Abstract
Objectives
To investigate the burden of disease of myocarditis in Germany and identify similarities and differences in myocarditis with or without COVID-19.
Methods
All patients hospitalized with myocarditis in Germany were included in this nationwide retrospective analysis. Data were retrieved from the Federal Statistical Office of Germany (DESTATIS) for the years from 2007 to 2022. The primary endpoint was hospital mortality.
Results
A total of 88,159 patients hospitalized with myocarditis were analyzed. Annual cases increased from 5100 in 2007 to 6593 in 2022 (p < 0.001 for trend) with higher incidence during winter months. Incidence per 100,000 inhabitants was 6.2 in 2007 rising to 7.8 in 2022 (p < 0.001 for trend). Hospital mortality remained constant at an average of 2.44% (p = 0.164 for trend). From 2020 to 2022, 1547/16,229 (9.53%) patients were hospitalized with both, myocarditis and COVID-19 (incidence 0.62/100,000 inhabitants and 180/100,000 hospitalizations with COVID-19). These patients differed significantly in most patient characteristics and had a higher rate of hospital mortality compared to myocarditis without COVID-19 (12.54% vs. 2.26%, respectively, p < 0.001).
Conclusions
Myocarditis hospitalizations were slowly rising over the past 16 years with hospital mortality remaining unchanged. Incidence of hospitalizations with combined myocarditis and COVID-19 was low, but hospital mortality was high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incidence of myocarditis is estimated at around 1.8 million cases per year worldwide with incidences varying widely between 1 and > 10 cases/100.000 people/year [1,2,3,4,5,6]. Globally, the age-standardized incidence rate decreased over the last 30 years, while mortality remained unchanged [1]. Clinically, differentiation between myocarditis and other cardiac diseases, including coronary artery disease, can be difficult, considering similar symptoms, electrocardiography patterns, and echocardiographic findings [7]. To some extent, this may explain the varying incidences reported previously. The gold standard for confirmation of myocarditis is myocardial biopsy [8]. Current guidelines, however, suggest myocarditis to be diagnosed alternatively by magnetic resonance imaging (MRI) and elevated troponin levels, not requiring myocardial biopsy [9,10,11,12].
Most myocarditis cases in high-income countries are associated with viral agents like influenza and coronaviruses including SARS-CoV-2 [7, 13]. Of note, some cardiotropic viruses, such as Parvovirus B19 and HHV-6 (human herpesvirus 6), are not only found in myocardial biopsies in myocarditis but also in healthy individuals as “innocent bystanders” [14, 15]. Infectious agents further include bacteria, protozoa, and fungi, while systemic immune-mediated diseases (e.g., sarcoidosis) [7, 13, 16] and side effects of checkpoint inhibitors [17] or vaccinations [18] represent other rare causes. SARS-CoV-2 vaccination coincides with myocarditis only in a minority of people [18].
Ammirati et al. reported an incidence of probable or confirmed myocarditis in 240/100,000 patients hospitalized for coronavirus disease 2019 (COVID-19) and a fulminant presentation in 39% of these cases [19]. These findings are in line with similar data published during the COVID-19 pandemic in Germany [20].
In myocarditis associated with COVID-19, both direct viral tissue damage as well as a dysregulated immune response are likely to injure the myocardium [21]. Other mechanisms of tissue damage are endothelialitis and microvascular thrombosis, systemic hyperinflammation, and reduced oxygen supply [22].
Clinical courses of myocarditis include a wide range from asymptomatic inflammation with full recovery to severe courses characterized by acute cardiac failure or cardiogenic shock, severe arrhythmia, or sudden death. Some patients develop chronic cardiomyopathy with mild or severe reduced left ventricular function [7, 10]. Treatment of the underlying cause (if detected) should be combined with standard heart failure medication. Immunosuppression is not generally advised [12, 23].
The goal of our current analysis was to investigate the burden of disease of myocarditis in Germany including changes since 2020 during the COVID-19 pandemic.
