Abstract
Objectives
Systemic inflammatory response syndrome (SIRS) is a common finding after cardiovascular interventions. Data on the incidence of SIRS and its impact on outcome in patients undergoing transcatheter edge-to-edge mitral valve repair (MV-TEER) for mitral regurgitation (MR) is lacking.
Methods
From January 2013 to December 2020, 373 patients with moderate or severe MR undergoing MV-TEER were included. SIRS was defined as at least two of the following criteria within 48 h after the procedure: leucocyte count > 12.0 or < 4.0 × 109/l, respiratory rate > 20 breaths per minute or PaCO2 ≤ 4.3 kPa/32 mmHg, heart rate > 90 bpm and temperature > 38.0 °C or < 36.0 °C. The primary endpoint was 3-years all-cause mortality.
Results
SIRS was observed in 49.6% (185/373) of patients. Patients who developed SIRS presented more frequently with NYHA III/IV at baseline [SIRS: 82.4% (149/185) vs. no SIRS: 79.0% (147/188); p = 0.029]. Patients who developed SIRS spent more days on ICU (p < 0.001) and overall length of stay was longer (p < 0.001). Relevant residual MR, defined as MR ≥ III in-hospital, was present more often in patients who developed SIRS [SIRS: 11.3% (20/177) vs. no SIRS: 3.93% (7/178), p = 0.036]. At 3 years, all-cause mortality in the entire population was 33.5% (125/373) with an increased all-cause mortality in patients with SIRS compared to patients without SIRS (HR 1.49, [CI 95% 1.04, 2.13]; p = 0.0264). In the multivariate analysis development of SIRS (HR 1.479 [CI 95% 1.016, 2.154]; p = 0.041) was identified as predictor for 3-years all-cause mortality.
Conclusions
SIRS is a common finding after MV-TEER occurring in approximately half of patients. SIRS after MV-TEER was associated with a longer in-hospital stay. In addition, we observed an increased 3-years all-cause mortality in patients with SIRS.
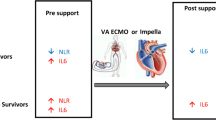
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, transcatheter edge-to-edge mitral valve repair (MV-TEER) has become an established therapeutic strategy for patients with severe, symptomatic mitral valve regurgitation (MR) who are at high or prohibitive risk for surgery [1]. In the context of demographic challenges with a growing number of elderly patients, the amount of MV-TEER procedures is expected to rise even further in the upcoming years [2]. Therefore, the identification of potential periprocedural risk factors and their adequate treatment is crucial to warrant optimal patient management.
The activation of a systemic inflammatory response has been reported in patients after myocardial infarction or coronary artery bypass grafting (CABG) [3,4,5]. Especially cardiac surgery induces a systemic inflammatory reaction, associated with increased postoperative mortality and morbidity [6, 7]. Squiccimarro et al. observed an incidence of systemic inflammatory response syndrome (SIRS) of 28.3% within 24 h in patients undergoing cardiovascular surgery (including CABG, aortic-, mitral-, and tricuspid valve surgery, surgery of the thoracic aorta, correction of atrial septal defect and ventricular defect or resection of cardiac tumor). In this cohort, SIRS was associated with a more complicated postoperative course and higher postoperative morbidity [7]. In addition, recent studies found that the incidence of SIRS after transcatheter aortic valve implantation (TAVI) was even higher, reaching approximately 40% [8, 9]. Thereby, Sinning et al. showed an increased 1-year mortality in patients who developed SIRS after TAVI, even after excluding patients with periprocedural complications such as major vascular or bleeding complications, and kidney injury [8]. Similar results were observed by Schwietz et al. showing that SIRS was associated with an increased 1-year mortality, but not 30-day mortality [9]. These observations suggest that the adverse outcome of patients with SIRS after TAVI may not be necessarily derived by hospital-associated infections or procedure-related complications.
However, in daily clinical practice, the treating physician is often confronted with the occurrence of postprocedural SIRS without knowing the relevance for the patient and his clinical outcome. Especially, in multimorbid patients undergoing MV-TEER standardized data on the incidence of SIRS and its impact on mortality do not exist so far. Therefore, the present study sought to evaluate the incidence of SIRS and potential prognostic implications of its occurrence in patients undergoing MV-TEER due to severe, symptomatic MR.
