Abstract
Purpose
To report daily total fluid intake (TFI) and fluid types in Indonesia according to age, sex, socio-economic status (SES) and geographic region, and compare TFI with the Indonesian adequate fluid intake (AI) recommendations.
Methods
Data were collected in 32 cities over nine regions from children (4–9 years, n = 388), adolescents, (10–17 years, n = 478) and adults (18–65 years, n = 2778) using a fluid intake 7-day record (Liq.In7); socio-economic status was also recorded. The 7-day mean TFIs were compared with the AI of water set by the Ministry of Health of the Republic of Indonesia.
Results
Total median fluid intakes for all age groups exceeded 2000 mL/day. At population level, TFI was associated with household income (P < 0.001), education (P < 0.001) and Indonesian geographical regions (P < 0.001). More than 67% of participants met the AI of water from fluids. A higher percentage of children and adolescents met the AI (78 and 80%, respectively), compared with adults (72%). Drinking water was the main contributor to TFI in all age groups (76–81%). Sugar-sweetened beverages (SSB) were consumed by 62% children, 72% adolescents and 61% of adults. An SSB intake ≥ 1 serving per day was observed for 24% children, 41% adolescents and 33% adults.
Conclusions
A high percentage of the population drank enough to meet the AI of water from fluids. Water was the most frequently consumed drink; however, many participants consumed at least one serving of SSB per day. This study provides data to help direct targeted intervention programs.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Nutrition and diet surveys are used to identify public health priorities. With increasing recognition of the role of water and adequate hydration in the prevention [1, 2] and management of diseases [3, 4], it is essential that such surveys assess total water and fluid intake to inform such priorities. Age- and sex-specific recommendations on adequate intake (AI) of water have been established for many countries, for example, the USA Institute of Medicine [5]. These recommendations for total water intake (TWI) are based on the median intakes of water at population level, while the European Food Safety Authority (EFSA) [6] used data from population-level intakes, desirable volume of water per energy unit consumed, and desirable urinary osmolarity. The Indonesian Ministry of Health applied the same method as EFSA and has published dietary recommendations on the adequate intake of water (Online Resource Table S1) [7].
One of the difficulties that experts face when developing dietary reference values for water is the diversity of environmental conditions including humidity and temperature across countries and regions [8]. Daily water requirements in hot weather (40 °C) can be triple of those in cooler climates (20 °C) for any given energy expenditure [9]. For example, a recent study in Japanese adults [10] reported total water intake to be approximately 10% higher in summer than winter. Water losses and, therefore, requirements may also be influenced by other factors including humidity, air motion and clothing. Therefore, EFSA added the caveat that the AIs only apply in moderate environmental temperatures and at moderate physical activity levels [6]. In an archipelago country such as Indonesia with different temperature and humidity among major islands, it is particularly important to collect such data; however, to date there is a paucity of such information.
Recommendations are usually for adequate total water intake (TWI), which includes water from fluids and food (the latter sometimes referred to as food moisture). The water content of food varies considerably; therefore, the contribution of food to TWI will also vary. For example, it has been reported to be 19% in the USA [5], 40% in China [11] and 51% in Japan [10]. EFSA estimated in 2010 that water from food was 20-30% based on the data available at that time. However, more recent publications have estimated the contribution of food moisture to be 27% in the UK [12], 33% in the Republic of Ireland [13] and 36% in France [12]. There is a paucity of information on the contribution of water from food to TWI in hot, humid countries. When developing their recommendations for adequate intake of water the Indonesian Ministry of Health estimated that food contributed 20% to daily TWI [7]. This is in agreement with a study in Indonesia that estimated the contribution of food to TWI to be approximately 20% [14]. However, this contrasted markedly with a study from another hot, humid country, namely Bolivia that showed that food contributed an average of 50% to TWI [15]. The authors attributed this to an attempt to reduce exposure to waterborne pathogens.
Access to safe drinking water is an issue in many parts of the world [16] including, perhaps surprisingly, parts of the USA [17]. Lack of adequate safe drinking water supply is not necessarily linked to the overall wealth of the country. However, differences in individual socio-economic status (SES) have been shown to affect the risk of dehydration within a community; lower SES was associated with a higher adjusted odds ratio for elevated urine osmolality, which in turn was associated with differences in access to tap water [18]. In a rapidly developing country such as Indonesia, SES may further influence access to safe drinking water and ability to purchase bottled water.
Collecting data on total water intake has several challenges as it is difficult to obtain complete information on both food and fluid intake over a period of several days, not least due to the burden placed on participants. Fluids account for the majority of TWI and are a key target when developing interventions to increase water intake or reduce energy intake from drinks. To provide more complete data on the volume and type of fluids consumed, the present survey focused on TFI. While information is available on fluid intake from the Indonesian Total Diet Study [19], the data were collected using single 24-h recalls, which have been shown to significantly underestimate TFI [20]. In addition, these data were not analyzed according to SES.
