 20:338–344. https://doi.org/10.1249/00005768-198808000-00003
Folland JP, Williams AG (2007) Morphological and neurological contributions to increased strength. Sports Med 37:145–168. https://doi.org/10.2165/00007256-200737020-00004
Erskine RM, Jones DA, Williams AG et al (2010) Inter-individual variability in the adaptation of human muscle specific tension to progressive resistance training. Eur J Appl Physiol 110:1117–1125. https://doi.org/10.1007/s00421-010-1601-9
Garthe I, Raastad T, Refsnes PE et al (2011) Effect of two different weight-loss rates on body composition and strength and power-related performance in elite athletes. Int J Sport Nutr Exerc Metab 21:97–104. https://doi.org/10.1123/ijsnem.21.2.97
Josse AR, Atkinson SA, Tarnopolsky MA, Phillips SM (2011) Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. J Nutr 141:1626–1634. https://doi.org/10.3945/jn.111.141028
Longland TM, Oikawa SY, Mitchell CJ et al (2016) Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: a randomized trial. Am J Clin Nutr 103:738–746. https://doi.org/10.3945/ajcn.115.119339
Petrizzo J, DiMenna FJ, Martins K et al (2017) Case study: the effect of 32 weeks of figure-contest preparation on a self-proclaimed drug-free female’s lean body and bone mass. Int J Sport Nutr Exerc Metab 27:543–549. https://doi.org/10.1123/ijsnem.2016-0313
Demling RH, DeSanti L (2000) Effect of a hypocaloric diet, increased protein intake and resistance training on lean mass gains and fat mass loss in overweight police officers. Ann Nutr Metab 44:21–29. https://doi.org/10.1159/000012817
Hall KD (2008) What is the required energy deficit per unit weight loss? Int J Obes 32:573–576. https://doi.org/10.1038/sj.ijo.0803720
Burrows TL, Ho YY, Rollo ME, Collins CE (2019) Validity of dietary assessment methods when compared to the method of doubly labeled water: a systematic review in adults. Front Endocrinol 10:850. https://doi.org/10.3389/fendo.2019.00850
Hagobian TA, Sharoff CG, Stephens BR et al (2009) Effects of exercise on energy-regulating hormones and appetite in men and women. Am J Physiol Regul Integr Comp Physiol 296:R233-242. https://doi.org/10.1152/ajpregu.90671.2008
Lizcano F, Guzmán G (2014) Estrogen deficiency and the origin of obesity during menopause. BioMed Res Int 2014:757461. https://doi.org/10.1155/2014/757461
Ashtary-Larky D, Bagheri R, Abbasnezhad A et al (2020) Effects of gradual weight loss v. rapid weight loss on body composition and RMR: a systematic review and meta-analysis. Br J Nutr. https://doi.org/10.1017/S000711452000224X
Fukumoto Y, Ikezoe T, Yamada Y et al (2012) Skeletal muscle quality assessed from echo intensity is associated with muscle strength of middle-aged and elderly persons. Eur J Appl Physiol 112:1519–1525. https://doi.org/10.1007/s00421-011-2099-5
Cawthon PM, Fox KM, Gandra SR et al (2009) Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? J Am Geriatr Soc 57:1411–1419. https://doi.org/10.1111/j.1532-5415.2009.02366.x
Subar AF, Freedman LS, Tooze JA et al (2015) Addressing current criticism regarding the value of self-report dietary data. J Nutr 145:2639–2645. https://doi.org/10.3945/jn.115.219634
Acknowledgements
The authors would like to acknowledge Formulite for donating all supplement shakes and soups used in the study and Sonosite Australia for providing the ultrasound equipment. This study received in-kind support from the Imaging and Image Analysis Centre at the Australian Institute for Musculoskeletal Science (AIMSS).
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. SK was supported by a student scholarship from Swinburne University. All protein shake and soup supplements were donated by Formulite. Ultrasound equipment was provided by Sonosite Australia. Support for image analysis was received in-kind from the Imaging and Image Analysis Centre at the Australian Institute for Musculoskeletal Science (AIMSS).
Author information
Authors and Affiliations
Contributions
SK, RB, MC, SW, DE designed research. SK, RB, MC, EB, MI conducted the research. WSC, JS, SK performed the statistical analyses. SK, MC, RB wrote the paper; all authors contributed to the final manuscript. SK, MC, RB had primary responsibility for the final content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest.
Ethical approval
This study was approved by the Swinburne University of Technology Human Research Ethics Committee (project #2018/322).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants consented to have non-identifiable data published.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keenan, S.J., Cooke, M.B., Hassan, E.B. et al. Intermittent fasting and continuous energy restriction result in similar changes in body composition and muscle strength when combined with a 12 week resistance training program. Eur J Nutr 61, 2183–2199 (2022). https://doi.org/10.1007/s00394-022-02804-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02804-3