Patients and methods
Patient population and procedures
All consecutive patients undergoing MV-TEER between January 2013 and December 2020 at the Deutsches Herzzentrum München, Germany, were evaluated for the present retrospective analysis.
In all cases, the indication for MV-TEER was symptomatic moderate-to-severe or severe MR and all procedures were approved by the local heart team. Patient informed consent was obtained prior to each procedure. MV-TEER was performed under general anesthesia and transoesophageal echocardiographic guidance through a transvenous, transseptal approach as previously described [10]. The number of devices implanted was at the discretion of the treating physician. All patients received prophylactic periprocedural antibiotic therapy with a second generation cephalosporin. After the procedure, patients were monitored at the intensive care unit (ICU) for at least 12 h and then transferred to the cardiology ward, remaining under observation for at least 72 h. Clinical, procedural and follow-up data were collected according to a standardized protocol and entered in a central electronic database.
The study was conducted in conformity with the Declaration of Helsinki and the collection of clinical, procedural and follow-up patient data was approved by the local ethics committee.
Echocardiographic analysis
All echocardiographic studies were performed by experienced institutional cardiologists during clinical routine. Echocardiographic measures were assessed according to the current guideline recommendations [11], and classification of MR severity was performed using a four-group classification (mild≙I°, moderate≙II°, severe≙III°, and massive≙IV°). All patients underwent transthoracic as well as transoesophageal echocardiography before MV-TEER and transthoracic echocardiography after MV-TEER in hospital. Relevant residual MR post procedure was defined as MR ≥ III°.
Endpoint definition and clinical follow-up
SIRS was defined according to the joint definition of the American College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) Consensus Conference, through the fulfillment of at least two of the following four criteria: leucocyte count > 12.0 or < 4.0 × 109/l, respiratory rate > 20 breaths per minute or PaCO2 ≤ 4.3 kPa/32 mmHg, heart rate > 90 beats per minute and temperature > 38.0 °C or < 36.0 °C within 48 h after the procedure [12, 13]. Clinical follow-up including transthoracic echocardiography was routinely performed 30 days and 1 year after MV-TEER. Procedural success was measured after 30 days and was defined according to the definition of the Mitral Valve Academic Research Consortium (MVARC) including the absence of a relevant residual MR [14]. As an elderly patient population was studied, post-procedural 3-years all-cause mortality was defined as a clinically meaningful primary outcome measure. Survival data were obtained from the German Civil Registry, meaning that no patient was lost to follow-up.
Laboratory methods
Blood samples were obtained pre-procedurally, the same day after the procedure, after 48 h, after 96 h and at discharge, as part of clinical routine. Leucocyte count was measured using fluorescence flow cytometry (Sysmex XN-2000, Kobe, Japan), C-reactive protein (CRP) levels were determined using immunturbidimetry (Cobas c501 Roche, Mannheim, Germany) and lactate dehydrogenase (LDH) levels were assessed using photometry (Cobas c501 Roche, Mannheim, Germany).
Statistical analysis
Continuous variables are reported as mean ± standard deviation (SD) or median [interquartile range], according to the distribution pattern of the variable, and compared using the Student’s t test or the Mann–Whitney U test as appropriate. Categorical variables are described as frequencies or proportions and compared using the Pearson χ2 test (or Fischer’s exact test where any expected cell count of the contingency table was < 5). Event-free survival was estimated by the Kaplan–Meier method and hazard ratios (HR) with two-sided 95% confidence intervals (95% CI) were calculated using the Cox proportional hazards model. A logistic regression computing the odds ratios (OR) with 95% CIs was performed to identify predictors of SIRS. Independent mortality predictors were analyzed by means of multivariable Cox proportional hazards models.
The selection of variables to be included in the multivariable models for mortality at 3 years as well as for SIRS occurrence was performed using the LASSO (Least Absolute Shrinkage and Selection Operator) regression method [15], after entering all relevant clinical, echocardiographic and laboratory parameters as well as relevant medications as candidates.
