Abstract
Purpose
Menopause disturbs energy, glucose, and lipid metabolisms and changes the composition of the gut microbiota, but dietary fibers without phytoestrogens may ameliorate menopausal metabolic disorders. The objective of the present study was to assess whether consuming the prebiotics chitosan and citrus pectin can improve postmenopausal symptoms, possibly by modulating the gut microbiota in ovariectomized (OVX) rats, and the mechanism of action was examined.
Methods
The OVX rats were given 4.5% cellulose (OVX-Control), chitosan (OVX-Chitosan), or citrus pectin (OVX-Pectin) in a 43% fat diet and the sham rats were given the same diet as the OVX-Control for 12 weeks. Sham-operated rats had the same diet as OVX-Control (Normal-Control). Body-weight, visceral fat mass, tail skin temperature, serum 17β-estradiol, glucose intolerance, and insulin tolerance were determined. Gut microbiota in the fecal samples was measured by NGS and analyzed with PICRUSt2. Short-chain fatty acids (SCFA) and metabolomic characteristics of serum were also measured with UPLC-mass spectrometry.
Results
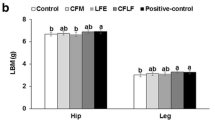
Chitosan and citrus pectin were selected because the incubation of rat feces with these two prebiotics in vitro had shown increased butyrate production. OVX-Chitosan reduced the weight, visceral fat content, and tail skin temperature, and OVX-Chitosan and OVX-Pectin improved glucose tolerance, compared to the OVX-Control. Both alleviated dyslipidemia, compared to the OVX-Control. OVX-Chitosan and OVX-Pectin elevated serum propionate and butyrate concentrations but only OVX-Chitosan lowered serum acetate concentrations. In PICRUSt2, chitosan upregulated the functional genes of gut microbiota involved in valine, leucine, and isoleucine biosynthesis, whereas the OVX-Control exhibited significantly upregulated lipopolysaccharide biosynthesis. OVX-Pectin exhibited increased α-diversity in the fecal bacteria. Metabolomic analysis revealed higher serum urate concentrations in the OVX-Control group than the other groups, and serum arginine and leucine concentrations were higher in the OVX-Chitosan group (P < 0.05).
Conclusion
Chitosan and citrus pectin consumptions improved menopausal symptoms by improving the diversity and composition of the gut microbiota, and serum metabolites and SCFA originating from fecal bacteria. Chitosan was more effective for improving menopausal symptoms than citrus pectin.





Similar content being viewed by others
Abbreviations
- OVX:
-
Ovariectomy
- OVX-Control:
-
OVX rats having 4.5% dextrin in a high-fat diet
- OVX-Chitosan:
-
OVX rats having 4.5% chitosan in a high-fat diet
- OVX-Pectin:
-
OVX rats having 4.5% citrus pectin in a high-fat diet; Normal-Control, Sham-operated rats having 4.5% dextrin in a high-fat diet
- LDL:
-
Low-density lipoproteins; SCFA, short-chain fatty acid
- OGTT:
-
Oral glucose tolerance test; IPITT, intraperitoneal insulin tolerance test
- OPLS-DA:
-
Orthogonal partial least squares discriminant analysis
- PICRUSt2:
-
Phylogenetic Investigation of Communities by Reconstruction of Unobserved States
- NGS:
-
Next-generation sequencing
- PCoA:
-
Principal coordinates analysis
- PERMANOVA:
-
Permutational multivariate analysis of variance
- KEGG:
-
Kyoto encyclopedia of genes and genomes
References
Lee AW, Ness RB, Roman LD, Terry KL, Schildkraut JM, Chang-Claude J et al (2016) Association between menopausal estrogen-only therapy and ovarian carcinoma risk. Obstet Gynecol 127:828–836
Delzenne NM, Rodriguez J, Olivares M, Neyrinck AM (2020) Microbiome response to diet: focus on obesity and related diseases. Rev Endocr Metab Disord. https://doi.org/10.1007/s11154-020-09572-7
Yan S, Tian Z, Li M, Li B, Cui W (2019) Effects of probiotic supplementation on the regulation of blood lipid levels in overweight or obese subjects: a meta-analysis. Food Funct 10:1747–1759
Bubnov RV, Babenko LP, Lazarenko LM, Mokrozub VV, Demchenko OA, Nechypurenko OV et al (2017) Comparative study of probiotic effects of Lactobacillus and Bifidobacteria strains on cholesterol levels, liver morphology and the gut microbiota in obese mice. EPMA J 8:357–376
Griffith RJ, Alsweiler J, Moore AE, Brown S, Middleton P, Shepherd E et al (2020) Interventions to prevent women from developing gestational diabetes mellitus: an overview of cochrane reviews. Cochrane Database Syst Rev 6:Cd012394