Methods
Data source
Data for this research were derived from the Federal Statistical Office of Germany (German: Statistisches Bundesamt, short: DESTATIS). By German law, all reimbursement-related healthcare patient data (e.g., diagnosis-related group, DRG) are reported to DESTATIS. These data, including OPS (“Operationen- und Prozedurenschlüssel”, English: Operation and Procedure Classification System) codes used to classify various tests and treatments and ICD (International Statistical Classification of Diseases and Related Health Problems) codes, can be obtained from DESTATIS in an anonymous data package. DESTATIS blanks some data requests for small subgroups due to the potential impact of fine data granulation on anonymity. No ethics approval is needed to access and analyze anonymized DESTATIS data. Statistics on COVID-19 were derived from the Robert Koch Institute and are openly available from 2020, week 10 until 2023, week 22.
Study population
We included all patients from the DESTATIS database diagnosed with myocarditis from January 1, 2007, to December 31, 2022. Myocarditis could be coded as the main or secondary diagnosis. Cases were identified using specific ICD codes I40* (coding for acute myocarditis). There were no exclusion criteria.
Outcome measures
The primary outcome was the incidence of hospitalization with myocarditis. Secondary outcomes were hospital survival (or in-hospital mortality, as applicable), the need for mechanical circulatory support (MCS), mechanical ventilation, and length of hospital stay.
Predefined subgroups
As a predefined subgroup, the incidence of myocarditis in the context of COVID-19 (i.e., myocarditis with COVID-19) was investigated using the ICD codes (U07.1!, U07.2!, U07.3!, or U07.4!). Patients with COVID-19 were only included in this research when also coded for myocarditis.
Other patient characteristics
Myocardial biopsy and MCS were identified using the following OPS codes: myocardial biopsy (1–497.1 and 1–497.2), intra-aortic balloon pump (IABP; OPS 8-83a.0*), percutaneous ventricular assist device (pVAD/Impella®, Abiomed, Danvers, MA, USA; OPS 8-83a.3*), and veno-arterial extracorporeal membrane oxygenation (V-A ECMO; OPS 8–852.3*).
Statistical analysis
Descriptive patient data were analyzed using unpaired t-tests (assuming Gaussian distribution and similar standard deviations) for continuous variables. For categorical variables, Fisher’s exact test was used. Simple linear regression was used for the trendlines given in the figures, and the 95% confidence interval is displayed. For data on the monthly incidence of myocarditis, an adjustment for the number of days per month was computed using the formula: (“number of patients” / “days in month” / “months per year” × “days in year”). For the incidence of myocarditis per 100,000 inhabitants, the number of citizens of Germany for each year was obtained from DESTATIS. The number of COVID-19 cases per year was derived from the database of the Robert Koch Institute [24]. The significance level was set at a p-value < 0.05. Data are presented as absolute numbers and percentages for categorical variables, and continuous variables are presented as mean and standard deviation.
Results
General population
From January 1, 2007, to December 31, 2022 (i.e., 16 consecutive years), 88,159 patients were treated for myocarditis in hospital in Germany. Patients’ average age was 42 years, and 30% were female. Myocarditis was the main diagnosis of the hospital stay in 71% of these cases, and myocardial biopsies were performed in 7%. On average, hospitalizations lasted 8 days. One percent of patients received MCS. For details, see Table 1.
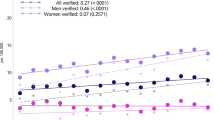
Incidence of myocarditis
Hospitalizations of patients with myocarditis increased significantly over the observed period from 5100 in 2007 to 6593 in 2022 (p < 0.001 for trend) (see Fig. 1A). This trend persisted when excluding patients with COVID-19 (see Fig. 1B). Incidence per 100,000 inhabitants increased from 6.2 in 2007 to 7.8 in 2022 (p < 0.001 for trend, see supplemental Fig. 1C). There was a consistent increase in hospitalizations during the winter months compared to summer with the highest number of hospitalizations in January (527 hospitalizations, on average) and lowest in September (407, on average) (see supplemental Fig. 1A and B). Both trends, the increase over time and the higher rate in winter persisted when adjusting for days per month and the growing number of inhabitants of Germany (see Fig. 1C and D).