A 2-sided p value of < 0.05 was considered statistically significant for all analyses. Statistical analysis was performed using the R 4.10 Statistical Package (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient population
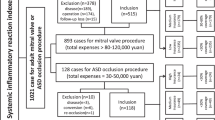
A total of 477 consecutive patients underwent MV-TEER at the Deutsches Herzzentrum München, Germany, between January 2013 and December 2020. Of these, patients with conversion to open heart surgery (n = 2), periprocedural death (n = 1), leucocytosis or leucopenia at admission (n = 65), active cancer (n = 20) and insufficient data to apply SIRS definition (n = 16) were excluded, resulting in a final study population of 373 patients. A detailed flow chart with exclusion criteria is depicted in Fig. 1.
Table 1 shows baseline characteristics of the patient population according to the presence/absence of SIRS. Overall, mean age was 79.0 years [interquartile range [IQR] 73.0, 82.0], 42.9% (160/373) were female and median logistic EuroSCORE I was 13.9% [IQR 8.9, 22.2]. Patients who developed SIRS presented more frequently with NYHA class III/IV (SIRS: 82.4% (149/185), no SIRS: 79% (147/188); p = 0.029) and less frequently with previous coronary artery disease (CAD) (SIRS: 60.0% (111/185), no SIRS: 70.7% (133/188); p = 0.038). Interventricular septum diameter (IVSD) was smaller in patients who developed SIRS (SIRS: 11.0 mm [9.53, 12.0], no SIRS: 11.0 mm [10.0, 13.0]; p = 0.025) with a trend towards a reduced left and right ventricular function.
Incidence of systemic inflammation response syndrome after transcatheter edge-to-edge mitral valve repair
Overall, the incidence of SIRS after transcatheter edge-to-edge mitral valve repair was 49.6% (185/373). The four different drivers of SIRS definition are shown in Fig. 2.
Inflammatory biomarkers following MV-TEER
The time course of inflammatory biomarkers of interest at admission as well as following MV-TEER are depicted in Fig. 3. Inflammatory biomarkers increased after the procedure, irrespective of SIRS development: leucocyte count increased in both groups after MV-TEER, however this effect was more pronounced in patients which experienced SIRS (leucocyte count at 48 h in patients with SIRS: 8.79 × 109/l [7.26, 10.5] vs. no SIRS: 7.50 × 109/l [6.64, 8.70]; p < 0.001) (Fig. 3a). A similar effect was observed regarding the increase in CRP levels (CRP count at 48 h in patients with SIRS: 32.8 mg/dl [19.1, 45.1], no SIRS: 27.7 mg/dl [11.7, 41.7]; p = 0.041) (Fig. 3b). In contrast, LDH levels did not differ significantly (LDH count at 48 h in SIRS: 208 U/l [178, 263], no SIRS: 219 U/l [189, 258]; p = 0.357) (Fig. 3c).
Impact of SIRS on clinical outcome
Procedural characteristics and in-hospital complications are shown in Table 2. Relevant residual MR after MV-TEER was present more often in patients developing SIRS versus patients without SIRS (SIRS 11.30% (20/177) vs. no SIRS: 3.93% (7/178), p = 0.036). Patients with SIRS after MV-TEER spent more days on ICU (SIRS: 1.00 [1.00, 2.00] days vs. no SIRS: 1.00 [1.00, 1.00] days; p < 0.001) and had an overall longer length of stay than patients who did not develop SIRS (SIRS: 3.00 [3.00, 5.00] days vs. no SIRS group: 3.00 [3.00, 4.00] days; p < 0.001). Differences in length of stay and days on ICU remained significant despite dividing the number of days into smaller subgroups (Table 2). Interestingly, relevant residual MR, defined as MR ≥ III in-hospital, was present more often in patients who developed SIRS (SIRS 11.30% (20/177) vs. no SIRS: 3.93% (7/1178), p = 0.036). In addition, patients with SIRS had required red blood cell (RBC) transfusions more frequently (SIRS: 9.44% (17/180) vs. no SIRS: 2.69% (5/186; p = 0.012).