Therefore, the primary aim of the present survey was to report daily total fluid intake (TFI) using a 7-day fluid intake (Liq.In7) record [21], and the contribution of different fluid types to TFI in Indonesia according to age group, sex, SES and geographic region. Earlier studies [22, 23] compared TWI in Indonesia with the EFSA recommendations [6]; since then recommendations on the AI of water have become available in Indonesia [7]. The second aim of this survey was to compare TFI with the Indonesian AIs.
Methods
Design and study population
The present analysis reports cross-sectional survey data for children (4–9 years), adolescents (10–17 years) and adults (18–65 years); this survey forms part of the Liq.In7 study. The method of recruitment, the instruments for data collection and data treatment were harmonized with the Liq.In7 surveys published elsewhere [24,25,26]. The data collection was performed in May 2016; this month was chosen for operational reasons. Temperature and humidity for the study locations were recorded using average daily information, from the following website http://www.timeanddate.com/weather/indonesia and shown in Online Resource Table S2.
Participants were randomly recruited in 32 cities over nine regions (Bali, Central Java, East Java, West Java, Yogyakarta, Jabodetabek, Sumatera, Kalimantan and Sulawesi; Online Resource Table S2) via a systematic door-to-door approach until the quotas for age, sex, habitat (urban/rural) and socioeconomic characteristics in relation to the total country population were met. Total household income, education and employment status were recorded as measures of SES.
Individuals who were not able to read and write in the language of the questionnaire (Bahasa Indonesia) or who were traveling within the next 10 days were excluded. Individuals working in the advertising, marketing, market research, the media, manufacture, distribution and/or sale of water and any kind of beverage were also excluded, as these individuals might be more aware of their fluid intake. Only one individual (regardless of age) per household was eligible to participate. If more than one member of the household was willing to take part the researcher chose the participant based on the need to satisfy the preset quotas. Pregnancy or lactation was not an exclusion criterion. There were no health-based exclusion criteria; therefore, everyone who self-reported themselves as being healthy was included.
Participants were given detailed information about the survey’s objectives, their involvement, their rights to confidentiality, risks and benefits, and a clear explanation that participation in the survey was entirely voluntary. All participants gave informed oral consent to take part in the survey. No monetary incentive was offered for taking part in the survey. All data were recorded and analyzed anonymously. The survey protocol was reviewed and approved by the University of Arkansas Review Board (ref. 14-12-376).
Anthropometry
Height (m) and weight (kg) were measured by the researchers using suitably calibrated portable height measure and portable digital scales (GEA model number BR9202) using standard procedures [27]. The body mass index (BMI) was calculated (kg/m2) for adults and BMI z-score for individuals ≤ 18 years.
Assessment of total fluid intake and the different fluid types
Participants were provided with the Liq.In7 record; a 7-day fluid-specific record validated for accuracy and reliability, although not in the Indonesian population [21]. The Liq.In7 record was presented in the official country language. A paper version of the record was delivered and explained to the participants during an interview at home. After a period of 7 days, the record was collected by the researcher after checking for completion with the participant. The Liq.In7 record was structured according to 12 occasions throughout the day including; awakening, meal times and periods, between meals and during the night. The participants were instructed to report all drinking events at any moment of the day with the following details: fluid type, size of the container from which the fluid was drunk, actual volume consumed, where the consumption took place and if the fluid was consumed with or without food. Food consumption was not recorded. To assist the participants in estimating the volume of fluid consumed, a photographic booklet of standard fluid containers was also provided. For children younger than 12 years, the primary caregiver was responsible for completing the record.
Classification and analysis of fluid types
The fluids recorded were classified into the following categories: water (tap and bottled water); milk and milk derivatives; hot beverages (coffee, tea and other hot beverages); 100% fruit juices; sugar-sweetened beverages (SSB) including carbonated soft drinks (CSD); juice-based drinks; functional beverages, e.g., energy and sports drinks; ready to drink tea and coffee; flavored water; artificial/non-nutritive sweeteners beverages (A/NSB) (diet/zero/light soft drinks) and other beverages. Full details are given in Online Resource Table S3. A participant was defined as a consumer of a certain fluid type if this fluid type was consumed at least once during the 7-day period. Volumes of all categories were summed to give TFI. The proportion of individuals drinking ≤ 1 serving (250 mL) of SSB per week, 2–6 servings of SSB per week and ≥ 1 serving/day intake of SSB was calculated (Online resource Figure S3). These cut-offs were obtained from meta-analyses associating such intakes with potential risks for the development of obesity, type 2 diabetes and metabolic syndrome [28,29,30].
