Abstract
Background
Color tissue Doppler imaging (TDI) M-mode can be used to measure the cardiac time intervals including the isovolumic contraction time (IVCT), the left ventricular ejection time (LVET), the isovolumic relaxation time (IVRT), and the combination of all the cardiac time intervals in the myocardial performance index (MPI) defined as [(IVCT + IVRT)/LVET]. The aim of this study was to establish normal age- and sex-based reference ranges for the cardiac time intervals.
Methods and results
A total of 1969 participants free of cardiovascular diseases and risk factors from the general population with limited age range underwent an echocardiographic examination including TDI. The median age was 46 years (25th–75th percentile: 33–58 years), and 61.5% were females. In the entire study population, the IVCT was observed to be 40 ± 10 ms [95% prediction interval (PI) 20–59 ms], the LVET 292 ± 23 ms (95% PI 248–336 ms), the IVRT 96 ± 19 ms (95% PI 59–134 ms) and MPI 0.47 ± 0.09 (95% PI 0.29–0.65). All the cardiac time intervals differed significantly between females and males. With increasing age, the IVCT increased in females, but not in males. The LVET did not change with age in both sexes, while the IVRT increased in both sexes with increasing age. Furthermore, we developed regression equations relating the heart rate to the cardiac time intervals and age- and sex-based normal reference ranges corrected for heart rate.
Conclusion
In this study, we established normal age- and sex-based reference ranges for the cardiac time intervals. These normal reference ranges differed significantly with sex.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The cardiac time intervals include the isovolumic contraction time (IVCT), the left ventricular ejection time (LVET), the isovolumic relaxation time (IVRT), and the combination of all the cardiac time intervals in the myocardial performance index (MPI) defined as [(IVCT + IVRT)/LVET]. In varieties of cardiovascular diseases, the cardiac time intervals have shown to be sensitive markers for diagnosis and prognosis [1,2,3]. A newer echocardiographic method for obtaining the cardiac time intervals is by applying color tissue Doppler imaging (TDI) M-mode. This method has been shown to be superior to the conventional pulsed-wave Doppler method [4, 5].
It has previously been demonstrated that the cardiac time intervals vary with sex and age [6,7,8]. Furthermore, the cardiac time intervals are inversely related to heart rate and should be corrected for heat rate [1]. The first normal reference ranges for the systolic cardiac time intervals (IVCT and LVET) corrected for heart rate were established in 1968 [6]. In the meantime, the methods of obtaining the cardiac time intervals and the epidemiology of the general population and cardiovascular diseases have changed. Hence, there is an unmet need to develop new age- and sex-based normal reference ranges for the cardiac time intervals. This is essential to incorporate and use the cardiac time intervals in clinical practice.
The primary aim of this study was to establish age- and sex-based normal reference ranges for the cardiac time intervals. Further, we wanted to develop regression equations relating the heart rate to the cardiac time intervals and age- and sex-based normal reference ranges corrected for heart rate.
Methods
Study population
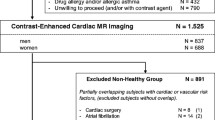
The Copenhagen City Heart Study (CCHS) is a prospective cardiovascular population study of randomly selected participants from the general population in Denmark (clinicaltrials.gov identifier: NCT02993172). Information on this study cohort has been described in detail elsewhere [9]. The current study is an echocardiographic substudy of the fifth CCHS spanning from 2011 to 2015. A total of 4466 participants underwent a health examination including a detailed echocardiographic examination [10]. In order to ensure a healthy study population, participants with the following cardiovascular diseases were excluded: hypertension (n = 2328), diabetes (n = 33), heart failure (n = 6), atrial fibrillation/flutter (n = 28), ischemic heart disease (n = 47), heart valve disease (n = 6) and participants who reported use of heart medication (n = 8). Additionally, participants without available measurements of the cardiac time intervals (n = 28) were excluded. Finally, participants with missing data (n = 13) were excluded. Hence, the final study population consisted of 1969 participants free of cardiovascular diseases and risk factors. This study population was used to develop normal reference ranges for the cardiac time intervals.