Myocarditis hospitalizations. Data adjusted for days per month and inhabitants of Germany. A Total hospitalizations with myocarditis per year. Annual hospitalization increased significantly from 2007 to 2022 with a pronounced dip in 2020. B Hospitalizations of myocarditis with or without COVID-19. Since the emergence of myocarditis with COVID-19 in 2020, it occurred significantly less frequently than myocarditis without COVID-19. C Hospitalizations with myocarditis per month. Peak levels of myocarditis occur in January. D Monthly hospitalizations for COVID-19 per months and period. Numbers of myocarditis were rising over the observed period (p < 0.001)
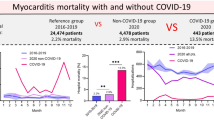
Myocarditis mortality
During the study period, 2154 patients died during hospitalization with myocarditis, resulting in an in-hospital mortality rate of 2.44% (see Fig. 2A). The in-hospital mortality rate of patients hospitalized with myocarditis remained constant over time (p = 0.164 for trend), and total numbers remained constant over time, as shown in Fig. 2B–D.
Myocarditis hospital mortality. A Mortality of hospitalizations with myocarditis per year. Hospital mortality was constantly around 2.5% between 2007 and 2022. B Hospital mortality with or without COVID-19. Myocarditis with COVID-19 showed significantly higher mortality than myocarditis without COVID-19. C Hospital mortality per period. The mortality of myocarditis without COVID-19 did not change after the emergence of COVID-19. D Number of in-hospital deaths per year. In-hospital deaths due to myocarditis did not change significantly over the investigated period (p = 0.353). Deaths with both myocarditis and COVID-19 were not significantly less than those due to myocarditis without COVID-19 in 2021 (p = 0.058)
COVID-19 statistics
From 2020 to 2022, 37,392,371 COVID-19 cases were reported in Germany. During this period, 166,621 died after SARS-CoV2 being detected. COVID-19 mortality was highest in 2020 at 2.96%, while the highest absolute number of non-survivors was recorded at 65,966 in 2021. Hospitalizations rose every year to a maximum of 448,110 in 2022. For details, see Table 2.
COVID-19 and myocarditis
Between 2020 and 2022, 1547 hospitalized patients were diagnosed with both COVID-19 and myocarditis, constituting 8.7% of all myocarditis cases during this period. Myocarditis cases with and without COVID-19 were significantly different in all baseline characteristics including the need for mechanical ventilation (p < 0.001). Significantly fewer patients with COVID-19 had myocarditis considered as the main diagnosis compared to patients without COVID-19 (48.9 vs. 73.2%, p < 0.001). Both V-A ECMO and PVAD were used significantly more often in patients with both, COVID-19 and myocarditis, compared to those with myocarditis alone (both p < 0.001) (see Table 1). Hospital mortality rate was significantly higher in patients with both, COVID-19 and myocarditis, compared to those with myocarditis alone (12.5% versus 2.3% respectively, p < 0.001) (see Fig. 2B and C).
Discussion
Current data from DESTATIS show a significant rise in myocarditis hospitalizations in recent years up to 6593 cases in 2022. Incidence was 6.2/100,000 inhabitants in 2007 and 7.8/100,000 in 2022 following a seasonal pattern.
This is lower than the incidence in the USA averaging 10–14/100,000 [25]. Importantly, only 7% of patients in our dataset received cardiac biopsies considering the recommendations of the European Society of Cardiology [26]. The low utilization of myocardial biopsy is in accordance to recommendations in low-risk patients [27]. There are data suggesting a rise in MRI-facilitated myocarditis diagnosis in recent years [25]. Although we cannot exclude an under-reporting in our dataset, hospital mortality in the USA and in our dataset is similar [28]. This makes it unlikely that severe cases are missed in the current research.
Influenza being a known infectious agent in myocarditis [13] strongly corresponds to the highest rates of myocarditis hospitalizations in January and February during the flu season in the northern hemisphere. A causal link between flu and myocarditis hospitalizations however cannot be drawn from our dataset, while the gender gap of men suffering from myocarditis significantly more often than women is well established [29]. Sex hormones may play a role in this pronounced gender gap [30].