Regarding procedural success at 30 days there was no significant difference between patients with SIRS (70.8%; 119/168) and patients without SIRS (79.2%; 137/173), p = 0.097). Functional recovery of patients after MV-TEER showed numerically more patients with NYHA Class ≥ III at 30 days in the SIRS group (30.4%; 45/148) versus 21.6% (33/153) in the no SIRS group, yet without reaching statistical significance (p = 0.255), (Table 3). Further, NYHA Class ≥ III at 1 year was 35.0% in the SIRS group (36/103) and 28.4% in the no SIRS group (35/123); (p = 0.459). Interestingly, in the multivariate analysis a higher left ventricular ejection fraction at baseline showed a lower risk of SIRS occurrence (OR 0.977 [95% CI: 0.958, 0.977]; p = 0.030), (Table 4).
Overall, all-cause mortality at 3 years was 33.5% (125/373) in the study population. We observed a significantly higher 3-year mortality in patients who developed SIRS after MV-TEER (HR 1.49, [95% CI: 1.04, 2.13]; p = 0.0264) compared to patients who did not develop SIRS (SIRS: 38.9% (72/185) vs. SIRS: 28.2% (53/188); p = 0.03) (Fig. 4).
When analyzed in a multivariable cox regression analysis, the development of SIRS (HR 1.479 [95% CI 1.016, 2.154]; p = 0.041), previous stroke/TIA (HR 1.342 [95% CI 1.023, 1.760]; p = 0.033) and use of diuretics (HR 3.990 [95% CI 1.228, 12.965]; p = 0.021) were identified as independent risk factors for 3-years all-cause mortality (Table 5). Increased eGFR (HR 0.973 [95% CI 0.959, 0.987]; p = 0.0001), hemoglobin (HR 0.758 [95% CI 0.667, 0.860]; p < 0.0001), ejection fraction (HR 0.979 [95% CI 0.963, 0.996]; p = 0.016) and concomitant CAD (HR 0.591 [95% CI 0.394, 0.887]; p = 0.011) showed a lower risk for 3-years all-cause mortality.
Discussion
This retrospective study is the first systematic analysis of the incidence of SIRS in patients undergoing MV-TEER. We found that the incidence of SIRS within 48 h after MV-TEER was high, affecting approximately half of the patients. Inflammatory markers increased in all groups irrespective of SIRS, but were significantly higher in patients with SIRS. The development of SIRS after MV-TEER occurred more often in patients with relevant residual MR and was associated with a prolonged in-hospital stay. Furthermore, we observed an increased all-cause mortality at 3 years in patients with postprocedural SIRS.
Potential mechanisms of systemic inflammatory response syndrome
SIRS is a common clinical finding in patients undergoing cardiac surgery [16, 17]. Procedure-related organ hypoperfusion leading to regional ischemia followed by reperfusion is a known trigger for the release of immune mediators and has been described as contributor in SIRS development after CABG [18]. Furthermore, the surgical trauma during CABG might also stimulate the immune response [3, 18, 19]. Similar, SIRS is known to occur in patients after myocardial infarction and comparably to the ischemia–reperfusion-triggered cytokine release in CABG, concentrations of inflammatory cytokines correlate with the blood flow through the infarct-related artery [20]. Additionally, SIRS has also been observed in patients after TAVI [8, 9, 21]. Possible pathomechanisms were reported to be suboptimal organ perfusion caused by transient drop in total or regional blood flow with consecutive hypotension during rapid pacing, valve deployment, post-dilatation as well as vascular complications and/or major bleeding events [8]. In our study there was no difference between patients with and without SIRS regarding the procedural time, which can be used as indicator for procedure-related ischemia. Also, periprocedural complications including vascular complications and major bleedings were similar between patients with and without SIRS. However, RBC transfusion rates were higher in patients who developed SIRS. RBC transfusion can cause the co-administration of e.g. interleukin (IL)-8 which accumulates in stored RBC packages and can contribute to the development of pyrexia and leucocytosis [8, 22].