Comparison with adequate intake of water from fluids
The observed 7-day mean TFIs were compared with the AI of water from fluids set by the Ministry of Health of the Republic of Indonesia [7] to determine the percentage of individuals in each age and sex group with TFIs meeting the AIs. The AIs for TWI were reduced by 20% to account for water in food; henceforth, this will be referred to as AI of water from fluids. Previous research has shown the contribution of food moisture to TWI to be approximately 20% [14]; the Indonesian Ministry of Health also estimated that food moisture in Indonesia was 20% when the AIs were developed [7]. The cut-offs for AI of TWI and total water from fluids can be found in Online Resource Table S1. To allow comparisons with previously published data from the Liq.In7 surveys, the comparison between observed intakes and the AI of water from fluids set by EFSA is also provided in the Online Resource Figure S1 [6].
Statistical analysis
The demographic and anthropometric characteristics of the survey population are presented either as means and standard deviation for continuous variables, or numbers and percentages for dichotomous variables. Participants who did not complete the full 7-day fluid record and/or participants reporting a mean total daily fluid intake below 0.4 L/day, or higher than 6 L/day, were excluded from the analysis. No weightings were applied to the data. All intakes were skewed data (Online Resource Figure S2); therefore, TFIs are presented as medians and percentiles; mean and standard error of the mean (SEM) are given for completeness. The intakes of the different fluids are presented as median (25th − 75th percentiles) (Table 3 and Online Resource Table S4a–c). The mean and standard error of mean (SEM) of the different fluid types can be found as Online Resource Tables S5a and b. Intakes are estimated values for all participants, including non-consumers. Between-group comparisons were tested by Wilcoxon rank tests for continuous variables. All statistical tests were two tailed and as there were multiple comparisons, the significance level was set at P < 0.001. All analyses were performed using the SPSS software version 22.0 (SPSS Inc, Chicago, IL).
Results
Sample description
The demographic and anthropometric characteristics of the survey population are shown in Table 1. The mean ages of the three groups (children, adolescents and adults) were 6.4 (± 1.7), 13.4 (± 2.3) and 35.5 (± 12.1) years, respectively. The mean BMIs were 21.7 (± 14.4) kg/m2 for children, 22.3 (± 16.2) kg/m2 and 23.2 (± 5.5) kg/m2 for adolescents and adults respectively. Household income was similarly distributed for all age groups. The regions of Jabodetabek (an urban area of Jakarta) and Sumatera represented over 40% of the sample, while Bali and Yogyakarta represented less than 6% in all age groups.
Daily total fluid intake
The daily TFIs for each sex, age group and geographic region are shown in Table 2; there were no significant differences by sex in any age group. However, there was a variation of over 1.5 L/day in fluid intakes for all age and sex categories. Total median (25th–75th percentiles) fluid intakes for the three age categories were 2156 (1430–2896) mL/day and 2080 (1436–3164) mL/day for boys and girls aged 4–9 years; 2460 (1674–3164) mL/day and 2379 (1627–3012) mL/day for males and females aged 10–17 years and 2553 (1822–3402) mL/day and 2640 (1836–3515) mL/day for adult men and women, respectively. TFI was significantly different (P < 0.0001) between Indonesian regions.
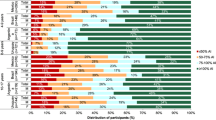
Comparison of total fluid intakes with adequate intakes set by the Institute of Medicine, Indonesia (2014) according to age and sex categories
Figure 1 shows the proportion of participants who drank more or less than the Indonesian AI of water from fluids (Online Resource Table S1) [7]. Online Resource Figure S1 shows TFI compared with the AI of water from fluids set by EFSA [6]. In all age and sex categories, at least 67% of participants met the AI of water from fluids. Table 3 shows the number and percentage of participants meeting or exceeding the recommendations according to region, household income, education level and employment status. Across the age groups, West Java had the lowest number of participants meeting or exceeding the AIs. The number of participants meeting or exceeding the AI increased with income for adults although this was less apparent in children and adolescents. Neither education level nor employment status appeared to influence the number of participants meeting or exceeding the AI. Children not meeting the AI were drinking less than 315 mL/day than the recommendations. This increased to 399 mL/day for adolescents and 531 mL/day for adults.