Since 2020, a subset of about 1500 patients was hospitalized with both, COVID-19 and myocarditis. The incidence of hospitalizations with myocarditis and COVID-19 in our dataset was 180/100,000 hospitalizations with COVID-19, comparable to the rate of 146–240/100,000 individuals seen in other registries [19, 31]. The low incidence of myocarditis hospitalizations in 2020 might be explained by an underutilization of the healthcare system during the COVID-19 pandemic [32,33,34,35]. Since our first analysis of myocarditis in 2020 [20], SARS-CoV-2 variants developed from Alpha to Omicron [6, 36,37,38,39]. Dominant variants switched regularly [40] as did outcome parameters of COVID-19 including case fatality rate (highest 2020), mortality (highest 2021), and infections (highest 2022). If and how virus variants influence myocarditis is unknown.
Patients hospitalized with both, COVID-19 and myocarditis, had a significantly higher hospital mortality rate of 12.5% compared to 2.3% in hospitalizations with myocarditis without COVID-19. As the combination of hospitalization for myocarditis and COVID-19 without respiratory failure seems to be a rare occurrence [41,42,43], it is tempting to speculate on cofactors such as acute respiratory distress syndrome (ARDS) being the main driver of mortality [44, 45] in myocarditis with COVID-19. ARDS does not only impair gas exchange, but also increases right ventricular afterload [46, 47], which might be especially detrimental in case of myocarditis. Since the cohorts of myocarditis with and without COVID-19 also differed significantly in several important characteristics including age and comorbidities, ARDS however might not be the only driver of mortality in myocarditis with COVID-19.
Limitations
Data presented derives from the Federal Statistical Office of Germany (DESTATIS). Data on non-reimbursement-relevant comorbidities is likely to be underreported and therefore not included in the current investigation. Data from clinical investigations like transthoracic echocardiogram, MRI, myocardial biopsies, or laboratory tests are not included in the DESTATIS dataset. The exact cause of death cannot be derived from the dataset. Also, the diagnosis of myocarditis could not be reviewed independently.
Conclusion
Overall numbers of hospitalization for myocarditis rose from 2007 to 2022, while mortality remained low. A minority of patients were hospitalized with both, COVID-19 and myocarditis. This distinct subgroup had different patient characteristics and a higher hospital mortality rate.
Data Availability
All data is publicly available from DESTATIS and the RKI.
References
Wang Y-W-Y, Liu R-B, Huang C-Y, Li H-Y, Zhang Z-X, Li X-Z et al (2023) Global regional and national burdens of myocarditis 1990–2019: systematic analysis from GBD 2019. BMC Public Health 23(1):714
Golpour A, Patriki D, Hanson PJ, McManus B, Heidecker B (2021) Epidemiological impact of myocarditis. J Clin Med 10:603
Ba H, Zhang D, Guan S, Zheng J (2023) Global burden of myocarditis and cardiomyopathy in children and prediction for 2035 based on the global burden of disease study 2019. Frontiers in Cardiovascular Medicine [Internet]. [cited 2024 Mar 3]. 10. Available from: https://www.frontiersin.org/articles/. https://doi.org/10.3389/fcvm.2023.1173015
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M et al (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396:1204–1222
Heymans S, Cooper LT (2022) Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol 19:75–77
Fairweather D, Beetler DJ, Di Florio DN, Musigk N, Heidecker B, Cooper LT (2023) COVID-19, myocarditis and pericarditis. Circ Res 132:1302–1319
Sagar S, Liu PP, Cooper LT (2012) Myocarditis. The Lancet 379:738–747
Thomas AH (1987) Myocarditis: the Dallas criteria. Hum Pathol 18:619–624
Cooper LT (2009) Myocarditis. N Engl J Med 360:1526–1538
Basso C (2022) Myocarditis. N Engl J Med 387:1488–1500
Gargano JW (2021) Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the Advisory Committee on Immunization Practices — United States. MMWR Morb Mortal Wkly Rep [Internet]. 2021 [cited 2024 Mar 3];70. Available from: https://www.cdc.gov/mmwr/volumes/70/wr/mm7027e2.htm