Muscogiuri G, Cantone E, Cassarano S, Tuccinardi D, Barrea L, Savastano S et al (2019) Gut microbiota: a new path to treat obesity. Int J Obes 9:10–19
Tilg H, Adolph TE (2015) Influence of the human intestinal microbiome on obesity and metabolic dysfunction. Curr Opin Pediatr 27:496–501
Keenan MJ, Janes M, Robert J, Martin RJ, Raggio AM, McCutcheon KL et al (2013) Resistant starch from high amylose maize (HAM-RS2) reduces body fat and increases gut bacteria in ovariectomized (OVX) rats. Obesity 21:981–984
Mayengbam S, Lambert JE, Parnell JA, Tunnicliffe JM, Nicolucci AC, Han J et al (2019) Impact of dietary fiber supplementation on modulating microbiota-host-metabolic axes in obesity. J Nutr Biochem 64:228–236
He M, Shi B (2017) Gut microbiota as a potential target of metabolic syndrome: the role of probiotics and prebiotics. Cell Biosci 7:54
Koh A, De Vadder F, Kovatcheva-Datchary P, Backhed F (2016) From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165:1332–1345
Wang L, Zhu Q, Lu A, Liu X, Zhang L, Xu C et al (2017) Sodium butyrate suppresses angiotensin II-induced hypertension by inhibition of renal (pro)renin receptor and the intrarenal renin-angiotensin system. J Hypertens 35:1899–1908
Perry RJ, Zhang X-M, Zhang D, Kumashiro N, Camporez J-PG, Cline GW et al (2014) Mechanism for the anti-diabetic effect of leptin. Nat Med 20:759
Miyamoto J, Kasubuchi M, Nakajima A, Irie J, Itoh H, Kimura I (2016) The role of short-chain fatty acid on blood pressure regulation. Curr Opin Nephrol Hypertens 25:379–383
Cheung RCF, Ng TB, Wong JH, Chan WY (2015) Chitosan: an update on potential biomedical and pharmaceutical applications. Mar Drugs 13:5156–5186
Prajapati B, Rajput P, Jena PK, Seshadri S (2015) Investigation of chitosan for prevention of diabetic progression through gut microbiota alteration in sugar rich diet-induced diabetic rats. Curr Pharm Biotechnol 17:173–184
Wicker L, Kim Y, Kim M-J, Thirkield B, Lin Z, Jung J (2014) Pectin as a bioactive polysaccharide—extracting tailored function from less. Food Hydrocoll 42:251–259
Park S, Kim DS, Kang ES, Kim DB, Kang S (2018) Low-dose brain estrogen prevents menopausal syndrome while maintaining the diversity of the gut microbiomes in estrogen-deficient rats. Am J Physiol Endocrinol Metab 315:E99–e109
Yeon S, Oh K, Kweon S, Hyun T (2016) Development of a dietary fiber composition table and intakes of dietary fiber in Korea National Health and Nutrition Examination Survey (KNHANES). Korean J Community Nutr 21:293–300
Ribeiro WR, Vinolo MAR, Calixto LA, Ferreira CM (2018) Use of gas chromatography to quantify short-chain fatty acids in the serum, colonic luminal content, and feces of mice. Bio Protocol 8:3089
Jeong SY, Kang S, Hua CS, Ting Z, Park S (2017) Synbiotic effects of beta-glucans from cauliflower mushroom and Lactobacillus fermentum on metabolic changes and gut microbiome in estrogen-deficient rats. Genes Nutr 12:31
Charan J, Kantharia ND (2013) How to calculate sample size in animal studies? J Pharmacol Pharmacother 4:303–306
Peacock K, Ketvertis KM (2020) Menopause. StatPearls. StatPearls Publishing, Treasure Island
Hevener AL, Clegg DJ, Mauvais-Jarvis F (2015) Impaired estrogen receptor action in the pathogenesis of the metabolic syndrome. Mol Cell Endocrinol 418(Pt 3):306–321
Quigley EMM (2019) Prebiotics and probiotics in digestive health. Clin Gastroenterol Hepatol 17:333–344
O’Connor S, Chouinard-Castonguay S, Gagnon C, Rudkowska I (2017) Prebiotics in the management of components of the metabolic syndrome. Maturitas 104:11–18
Morrison DJ, Preston T (2016) Formation of short-chain fatty acids by the gut microbiota and their impact on human metabolism. Gut microbes 7:189–200
Heimann E, Nyman M, Degerman E (2015) Propionic acid and butyric acid inhibit lipolysis and de novo lipogenesis and increase insulin-stimulated glucose uptake in primary rat adipocytes. Adipocyte 4:81–88
Holscher HD (2017) Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes 8:172–184
Trivedi VR, Satia MC, Deschamps A, Maquet V, Shah RB, Zinzuwadia PH et al (2016) Single-blind, placebo-controlled randomized clinical study of chitosan for body weight reduction. Nutr J 15:3