Proportion (%) of participants showing different intake levels of water from fluids compared to the age- and sex-specific adequate intake (AI) recommended by the Indonesian Ministry of Health (2012) [8]
Daily intake of different fluid types
All participants drank water, which represented 77% of TFI in children, 78% in adolescents and 80% in adults (Fig. 2). Table 4 shows the median daily intakes of the types of fluid and percentage consumers for each age group. These data were highly skewed as shown by the interquartile ranges. A higher percentage of children and adolescents drank bottled water than boiled tap water. This pattern was different in adults with an intake of 617 mL/day of boiled tap water and 480 mL/day of bottled water. The percentage of individuals consuming hot beverages increased with age (33% of children, 53% of adolescents and 73% of adults) although volumes consumed were comparatively small; tea was more frequently drunk than coffee. Consumption of milk and its derivatives decreased with increasing age. Sugar-sweetened beverages were consumed at least once a week by 62% children, 72% adolescents and 61% of adults, with ready-to-drink tea being the most frequently consumed SSB. Data according to age group are shown in Online Resource Table S4 a–c. In the total survey population, 41% of children, 29% of adolescents and 41% of adults drank ≤ 1 serving of SSB per week. An intake of 2–6 servings of SSB per week was recorded by 34% of children, 29% of adolescents and 26% of adults. A higher proportion of adolescents, children and adults consumed ≥ 1 servings of SSB per day (41, 24, and 33%, respectively) (Figure S3 in online resources).
Associations between type of consumed and measures of social economic status
There was a gradient in consumption of bottled or boiled tap water (Table 5) with participants in the highest income bracket consuming significantly more bottled water (P < 0.0001) and significantly less tap water (P < 0.0001). There was a low median (25–75th) intake of 34 (0–1162) mL/day of bottled water in the lowest income households. A similar gradient was observed between education level and types of water consumed with participants in the lowest education group consuming significantly more tap water (P < 0.0001) and significantly less bottled water than participants in the two most educated groups (P < 0.0001) (Table 6). No relationship was observed between type of water consumed and employment status (Table S7 in Online Resources).
Discussion
This cross-sectional survey reports TFI and fluid type for children, adolescents and adults aged 4–65 years in Indonesia in an attempt to study the fluid intake pattern across nine regions of Indonesia. In the present survey, 67–80% of participants reported daily TFIs that met the Indonesian recommendations on adequate intake [7]. These rates are higher than previous data from Indonesia 55–70% [22, 23] where EFSA recommendations were used [6]. While undoubtedly the use of Indonesian recommendations is more appropriate and may account for the differences reported, there are other possible explanations. For example, recently there has been an increased emphasis in promoting the drinking of water in Indonesia. Water, as opposed to fluids generally, is now included in Indonesia’s food-based dietary guidelines Tumpeng Gizi Seimbang (TGS, Balanced Nutritional Pyramid) [31]. While this, and other, campaigns may have increased public knowledge and awareness of healthy hydration, to date there are no published evaluations of the impact these initiatives may have had. Improved access to drinking water may also have been a factor in this apparent increase in participants meeting the recommended AI for water from fluids. However, improving access to water for drinking and sanitation is a health priority in Indonesia [32] and access to, at least, basic drinking water has increased from 70% of the population in 1990 [33] to nearly 80% in 2015 [16]. Despite this, there are still disparities in access due to geographical and socioeconomic differences [34]. However, it is also important to consider the representativeness of the present study as this increase may be due to the voluntary nature of participation, which, by default, leads to a select group of participants who may have been better motivated to consume higher volumes.
Data from another Indonesian study conducted, under varying climatic conditions, showed intakes for adolescents and adults similar to the present study [35]. However, it should be noted that the areas surveyed in both studies although overlapping are geographically and, therefore, climatically different. In addition to the differences in sample size, the age ranges were also different (10–17 vs. 15–18 years and 18–65 vs. 19–55 years); younger children were not included in the earlier study. Another cross-sectional study of urban school children reported similar intakes to the present study [14]. The study by Hardinsyah et al. used a 7-day recall (semi-quantitative food frequency questionnaire) [35], and the second study 2-day, 24-h recalls [14]; neither methodology was validated for assessing TFI. The more recent Indonesian Total Diet Study [19] reported an average TFI of 1317 mL/day, with adults having an average intake of nearly 1500 mL/day. It is interesting to note that despite the volumes reported in the aforementioned study, nearly half of the population was described as dehydrated based on urine specific gravity and symptoms of dehydration [19]. Secondary analysis of these data found that the dehydration risk was related to ecological (geographical) area and fluid intake [36]. The present survey also showed that geographic region was significantly associated with TFI. As hydration status was not assessed in the present study, no association between the TFI and dehydration risk could be assessed. However, it is important to note that while the majority of participants in the present study met, or exceed the recommended AIs, those not drinking enough to meet these recommendations would need to drink between 351 and 531 mL/day (at least one to two servings) depending on age. Given the association between ambient temperature and urine specific gravity [37], it is vital that more research is conducted to further elucidate the effect of climate, including ambient temperature and altitude on TFI and the risk of dehydration, especially in those not meeting AI recommendations.