The study was conducted according to the 2nd Declaration of Helsinki and approved by the Regional Ethics Committee. All participants gave written informed consent before the examination. All participants attended a general health examination, which included physical examination, self-administered questionnaire and blood samples [9].
Baseline information
The Danish National Patient Registry was used to collect information on diagnoses using the International Classification of Disease (ICD-8 and ICD-10) codes. The obtained diagnoses included heart valve disease (aortic stenosis/regurgitation or mitral stenosis/regurgitation), atrial fibrillation/flutter, heart failure, ischemic heart disease, diabetes mellitus and hypertension. Definitions of ischemic heart disease, diabetes mellitus and hypertension have previously been described in detail [10].
Echocardiography
Echocardiography was performed using Vivid 9 ultrasound systems (GE Healthcare, Horten, Norway) by experienced sonographers. The echocardiograms were stored and analyzed offline with commercially available software (EchoPac version 113.15, GE Healthcare, Horten Norway) [10].
Measures of left ventricular (LV) dimensions were performed in the parasternal long-axis view at end-diastole. The LV dimensions included interventricular septal diameter, LV internal diameter and LV posterior wall diameter. LV mass index (LVMI) was estimated by dividing LV mass with the body surface area. LV hypertrophy was defined as LVMI ≥ 96 g/m2 for females and ≥ 116 g/m2 for males. LV ejection fraction (LVEF) was estimated by the Simpson’s biplane method [11].
Two-dimensional speckle tracking echocardiography was performed in the three apical views by using an automated function that defined a region of interest (ROI). This has previously been described in detail [10]. Global longitudinal strain (GLS) was calculated as an average peak strain from the three apical views.
The left atrial (LA) volume was measured using the biplane area-length method and indexed to body surface area to create left atrial volume index (LAVI) [11]. Pulsed-wave Doppler was used to record the mitral inflow between the tips of the mitral valve leaflets. The peak velocity of early (E) and atrial (A) diastolic filling and deceleration time of the E-wave were measured, and the E/A ratio was calculated.
The color TDI was used to obtain the peak systolic (s′), early diastolic (e′) and late diastolic (a′) velocities. The average values of e′ were used to calculate E/e′.
Tissue Doppler imaging
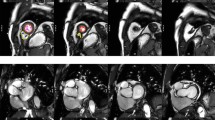
The cardiac time intervals were measured from the color TDI 4-chamber view at the highest possible frame rate (median frame rate: 162 frames per second [25th–75th percentile: 161–166 frames per second]). A 2–4 cm straight M-mode line was placed through the septal half of the anterior mitral valve leaflet (Fig. 1).
The mitral valve closure (MVC) was determined by the color shift from blue/turquoise to red at end-diastole. The aortic valve opening (AVO) was determined by the color shift from blue to red at the beginning of the systole. The aortic valve closure (AVC) was determined by the color shift from red to blue at end-systole. The mitral valve opening (MVO) was determined by the color shift from red orange to yellow.
The IVCT was defined as the time interval from the MVC to AVO, the LVET was defined as the time interval from the AVO to AVC, and the IVRT was defined as the time interval from the AVC to MVO. This method has previously been described in detail and a validation of this method has been performed [4, 5, 12].
Statistics
The statistical analyses were conducted using STATA SE version 15.1 (StataCorp, College Station, Texas). Histograms and QQ-plots were used to assess for normal distribution. Continuous Gaussian distributed variables were compared using Student t test and reported as mean ± SD. Kruskal–Wallis test was used for comparing continuous non-Gaussian distributed variables and reported as medians with 25th–75th percentiles. Categorical variables were compared using Chi-square test and reported as percentages.
p values for trend were calculated using linear regression for continuous distributed variables and by Chi-square test for trend for proportions.