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M et al (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42:3599–3726
Tschöpe C, Ammirati E, Bozkurt B, Caforio ALP, Cooper LT, Felix SB et al (2021) Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol 18:169–193
Elsanhoury A, Kühl U, Stautner B, Klein O, Krannich A, Morris D et al (2022) The spontaneous course of human herpesvirus 6 DNA-associated myocarditis and the effect of immunosuppressive intervention. Viruses 14:299
Bock C-T, Klingel K, Kandolf R (2010) Human parvovirus B19–associated myocarditis. N Engl J Med 362:1248–1249
Caforio ALP, Adler Y, Agostini C, Allanore Y, Anastasakis A, Arad M et al (2017) Diagnosis and management of myocardial involvement in systemic immune-mediated diseases: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Disease. Eur Heart J 38:2649–2662
Hu J-R, Florido R, Lipson EJ, Naidoo J, Ardehali R, Tocchetti CG et al (2019) Cardiovascular toxicities associated with immune checkpoint inhibitors. Cardiovasc Res 115:854–868
Block JP (2022) Cardiac complications after saRS-CoV-2 infection and mRNA COVID-19 vaccination — PCORnet, United States, January 2021–January 2022. MMWR Morb Mortal Wkly Rep [Internet]. [cited 2024 Mar 3];71. Available from: https://www.cdc.gov/mmwr/volumes/71/wr/mm7114e1.htm
Ammirati E, Lupi L, Palazzini M, Hendren NS, Grodin JL, Cannistraci CV et al (2022) Prevalence, characteristics, and outcomes of COVID-19-associated acute myocarditis. Circulation 145:1123–1139
Bemtgen X, Kaier K, Rilinger J, Rottmann F, Supady A, von ZurMühlen C et al (2024) Myocarditis mortality with and without COVID-19: insights from a national registry. Clin Res Cardiol 113:216–222
Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY et al (2020) Recognizing COVID-19–related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 17:1463–1471
Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, Aubry M-C et al (2020) Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J 41:3827–3835
Maron BJ, Udelson JE, Bonow RO, Nishimura RA, Ackerman MJ, Estes NAM et al (2015) Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis. Circulation 132:e273–e280
RKI - Coronavirus SARS-CoV-2 (n.d.) COVID-19-Fälle nach Meldewoche und Geschlecht sowie Anteile mit für COVID-19 relevanten Symptomen, Anteile Hospitalisierter/Verstorbener und Altersmittelwert/-median [Internet]. [cited 2024 Mar 6]. Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Klinische_Aspekte.html
Pahuja M, Adegbala O, Mishra T, Akintoye E, Chehab O, Mony S et al (2019) Trends in the incidence of in-hospital mortality, cardiogenic shock, and utilization of mechanical circulatory support devices in myocarditis (analysis of national inpatient sample data, 2005–2014). J Cardiac Fail 25:457–467
Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB et al (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 34:2636–2648
Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M et al (2020) Management of acute myocarditis and chronic inflammatory cardiomyopathy. Circ Heart Fail 13(11):e007405
Shah Z, Mohammed M, Vuddanda V, Ansari MW, Masoomi R, Gupta K (2019) National trends, gender, management, and outcomes of patients hospitalized for myocarditis. Am J Cardiol 124:131–136
Kytö V, Sipilä J, Rautava P (2013) The effects of gender and age on occurrence of clinically suspected myocarditis in adulthood. Heart 99:1681–1684
Fairweather D, Cooper LT, Blauwet LA (2013) Sex and gender differences in myocarditis and dilated cardiomyopathy. Curr Probl Cardiol 38:7–46
Boehmer TK (2021) Association between COVID-19 and myocarditis using hospital-based administrative data — United States, March 2020–January 2021. MMWR Morb Mortal Wkly Rep [Internet]. [cited 2024 Mar 8];70. Available from: https://www.cdc.gov/mmwr/volumes/70/wr/mm7035e5.htm
Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW (2021) Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol 77:159–169
Seiffert M, Brunner FJ, Remmel M, Thomalla G, Marschall U, L’Hoest H et al (2020) Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: an analysis of health insurance claims. Clin Res Cardiol 109:1540–1548