Socioeconomic status may influence several factors associated with fluid intake including access to safe tap water, ability to purchase bottled water and other drinks, access to heating facilities to boil water for drinking and air conditioning. In the present survey, TFI was related to household income and education, not employment status. SES has been associated with risk of dehydration and access to clean tap water in American countries [18, 38]. Several studies have also shown socio-economic differences in patterns of different types of fluid intake, with lower SES being associated with higher consumption of sugar-sweetened beverages [39,40,41]. Unfortunately, fluid type was not analyzed in relation to any measure of SES in the present survey as small numbers in some fluid type groups meant that further analysis would have been meaningless. It is important to recognize that the interpretation of the influence of SES on TWI and the types of fluid consumed is confounded by factors that may or may not be included in the definition of SES. For example, a recent analysis has shown that TWI was affected by education level, ethnicity and place of birth [42].
Water was drunk by all the participants in the present survey. Earlier studies in Indonesia have also shown that water was the largest contributor to TFI [14, 35]. Intake of SSBs was low in the present survey compared with previous Indonesian studies [43, 44] although 24% of children, 41% of adolescents and 33% of adults reported consuming at least one serving per day. The intake of this amount of SSB has been associated with a 25% increased future risk of type 2 diabetes [45]. In addition, obesity is a significant risk factor for type 2 diabetes; the consumption of SSB was also independently and positively associated with and increased risk of obesity [46,47,48] and cardiovascular disease [28, 49]. Because of the high risk of overweight and obesity in Indonesia [50,51,52] and a predicted rise in the prevalence of diabetes [52] there has been a call for policies to address the increasing prevalence of type 2 diabetes [53] and the amount of sugar in SSB [54, 55]. However, a recent review has identified the need for a nationwide nutrition survey in Indonesia using appropriate methodology, before developing such policies [56]. The present study may, therefore, be useful at a national level to develop health initiatives in Indonesia in the future.
This study has several strengths; perhaps the most significant being the use of a standardized methodology that has been validated, although not in Indonesia, for assessing TFI against total body water measured by deuterium dilution [21]. The sample size was particularly large and included participants from most of the Indonesian islands. However, it is important to acknowledge possible limitations. As with all dietary surveys, the sample may have been biased towards those people most interested in this topic and/or in their diet and health and those willing to complete such research. In addition, the present sample may not be truly representative of the total population; the eastern part of Indonesia was not represented, and the sample size in some regions was small. Moreover, compared with the 2011 statistics of the Indonesian Central Bureau of Statistics (BPS), the survey sample contained fewer individuals with a lower SES and living in rural areas than the national population. In addition, these data were collected using survey procedures and as such not weighted; therefore, its representativeness of the country’s population may be questioned. The levels of overweight and obesity for adults were comparable with published figures [53] although higher than WHO figures for children [57]. Conversely, the levels of underweight for children in the present survey were substantially lower than has previously been published [55, 57]. Again, this may be a reflection of underrepresentation in lower SES groups and in rural areas. Physical activity level and occupation will greatly influence fluid intake; however, activity was not recorded in this survey. Due to the methodology with parents/carers completing the record for children under 12 years old, there is a greater potential for intakes to be under- or overestimated. No information was collected about food consumption during the study period and, therefore, it was not possible to estimate the contribution of food moisture to TWI for this population sample. While food moisture was estimated to be 20% of TWI in the current analysis, more research is needed to confirm or refute this assumption. It should also be acknowledged that it is not possible to draw any conclusions about the hydration status of the participants as no biomarkers of hydration were measured. The present survey was conducted in May and intakes may not be representative of consumption at other times of the year especially in such a hot, humid country.
Conclusions
The present study presents data on volume and type of fluids consumed over a 7-day period in a large sample of the Indonesian population aged 4–65 years. The majority of the survey population drank enough to meet or exceed the Indonesian recommendations. However, in those not meeting the recommendations, an extra 351–531 mL/day (1–2 average servings) would need to be consumed to reach the recommended intakes. The most frequently consumed drink was water in all age and sex categories, although a significant percentage of individuals consumed at least one serving of SSB per day, a level of consumption that has been associated in different studies with an increased risk of type 2 diabetes and obesity. With rapidly increasing levels of type 2 diabetes in Indonesia, this study highlights a possible contributing factor and suggests possible targets for intervention.