Furthermore, emerging hypotheses suggest a shear-stress induced development of SIRS in patients after TAVI. Underlying considerations are based on the anatomy of the aortic valve leaflet, composed of two different cell types, an interstitial layer of fibroblast-like cells named valve interstitial cells (VICs), and two outer-layers of valve endothelial cells (VECs) [23]. By tissue damage, e.g. through TAVI procedure-related dilatation of the aortic annulus, VICs become activated to myofibroblasts, thus leading to the production and secretion of a number of cytokines within tissue repair [24, 25], contributing to the development of SIRS. However, the impact of periprocedural-induced shear stress with regard to clinical outcomes remains a matter of debate and needs to be investigated in further studies.
Systemic inflammatory response syndrome in transcatheter edge-to-edge mitral valve repair
So far, SIRS has not been investigated in patients undergoing MV-TEER. Applying the current knowledge of SIRS development to an edge-to edge repair of the mitral valve, a potential procedure-related trigger for SIRS could be the grasping of the mitral valve leaflets. This step during MV-TEER followed by the closing of the transcatheter device causes a significant mechanical stress on the mitral valve leaflets and its apparatus and could be a pendant to the aortic stretch during TAVI.
Another important aspect to consider is that MV-TEER cohorts typically comprise mainly old and multimorbid patients. Nowadays, the elderly population (> 65 years old) in Europe represents 19.7% of the population and is expected to reach 28.5% in 2050 [26]. Biologically, aging is associated with a physiological process of tissue degeneration related to chronic inflammation [27]. This mechanism of age-related chronic inflammation is called “inflammaging”, which was initially defined as progressive increase of proinflammation in aged organisms [28], leading to increased morbidity and mortality [29,30,31,32]. Despite lacking evidence on the direct interaction between “inflammaging” and the development of postprocedural SIRS, “inflammaging” may represent an additional risk factor in elderly, multimorbid patients. In our cohort, we observed an increase of serum inflammatory markers (CRP, leucocytes) in both, the SIRS group and no SIRS group; however, this effect was more pronounced in the SIRS group.
Besides the above-mentioned mechanisms, a further possible contribution to the development of SIRS might be the standard performance of general anesthesia (GA) in an elderly, already frail patient collective. GA is reported to increase stress hormone release by its invasive character, thus accelerating inflammatory processes [21]. However, a recent meta-analysis, including four studies comparing GA with deep sedation (DS) after MV-TEER, showed no difference regarding the composite endpoint of all-cause death, stroke, pneumonia or major to life-threatening bleeding between patients treated with DS as compared to GA, while ICU stay was longer after GA compared to DS [33].
In addition, anaesthesiologic monitoring in patients undergoing MV-TEER is challenging as patients usually are hypovolemic due to a continuous diuretic therapy. Nearly all commonly used anesthetic agents which are used for general anesthesia for MV-TEER procedure lead to vasodilatation resulting in hypotension which has to be treated with a vasopressor. Thereby, increased systemic vascular resistance can increase MV regurgitation, resulting in mandatory inotropic support in patients with a reduced left-ventricular ejection fraction, to counteract the hemodynamic results of a reduced MV-regurgitation after MV-TEER. Interestingly, in our study residual MR was associated with SIRS whereas patients with a higher ejection fraction showed a lower risk for developing SIRS. Thus, the hemodynamic state of the patient during the procedure may be a relevant factor in SIRS development after MV-TEER [34, 35].
Incidence of systemic inflammatory response syndrome and its impact on patient outcome
The occurrence of SIRS after various cardiac interventions, including CABG and TAVI, has been previously described with high incidences of up to 40% [7,8,9]. In our study, we found an even higher incidence of SIRS after MV-TEER, in nearly half of the patients (49.6%). This might be second to differences regarding the standard patient collectives assessed for the respective procedures: While TAVI is increasingly performed in younger patients with intermediate or even low surgical risk [36, 37], patients assessed for MV-TEER are usually multimorbid with high or prohibitive surgical risk [1].