Normal reference ranges for the cardiac time intervals were established for the entire study sample. Additionally, to establish age- and sex-based normal reference ranges, the study sample was stratified by sex and by sex and age categories (20–34, 35–49, 50–64, and > 65 years). The normal reference ranges were reported as mean ± SD with corresponding 95% prediction intervals (PI). Prediction plots were generated to illustrate the relationship between the cardiac time intervals and age. Regression equations relating the heart rate to the cardiac time intervals were calculated.
We conducted different sensitivity analyses to determine whether the size of the LAVI, the value of GLS or PALS affected our results. We defined normal LAVI as ≤ 34 mL/m2 and abnormal LAVI as > 34 mL/m2 [13]. Normal GLS was defined as an absolute value of ≥ 15.8% and abnormal GLS < 15.8% [10]. Normal PALS was defined as a value ≥ 23% and abnormal PALS as < 23% [14]. The definitions of GLS and PALS are based on data from the CCHS [10, 14].
A p value < 0.05 in two-sided tests was considered statistically significant.
Results
Baseline characteristics
The baseline characteristics for the entire study population and stratified by age categories are shown in Table 1. The participants median age was 46 years (25th–75th percentile: 33–58 years), and 61.5% (n = 1211) were females. The mean systolic and diastolic blood pressure were 124 mmHg (25th–75th percentile: 116–131 mmHg) and 74 mmHg (25th–75th percentile: 69–80 mmHg), respectively, and mean heart rate was 63 ± 10 beats per minute. The mean LVEF was 58 ± 5%
Normal reference ranges of the cardiac time intervals
In Table 2, the normal reference ranges including 95% prediction intervals of the cardiac time intervals are shown for the entire study population and stratified by sex. In the entire study population, the IVCT was observed to be 40 ± 10 ms (95% PI 20–59 ms), the LVET 292 ± 23 ms (95% PI 248–336 ms), the IVRT 96 ± 19 ms (95% PI 59–134 ms) and MPI 0.47 ± 0.09 (95% PI 0.29–0.65). All the cardiac time intervals differed significantly between females and males (p < 0.001 for all). The IVCT and LVET were significantly longer in females than males, while the IVRT was significantly longer in males than females. Greater values of MPI were observed in males than females.
Table 3 shows normal reference ranges including 95% PI of the cardiac time intervals stratified by sex and age. Sex modified the relationship between IVCT and age (p for interaction = 0.003), such that the IVCT increased significantly across age categories in females (p < 0.001); however, the IVCT did not increase significantly across age categories in males (p = 0.55). The LVET did not change significantly across age categories in neither females (p = 0.08) nor males (0.38). The IVRT increased significantly across age categories in both females (p < 0.001) and males (p < 0.001). The MPI increased significantly across age categories in both females (p < 0.001) and males (p < 0.001). Figure 2 illustrates the association between the cardiac time intervals and age in females and males.
Normal reference ranges of the IVCT, LVET, IVRT and MPI according to sex and age. The regression line is in black. The 95% confidence interval is in gray. The 95% prediction interval is the dotted black line. IVCT isovolumic contraction time, IVRT isovolumic relaxation time, LVET left ventricular ejection time, MPI myocardial performance index
Normal reference ranges of the cardiac time intervals corrected for heart rate
Table 4 shows the developed regression equations relating heart rate to each cardiac time interval and normal reference ranges of the cardiac time intervals including 95% PI in the entire study population and stratified by sex. In females, the regression equation for IVCT was found to be 0.18 × HR + IVCT and the IVCT corrected for heart rate was found to be 52 ± 9 ms (95% PI 34–70 ms). In males, the regression equation for IVCT was found to be 0.15 × HR + IVCT and the IVCT corrected for heart rate was found to be 48 ± 10 ms (95% PI 28–68 ms). In females, the regression equation for LVET was found to be 1.51 × HR + LVET and the LVET corrected for heart rate was found to be 393 ± 16 ms (95% PI 361–423 ms). In males, the regression equation for LVET was found to be 1.38 × HR + LVET and the LVET corrected for heart rate was found to be 372 ± 17 ms (95% PI 340–406 ms). In females, the regression equation for IVRT was found to be 0.30 × HR + IVRT and the IVRT corrected for heart rate was found to be 113 ± 19 ms (95% PI 77–150 ms). In males, the regression equation for IVRT was found to be 0.19 × HR + IVRT and the IVRT corrected for heart rate was found to be 111 ± 19 ms (95% PI 74–149 ms).