References
Strippoli GF, Craig JC, Rochtchina E, Flood VM, Wang JJ, Mitchell P (2011) Fluid and nutrient intake and risk of chronic kidney disease. Nephrology (Carlton) 16(3):326–334. https://doi.org/10.1111/j.1440-1797.2010.01415.x
Enhorning S, Hedblad B, Nilsson PM, Engstrom G, Melander O (2015) Copeptin is an independent predictor of diabetic heart disease and death. Am Heart J 169(4):549–556 e541. https://doi.org/10.1016/j.ahj.2014.11.020
Clark WF, Sontrop JM, Huang SH, Moist L, Bouby N, Bankir L (2016) Hydration and chronic kidney disease progression: a critical review of the evidence. Am J Nephrol 43(4):281–292. https://doi.org/10.1159/000445959
Fresan U, Gea A, Bes-Rastrollo M, Ruiz-Canela M, Martinez-Gonzalez MA (2016) Substitution models of water for other beverages, and the incidence of obesity and weight gain in the SUN cohort. Nutrients. https://doi.org/10.3390/nu8110688
Institute of Medicine, Food and Nutrition Board (2004) Dietary Reference Intakes for water, potassium, sodium, chloride and sulfate. National Academies Press, Washington DC. https://www.nap.edu/read/10925/chapter/1 Accessed 29 May 2018
EFSA Panel on Dietetic Products Nutrition and Allergies (NDA) (2010) Scientific Opinion on Dietary reference values for water. EFSA Journal 8 (3):1459–1507. https://doi.org/10.2903/j.efsa.2010.1459
Ministry of Health of the Republic of Indonesia (2013) Recommended Nutritional Intake for Indonesian Population; Ministry of Health: Jakarta, Indonesia
Bernal J (2015) Hydration guidelines for fractionation of liquid intake in hot environments: report of Latin America. Nutr Hosp 32(S2):10269. https://doi.org/10.3305/nh.2015.32.sup2.10269
Sawka MN, Cheuvront SN, Carter R (2005) Human water needs. Nutr Rev 63(6 Pt 2):S30–S39
Tani Y, Asakura K, Sasaki S, Hirota N, Notsu A, Todoriki H, Miura A, Fukui M, Date C (2015) The influence of season and air temperature on water intake by food groups in a sample of free-living Japanese adults. Eur J Clin Nutr 69(8):907–913. https://doi.org/10.1038/ejcn.2014.290
Ma G, Zhang Q, Liu A, Zuo J, Zhang W, Zou S, Li X, Lu L, Pan H, Hu X (2012) Fluid intake of adults in four Chinese cities. Nutr Rev 70(S2):S105-S110. https://doi.org/10.1111/j.1753-4887.2012.00520.x
Guelinckx I, Tavoularis G, Konig J, Morin C, Gharbi H, Gandy J (2016) Contribution of water from food and fluids to total water intake: analysis of a French and UK Population Surveys. Nutrients 8(10):630. https://doi.org/10.3390/nu8100630
O’Connor L, Walton J, Flynn A (2014) Water intakes and dietary sources of a nationally representative sample of Irish adults. J Hum Nutr Diet 27(6):550–556. https://doi.org/10.1111/jhn.12189
Briawan DRP, Ka D (2011) Drinking habits and fluids intakes of school children in Urban. J Nutr Food 6(3):186–191
Rosinger A, Tanner S (2015) Water from fruit or the river? Examining hydration strategies and gastrointestinal illness among Tsimane’ adults in the Bolivian Amazon. Public Health Nutr 18(6):1098–1108. https://doi.org/10.1017/S1368980014002158
WHO/UNICEF (2017) Progress on Drinking Water, Sanitation and Hygiene. https://www.unicef.org/publications/index_96611.html Accessed 29 May 2018
Balazs CL, Ray I (2014) The drinking water disparities framework: on the origins and persistence of inequities in exposure. Am J Public Health 104(4):603–611. https://doi.org/10.2105/AJPH.2013.301664
Brooks CJ, Gortmaker SL, Long MW, Cradock AL, Kenney EL (2017) Racial/ethnic and socioeconomic disparities in hydration status among US adults and the role of tap water and other beverage intake. Am J Public Health 107(9):1387–1394. https://doi.org/10.2105/AJPH.2017.303923
Badan Penelitian dan Pengembangan Kesehatan (2014) Studi Diet Total Provinsi DKI Jakarta Tahun 2014: Survey Konsumsi Makanan Pribadi. http://terbitan.litbang.depkes.go.id/penerbitan/index.php/lpb/catalog/book/163 Accessed 22 August 2017
Bardosono S, Monrozier R, Permadhi I, Manikam NR, Pohan R, Guelinckx I (2015) Total fluid intake assessed with a 7-day fluid record versus a 24-h dietary recall: a crossover study in Indonesian adolescents and adults. Eur J Nutr 54(S2):17–25. https://doi.org/10.1007/s00394-015-0954-6
Johnson EC, Peronnet F, Jansen LT, Capitan-Jimenez C, Adams JD, Guelinckx I, Jimenez L, Mauromoustakos A, Kavouras SA (2017) Validation testing demonstrates efficacy of a 7-day fluid record to estimate daily water intake in adult men and women when compared with total body water turnover measurement. J Nutr 147(10):2001–2007. https://doi.org/10.3945/jn.117.253377