Despite the finding of a high SIRS incidence after MV-TEER, we additionally observed that patients who developed SIRS had a prolonged stay on intensive care unit and overall, a longer in-hospital stay. Further, we observed that development of SIRS after MV-TEER increases 3-years all-cause mortality, which was high, at 33.5% and is in line with previous studies such as the COAPT trial, which showed a mortality of 32.7% at 2 years [38]. Interestingly, we found that CAD was associated with a lower risk of 3-years all-cause mortality in our cohort. Although only speculative, one explanation for this finding may be that patients with CAD develop relevant MR due to regional wall motion abnormalities and not due to a global reduced left ventricular ejection fraction as for example seen in advanced stages of dilated cardiomyopathy. In addition, use of diuretics was a strong predictor of mortality pointing to advanced stages of MR and congestive heart failure. In accordance with this, higher eGFR, hemoglobin and increased left ventricular ejection fraction were predictors of a reduced 3-years mortality.
Furthermore, we found SIRS to be a predictor for all-cause mortality after 3 years. However, these results have to be interpretated carefully and further studies are necessary to better characterize patients that develop SIRS and also to provide further insight into the underlying pathomechanism.
Limitations
All limitations inherent to retrospective data analysis also apply to our study. Especially, causality between the development of SIRS and clinical outcome cannot be established from such analysis and requires prospectively designed randomized trials. In particular, a potential influence of periprocedural catecholamine administration and ventilation time on the development of SIRS cannot be excluded. Furthermore, adding an external cohort would have improved our analysis by increasing the sample size. In addition, we analysed a cohort of multimorbid and old patients and therefore the results cannot be extrapolated to a younger, healthier cohort. However, given the globally growing numbers of MV-TEER procedures and transcatheter valve interventions in general, further investigations addressing causes and pathomechanisms of SIRS are needed in order to derive preventive and therapeutic consequences to optimize periprocedural management of patients at risk.
Conclusion
SIRS development is a common finding in patients undergoing MV-TEER for MR and is associated with a prolonged in-hospital stay. SIRS development after MV-TEER suggests an adverse impact on patient outcome, however the underlying pathomechanims have to be evaluated further to allow optimized patient management.
Data availability
Data available on request.
Abbreviations
- CRP:
-
C-reactive protein
- LDH:
-
Lactate dehydrogenase
- MR:
-
Mitral valve regurgitation
- MV-TEER:
-
Transcatheter edge-to-edge mitral valve repair
- SIRS:
-
Systemic inflammatory response syndrome
References
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP III, Gentile F et al (2021) 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: a Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143(5):e72–e227. https://doi.org/10.1161/cir.0000000000000923
Nita N, Schneider L, Dahme T, Markovic S, Keßler M, Rottbauer W et al (2022) Trends in transcatheter edge-to-edge mitral valve repair over a decade: data from the MiTra ULM Registry. Front Cardiovasc Med 9:850356. https://doi.org/10.3389/fcvm.2022.850356
Diegeler A, Doll N, Rauch T, Haberer D, Walther T, Falk V et al (2000) Humoral immune response during coronary artery bypass grafting: a comparison of limited approach, “off-pump” technique, and conventional cardiopulmonary bypass. Circulation 102(19 Suppl 3):Iii95–Iii100. https://doi.org/10.1161/01.cir.102.suppl_3.iii-95
Hirai S (2003) Systemic inflammatory response syndrome after cardiac surgery under cardiopulmonary bypass. Ann Thorac Cardiovasc Surg 9(6):365–370
Kohsaka S, Menon V, Lowe AM, Lange M, Dzavik V, Sleeper LA et al (2005) Systemic inflammatory response syndrome after acute myocardial infarction complicated by cardiogenic shock. Arch Intern Med 165(14):1643–1650. https://doi.org/10.1001/archinte.165.14.1643