Tang D, Wang Y, Kang W, Zhou J, Dong R, Feng Q (2020) Chitosan attenuates obesity by modifying the intestinal microbiota and increasing serum leptin levels in mice. J Func Foods 64:103659
Debédat J, Amouyal C, Aron-Wisnewsky J, Clément K (2019) Impact of bariatric surgery on type 2 diabetes: contribution of inflammation and the gut microbiome? Semin Immunopathol 41:461–475
Tilg H, Zmora N, Adolph TE, Elinav E (2020) The intestinal microbiota fuelling metabolic inflammation. Nat Rev Immunol 20:40–54
Lin TL, Shu CC, Chen YM, Lu JJ, Wu TS, Lai WF et al (2020) Like cures like: pharmacological activity of anti-inflammatory lipopolysaccharides from gut microbiome. Front Pharmacol 11:554
Wotzka SY, Kreuzer M, Maier L, Arnoldini M, Nguyen BD, Brachmann AO et al (2019) Escherichia coli limits Salmonella typhimurium infections after diet shifts and fat-mediated microbiota perturbation in mice. Nat Microbiol 4:2164–2174
Ma S, Qin J, Hao Y, Shi Y, Fu L (2020) Structural and functional changes of gut microbiota in ovariectomized rats and their correlations with altered bone mass. Aging 12:10736–10753
Wang C, Symington JW, Ma E, Cao B, Mysorekar IU (2013) Estrogenic modulation of uropathogenic Escherichia coli infection pathogenesis in a murine menopause model. Infect Immun 81:733–739
Ricaud K, Even M, Lavigne F, Davail S, Arroyo J (2019) Evolution of intestinal microbiota and body compartments during spontaneous hyperphagia in the greylag goose. Poult Sci 98:1390–1402
Hino S, Morita T (2017) Pectin and its hydrolysates stimulate intestinal mucin secretion. FASEB J 31:968.962
Aguilar EC, da Silva JF, Navia-Pelaez JM, Leonel AJ, Lopes LG, Menezes-Garcia Z et al (2018) Sodium butyrate modulates adipocyte expansion, adipogenesis, and insulin receptor signaling by upregulation of PPAR-gamma in obese Apo E knockout mice. Nutrition 47:75–82
Müller M, Hernández MAG, Goossens GH, Reijnders D, Holst JJ, Jocken JWE et al (2019) Circulating but not fecal short-chain fatty acids are related to insulin sensitivity, lipolysis, and GLP-1 concentrations in humans. Sci Rep 9:12515
Asghar A, Sheikh N (2017) Role of immune cells in obesity-induced low-grade inflammation and insulin resistance. Cell Immunol 315:18–26
Dopkins N, Nagarkatti PS, Nagarkatti M (2018) The role of the gut microbiome and associated metabolome in the regulation of neuroinflammation in multiple sclerosis and its implications in attenuating chronic inflammation in other inflammatory and autoimmune disorders. Immunology 154:178–185
Tibullo D, Li Volti G, Giallongo C, Grasso S, Tomassoni D, Anfuso CD et al (2017) Biochemical and clinical relevance of alpha-lipoic acid: antioxidant and anti-inflammatory activity, molecular pathways and therapeutic potential. Inflamm Res 66:947–959
Monirujjaman M, Ferdouse A (2014) Metabolic and physiological roles of branched-chain amino acids. Adv Mol Biol 2014:364976
Gui S, Jia J, Niu X, Bai Y, Zou H, Deng J et al (2014) Arginine supplementation for improving maternal and neonatal outcomes in the hypertensive disorder of pregnancy: a systematic review. J Renin Angio Aldo S 15:88–96
Wu M, Xiao H, Shao F, Tan B, Hu S (2020) Arginine accelerates intestinal health through cytokines and intestinal microbiota. Int Immunopharmacol 81:106029
Acknowledgements
This research and the study design and methods were evaluated and approved for funding by the National Research Foundation (NRF-2019R1A2C1007203), Korea.
Author information
Authors and Affiliations
Contributions
Contributed to the experimental design: SP, XW; Conducted the animal study and biochemical assays. XW, MJK. Wrote the first draft of the manuscript: XW; Reviewed and edited the manuscript: SP; All authors reviewed the manuscript and they read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical standards
All experimental procedures were performed according to the guidelines for the care and use of laboratory animals from the National Research Council and with the approval of the Animal Care and Use Review Committee at Hoseo University (HSIACUC-18-231), Korea.
Rights and permissions
About this article
Cite this article
Wu, X., Kim, M.J., Yang, H.J. et al. Chitosan alleviated menopausal symptoms and modulated the gut microbiota in estrogen-deficient rats. Eur J Nutr 60, 1907–1919 (2021). https://doi.org/10.1007/s00394-020-02382-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02382-2