Ferreira-Pego C, Guelinckx I, Moreno LA, Kavouras SA, Gandy J, Martinez H, Bardosono S, Abdollahi M, Nasseri E, Jarosz A, Babio N, Salas-Salvado J (2015) Total fluid intake and its determinants: cross-sectional surveys among adults in 13 countries worldwide. Eur J Nutr 54(S2):35–43. https://doi.org/10.1007/s00394-015-0943-9
Iglesia I, Guelinckx I, De Miguel-Etayo PM, Gonzalez-Gil EM, Salas-Salvado J, Kavouras SA, Gandy J, Martinez H, Bardosono S, Abdollahi M, Nasseri E, Jarosz A, Ma G, Carmuega E, Thiebaut I, Moreno LA (2015) Total fluid intake of children and adolescents: cross-sectional surveys in 13 countries worldwide. Eur J Nutr 54(S2):57–67. https://doi.org/10.1007/s00394-015-0946-6
Zhang NMC, Guelinckx I, Moreno LA, Kavouras SA, Gandy J, Martinez H, Salas-Salvadó J, Ma G (2018) Fluid intake in China: results of the 2016 Liq.In7 national cross-sectional surveys. Eur J Nut. https://doi.org/10.1007/s00394-018-1747-5
Martinez HMC, Gandy J, Carmuega E, Arredondo JL, Pimentel C, Moreno LA, Kavouras SA, Salas-Salvadó J, Guelinckx I (2018) Fluid intake of Latin American adults: results of four 2016 Liq.In7 national cross-sectional surveys. Eur J Nut. https://doi.org/10.1007/s00394-018-1724-z
Gandy JMH, Carmuega E, Arredondo JL, Pimmental C, Moreno LA, Kavouras SA, Salas-Salvadó J, Guelinckx I (2018) Fluid intake of Latin American children and adolescents: results of four 2016 Liq.In7 national cross-sectional surveys. Eur J Nut. https://doi.org/10.1007/s00394-018-1728-8
WHO (1995) Report of a WHO Expert Committee: Physical status: the use and interpretation of anthropometry. Technical Report Series No. 854. World Health Organization, Geneva
Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB (2009) Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr 89(4):1037–1042 (pii: 0.3945/ajcn.2008.27140)
Hu FB, Malik VS (2010) Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav 100(1):47–54. https://doi.org/10.1016/j.physbeh.2010.01.036
Malik VS, Pan A, Willett WC, Hu FB (2013) Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 98(4):1084–1102. https://doi.org/10.3945/ajcn.113.058362
Ministry of Health, Republic of Indonesia (2014) Pedoman Gizi Seimbang.. http://gizi.depkes.go.id/download/Pedoman%20Gizi/PGS%20Ok.pdf Accessed 29 May 2017
FAO/WHO National Nutrition Strategy Paper of Indonesia In: 2nd International Conference on Nutrition ICN2, Jakarta, 2014
Patunru A (2015) Access to Safe Drinking Water and Sanitation in Indonesia. Asia Pac Policy Stud 2(2):234–244. https://doi.org/10.1002/app5.81
Irianti SPP, Sasimartoyo TP, Lee A (2016) Determinants of household drinking-water source in Indonesia: An analysis of the 2007 Indonesian family life survey. Cogent Med 3(1):1151143
Hardinsyah SE, Briawan D, Damayanthi E, Dwiriani CM, Effendi YH, Dewi M, Aries M (2009) Drinking Habits and Hydration Status Among Teenagers and Adults in Two Different Ecological Areas. Food and Nutrition Society of Indonesia (PERGIZI PANGAN Indonesia) Department of Community Nutrition, Faculty of Human Ecology, IPB Danone, Indonesia
Gustam (2012) Risk Factors of Dehydration in Adolescents and Adults. Thesis Ecology Institute of Agricultural. Bogor, Indonesia
Rosinger A (2015) Heat and hydration status: Predictors of repeated measures of urine specific gravity among Tsimane’ adults in the Bolivian Amazon. Am J Phys Anthropol 158(4):696–707. https://doi.org/10.1002/ajpa.22813
Soares LC, Griesinger MO, Dachs JN, Bittner MA, Tavares S (2002) Inequities in access to and use of drinking water services in Latin America and the Caribbean. Rev Panam Salud Publica 11(5–6):386–396
Rosinger AHK, Gahche J, Park S, Frenk SM (2017) Percentage of Total daily kilocalories consumed from sugar-sweetened beverages among children and adults, by sex and income lever-National Health and Nutrition Examination Survey, United States, 2011–2014. MMWR Morb Mortal Wkly Rep 66(6):181
Grimes CA, Szymlek-Gay EA, Nicklas TA (2017) Beverage Consumption among US Children Aged 0–24 months: National Health and Nutrition Examination Survey (NHANES). Nutrients. https://doi.org/10.3390/nu9030264
Mullie P, Aerenhouts D, Clarys P (2012) Demographic, socioeconomic and nutritional determinants of daily versus non-daily sugar-sweetened and artificially sweetened beverage consumption. Eur J Clin Nutr 66(2):150–155. https://doi.org/10.1038/ejcn.2011.138