Paparella D, Yau TM, Young E (2002) Cardiopulmonary bypass induced inflammation: pathophysiology and treatment. An update. Eur J Cardiothorac Surg 21(2):232–244. https://doi.org/10.1016/s1010-7940(01)01099-5
Squiccimarro E, Labriola C, Malvindi PG, Margari V, Guida P, Visicchio G et al (2019) Prevalence and clinical impact of systemic inflammatory reaction after cardiac surgery. J Cardiothorac Vasc Anesth 33(6):1682–1690. https://doi.org/10.1053/j.jvca.2019.01.043
Sinning JM, Scheer AC, Adenauer V, Ghanem A, Hammerstingl C, Schueler R et al (2012) Systemic inflammatory response syndrome predicts increased mortality in patients after transcatheter aortic valve implantation. Eur Heart J 33(12):1459–1468. https://doi.org/10.1093/eurheartj/ehs002
Schwietz T, Behjati S, Gafoor S, Seeger F, Doss M, Sievert H et al (2015) Occurrence and prognostic impact of systemic inflammatory response syndrome in transfemoral and transapical aortic valve implantation with balloon- and self-expandable valves. EuroIntervention 10(12):1468–1473. https://doi.org/10.4244/EIJY14M06_05
Feldman T, Wasserman HS, Herrmann HC, Gray W, Block PC, Whitlow P et al (2005) Percutaneous mitral valve repair using the edge-to-edge technique: six-month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol 46(11):2134–2140. https://doi.org/10.1016/j.jacc.2005.07.065
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1–39. https://doi.org/10.1016/j.echo.2014.10.003. (e14)
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 29(4):530–538. https://doi.org/10.1007/s00134-003-1662-x
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM et al (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39(2):165–228. https://doi.org/10.1007/s00134-012-2769-8
Stone GW, Adams DH, Abraham WT, Kappetein AP, Généreux P, Vranckx P et al (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 2: endpoint definitions: a consensus document from the Mitral Valve Academic Research Consortium. Eur Heart J 36(29):1878–1891. https://doi.org/10.1093/eurheartj/ehv333
Tibshirani R (1997) The lasso method for variable selection in the Cox model. Stat Med 16(4):385–395. https://doi.org/10.1002/(sici)1097-0258(19970228)16:4%3c385::aid-sim380%3e3.0.co;2-3
Cremer J, Martin M, Redl H, Bahrami S, Abraham C, Graeter T et al (1996) Systemic inflammatory response syndrome after cardiac operations. Ann Thorac Surg 61(6):1714–1720. https://doi.org/10.1016/0003-4975(96)00055-0
Sablotzki A, Friedrich I, Mühling J, Dehne MG, Spillner J, Silber RE et al (2002) The systemic inflammatory response syndrome following cardiac surgery: different expression of proinflammatory cytokines and procalcitonin in patients with and without multiorgan dysfunctions. Perfusion 17(2):103–109. https://doi.org/10.1177/026765910201700206
Fransen E, Maessen J, Dentener M, Senden N, Geskes G, Buurman W (1998) Systemic inflammation present in patients undergoing CABG without extracorporeal circulation. Chest 113(5):1290–1295. https://doi.org/10.1378/chest.113.5.1290
Franke A, Lante W, Fackeldey V, Becker HP, Kurig E, Zöller LG et al (2005) Pro-inflammatory cytokines after different kinds of cardio-thoracic surgical procedures: is what we see what we know? Eur J Cardiothorac Surg 28(4):569–575. https://doi.org/10.1016/j.ejcts.2005.07.007
Kalinskaya A, Dukhin O, Lebedeva A, Maryukhnich E, Rusakovich G, Vorobyeva D et al (2022) Circulating cytokines in myocardial infarction are associated with coronary blood flow. Front Immunol 13:837642. https://doi.org/10.3389/fimmu.2022.837642
Lindman BR, Goldstein JS, Nassif ME, Zajarias A, Novak E, Tibrewala A et al (2015) Systemic inflammatory response syndrome after transcatheter or surgical aortic valve replacement. Heart 101(7):537–545. https://doi.org/10.1136/heartjnl-2014-307057
Izbicki G, Rudensky B, Na’amad M, Hershko C, Huerta M, Hersch M (2004) Transfusion-related leukocytosis in critically ill patients. Crit Care Med 32(2):439–442. https://doi.org/10.1097/01.Ccm.0000104951.94820.A9
Xu K, Xie S, Huang Y, Zhou T, Liu M, Zhu P et al (2020) Cell-type transcriptome atlas of human aortic valves reveal cell heterogeneity and endothelial to mesenchymal transition involved in calcific aortic valve disease. Arterioscler Thromb Vasc Biol 40(12):2910–2921. https://doi.org/10.1161/atvbaha.120.314789