Settelmeier S, Rassaf T, Giannitsis E, Münzel T, Breuckmann F (2020) Capacity changes in German certified chest pain units during COVID-19 outbreak response. Clin Res Cardiol 109:1469–1475
De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A et al (2020) Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med 383:88–89
Stein C, Nassereldine H, Sorensen RJD, Amlag JO, Bisignano C, Byrne S et al (2023) Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis. The Lancet 401:833–842
Hillary VE, Ceasar SA (2023) An update on COVID-19: SARS-CoV-2 variants, antiviral drugs, and vaccines. Heliyon 9:e13952
CDC (2023) CDC Museum COVID-19 timeline [Internet].Centers for Disease Control and Prevention. [cited 2024 Mar 6]. Available from: https://www.cdc.gov/museum/timeline/covid19.html
Coronavirus Disease (COVID-19) (n.d.) Situation reports [Internet]. [cited 2024 Mar 6]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
Gong W, Parkkila S, Wu X, Aspatwar A (2023) SARS-CoV-2 variants and COVID-19 vaccines: current challenges and future strategies. Int Rev Immunol 42:393–414
Atif Masood Noori M, Rushdy A, Fichadiya H, Sherif R, Younes I, Lenchur PD et al (2021) Stemi mimicking post COVID: a case of focal myopericarditis post COVID infection. J Community Hosp Intern Med Perspect. 11:769–771
Gaine S, Devitt P, Coughlan JJ, Pearson I (2021) COVID-19-associated myocarditis presenting as new-onset heart failure and atrial fibrillation. BMJ Case Reports CP 14:e244027
Du H, Du Z, Wang L, Wang H, Jia M, Zhang C et al (2024) Fulminant myocarditis induced by SARS-CoV-2 infection without severe lung involvement: insights into COVID-19 pathogenesis. Journal of Genetics and Genomics [Internet]. [cited 2024 Apr 10]; Available from: https://www.sciencedirect.com/science/article/pii/S1673852724000365
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720
Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G et al (2020) A new coronavirus associated with human respiratory disease in China. Nature 579:265–269
Dandel M (2022) Heart–lung interactions in COVID-19: prognostic impact and usefulness of bedside echocardiography for monitoring of the right ventricle involvement. Heart Fail Rev 27:1325–1339
Wei Z-Y, Geng Y-J, Huang J, Qian H-Y (2020) Pathogenesis and management of myocardial injury in coronavirus disease 2019. Eur J Heart Fail 22:1994–2006
Acknowledgements
We acknowledge support by the Open Access Publication Fund of the University of Freiburg.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAR, CG, KK, CM, and DW declare no conflicts of interest. XB reports lecture fees from Amomed and AstraZeneca. AS declares a research grant, lecture honoraria and travel support from CytoSorbents Europe, lecture honoraria from AstraZeneca and Getinge, and travel support from Artcline. TW received lecture honoraria or travel support from Abbot Medical, AstraZeneca, and Boston Scientific. DLS received lecture honoraria or travel support from Abiomed, AstraZeneca, Dahlhausen, Getinge, Medtronic, and Orion Pharma and was part of a dual lumen advisory board by Medtronic.
Supplementary Information
Below is the link to the electronic supplementary material.
392_2024_2494_MOESM1_ESM.docx
Supplementary file1 Supplementary figure 1: Myocarditis hospitalizations. Data not adjusted for days per month and inhabitants of Germany. A: Hospitalizations with myocarditis per month. Peak levels of myocarditis occur in January. B: Monthly hospitalizations for COVID-19 per months and period. Numbers of myocarditis were rising over the observed period (p<0.001). C: Hospitalizations per 100,000 inhabitants and year. Numbers were rising significantly in the investigated time frame (p<0.001).(DOCX 221 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rottmann, F.A., Glück, C., Kaier, K. et al. Myocarditis incidence and hospital mortality from 2007 to 2022: insights from a nationwide registry. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02494-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02494-3