Rosinger A, Herrick K, Gahche J, Park S (2017) Sugar-sweetened beverage consumption among US adults, 2011–2014. NCHS Data Brief 270:1–8
Guelinckx I, Ferreira-Pego C, Moreno LA, Kavouras SA, Gandy J, Martinez H, Bardosono S, Abdollahi M, Nasseri E, Jarosz A, Ma G, Carmuega E, Babio N, Salas-Salvado J (2015) Intake of water and different beverages in adults across 13 countries. Eur J Nutr 54(S2):S45–S55
Guelinckx I, Iglesia I, Bottin JH, De Miguel-Etayo P, Gonzalez-Gil EM, Salas-Salvado J, Kavouras SA, Gandy J, Martinez H, Bardosono S, Abdollahi M, Nasseri E, Jarosz A, Ma G, Carmuega E, Thiebaut I, Moreno LA (2015) Intake of water and beverages of children and adolescents in 13 countries. Eur J Nutr 54(S2):69–79. https://doi.org/10.1007/s00394-015-0955-5
Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 33(11):2477–2483. https://doi.org/10.2337/dc10-1079
International Diabetes Federation (2017) Diabetes Atlas 8th Edition. http://www.diabetesatlas.org/. Accessed 25 November 2017
WHO (2017) Prevalence of diabetes in WHO South-East Asia region. Country and regional data on diabetes.. http://www.who.int/diabetes/facts/world_figures/en/index5.html. Accessed 20 December 2017
Piernas C, Ng SW, Mendez MA, Gordon-Larsen P, Popkin BM (2015) A dynamic panel model of the associations of sweetened beverage purchases with dietary quality and food-purchasing patterns. Am J Epidemiol 181(9):661–671. https://doi.org/10.1093/aje/kwu317
Ambrosini GL, Oddy WH, Huang RC, Mori TA, Beilin LJ, Jebb SA (2013) Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am J Clin Nutr 98(2):327–334 (pii: 0.3945/ajcn.112.051383)
Pan L, Li R, Park S, Galuska DA, Sherry B, Freedman DS (2014) A longitudinal analysis of sugar-sweetened beverage intake in infancy and obesity at 6 years. Pediatrics 134(Suppl 1):S29–S35. https://doi.org/10.1542/peds.2014-0646F
Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D’Agostino RB, Gaziano JM, Vasan RS (2007) Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 116(5):480–488. (CIRCULATIONAHA.107.689935)
Rachmi CN, Li M, Alison Baur L (2017) Overweight and obesity in Indonesia: prevalence and risk factors-a literature review. Public Health 147:20–29. https://doi.org/10.1016/j.puhe.2017.02.002
Ng M, Fleming T, Robinson M et al (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945):766–781. https://doi.org/10.1016/S0140-6736(14)60460-8
Soewondo P, Ferrario A, Tahapary DL (2013) Challenges in diabetes management in Indonesia: a literature review. Global Health 9:63. https://doi.org/10.1186/1744-8603-9-63
Atmarita MPHIN., Jahari AB, Permaesih D, Chan P, Amarra MS (2017) Consumption and sources of added sugar in Indonesia: a review. Asia Pac J Clin Nutr:1–25
Haning MTAA., Muqni AD (2016) The government policy relating to sugar-sweetened beverages in Indonesia. Indian J Comm Health 28(3):222–227
WHO (2017) Global Health Observatory (GHO) data: Prevalence of overweight among children and adolescents. http://www.who.int/gho/ncd/risk_factors/overweight_obesity/overweight_adolescents/en/ Accessed 29 May 2018
Acknowledgements
Participant recruitment and data collection were performed by IPSOS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CM and IG are full-time employees of Danone Research. JS-S, LAM, S.A.K, JG, HM are members of the advisory board on fluid intake for Danone Research, and have received consultancies of Danone Research. S.A.K. was a scientific consultant for Quest Diagnostics and has active research grants from Danone Research. J.S.-S. and LAM have received consultancies from Danone S.A. RP reports no conflicts of interest.
Ethical approval
All data were recorded anonymously. The protocol of the surveys was reviewed and approved by the Institutional Review Board, Office of Research Compliance of the University of Arkansas (IRB Protocol # 14-12-376).
Informed consent
All the participants gave their consent prior to the inclusion in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Laksmi, P.W., Morin, C., Gandy, J. et al. Fluid intake of children, adolescents and adults in Indonesia: results of the 2016 Liq.In7 national cross-sectional survey. Eur J Nutr 57 (Suppl 3), 89–100 (2018). https://doi.org/10.1007/s00394-018-1740-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1740-z