Ma H, Killaars AR, DelRio FW, Yang C, Anseth KS (2017) Myofibroblastic activation of valvular interstitial cells is modulated by spatial variations in matrix elasticity and its organization. Biomaterials 131:131–144. https://doi.org/10.1016/j.biomaterials.2017.03.040
Baum J, Duffy HS (2011) Fibroblasts and myofibroblasts: what are we talking about? J Cardiovasc Pharmacol 57(4):376–379. https://doi.org/10.1097/FJC.0b013e3182116e39
Serrano-López J, Martín-Antonio B (2021) Inflammaging, an imbalanced immune response that needs to be restored for cancer prevention and treatment in the elderly. Cells. https://doi.org/10.3390/cells10102562
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153(6):1194–1217. https://doi.org/10.1016/j.cell.2013.05.039
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E et al (2000) Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci 908:244–254. https://doi.org/10.1111/j.1749-6632.2000.tb06651.x
Barcena ML, Aslam M, Pozdniakova S, Norman K, Ladilov Y (2022) Cardiovascular inflammaging: mechanisms and translational aspects. Cells. https://doi.org/10.3390/cells11061010
Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 14(10):576–590. https://doi.org/10.1038/s41574-018-0059-4
Khansari N, Shakiba Y, Mahmoudi M (2009) Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat Inflamm Allergy Drug Discov 3(1):73–80. https://doi.org/10.2174/187221309787158371
Franceschi C, Campisi J (2014) Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S4-9. https://doi.org/10.1093/gerona/glu057
Jobs A, Grund S, de Waha-Thiele S, Ledwoch J, Sievert H, Rassaf T et al (2021) Deep sedation versus general anaesthesia for transcatheter mitral valve repair: an individual patient data meta-analysis of observational studies. EuroIntervention 16(16):1359–1365. https://doi.org/10.4244/eij-d-20-00607
Jentzer JC, Lawler PR, van Diepen S, Henry TD, Menon V, Baran DA et al (2020) Systemic inflammatory response syndrome is associated with increased mortality across the spectrum of shock severity in cardiac intensive care patients. Circ Cardiovasc Qual Outcomes 13(12):e006956. https://doi.org/10.1161/circoutcomes.120.006956
Cuinet J, Garbagnati A, Rusca M, Yerly P, Schneider AG, Kirsch M et al (2020) Cardiogenic shock elicits acute inflammation, delayed eosinophilia, and depletion of immune cells in most severe cases. Sci Rep 10(1):7639. https://doi.org/10.1038/s41598-020-64702-0
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M et al (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380(18):1695–1705. https://doi.org/10.1056/NEJMoa1814052
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D et al (2019) Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 380(18):1706–1715. https://doi.org/10.1056/NEJMoa1816885
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM et al (2018) Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 379(24):2307–2318. https://doi.org/10.1056/NEJMoa1806640
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
FS: conceptualization; investigation; data collection; methodology; writing original draft. CP: validation; writing—review and editing. MG: validation; data collection; writing—review and editing. PN: validation; writing—review and editing. NPM: validation; writing—review and editing. HA-C: validation; writing—review and editing. NA: validation; writing—review and editing. TR: validation; writing—review and editing. SH: validation; writing—review and editing. HS: project administration; supervision; validation; writing—review and editing. AK: project administration; supervision; validation; writing—review and editing. MJ: project administration; supervision; validation; writing—review and editing. EX: project administration; supervision; validation; writing—review and editing. TT: conceptualization; project administration; supervision; validation; writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Technical University of Munich (OBSERV-MITRA-R: Date: 05.11.2020, Number: 600/20 S-EB). All patients provided written informed consent.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Syryca, F., Pellegrini, C., Gollreiter, M. et al. Incidence of systemic inflammatory response syndrome and patient outcome following transcatheter edge-to-edge mitral valve repair. Clin Res Cardiol 113, 276–287 (2024). https://doi.org/10.1007/s00392-023-02316-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-023-02316-y