Tables 5 and 6 show regression equations relating heart rate to each cardiac time interval and normal reference ranges including 95% PI stratified by sex and age. Figure 3 illustrates the association between the cardiac time intervals corrected for heart rate and age in females and males.
Normal reference ranges of the IVCT, LVET, IVRT corrected for heart rate according to sex and age. The regression line is in black. The 95% confidence interval is in gray. The 95% prediction interval is the dotted black line. IVCT isovolumic contraction time, IVRT isovolumic relaxation time, LVET left ventricular ejection time
Normal reference ranges of the cardiac time intervals stratified by LAVI, GLS and PALS
In a sensitivity analysis, we included a total of 1954 healthy participants where measurements of the cardiac time intervals and LAVI were available. The IVCT was significantly increased in participants with abnormal LAVI than those with normal LAVI. The LVET, IVRT and MPI did not differ significantly with regard to the size of LAVI (Supplemental Table S1).
In another sensitivity analysis, we included a total of 1903 healthy participants where measurements of the cardiac time intervals and GLS were available. All the cardiac time intervals differed significantly between participants with normal GLS and abnormal GLS. In participants with abnormal GLS, the IVCT was increased, the LVET was decreased, and the IVRT and MPI were increased (Supplemental Table S2). Additionally, in another sensitivity analysis we included a total of 1785 healthy participants with available measurements of the cardiac time intervals and PALS. All the cardiac time intervals differed significantly between participants with normal PALS and abnormal PALS. The IVCT was increased, the LVET was decreased, and the IVRT and MPI were increased in participants with abnormal PALS (Supplemental Table S3).
Normal reference ranges of the cardiac time intervals according to hypertension and atrial fibrillation
In a secondary analysis to assess the normal values in participants with hypertension or atrial fibrillation (AF), we included participants regardless of health status (n = 4374). The IVCT did not differ between participants with hypertension and without hypertension. In participants with hypertension, the LVET was decreased, while the IVRT and MPI were increased (Supplemental Table S4). In participants with AF, the IVCT was increased, the LVET was decreased and the MPI increased. The IVRT did not differ between participants with and without AF (Supplemental Table S5).
Discussion
This is the largest study providing normal reference ranges for the IVCT, LVET, IVRT and MPI in participants free of cardiovascular diseases and risk factors. In the current study, we report several relevant findings. (1) We established normal reference ranges including 95% PI for IVCT, LVET, IVRT and MPI in the entire study population and across four age categories for each sex. (2) We demonstrated that duration of all the cardiac time intervals differed significantly between females and males. (3) Additionally, we demonstrated how the duration of the cardiac time intervals varies with increasing age for each sex. (4) We developed regression equations relating the heart rate to IVCT, LVET and IVRT in the entire population and across four age categories for each sex.
Few studies have reported normal reference ranges for the cardiac time intervals. Weissler et al. established normal reference ranges for the systolic time intervals including IVCT and LVET [6]. The study was based on a total of 211 healthy participants (121 males and 90 females) aged 19–65 years. However, the definition of the healthy participants was not specified in the study. The IVCT and LVET were measured using simultaneous recordings of the electrocardiogram, the phonocardiogram and the carotid arterial pulse. These measurements were performed with the participants in supine position and fasting [6]. The normal reference ranges for IVCT and LVET were corrected for heart rate and reported as mean ± SD. The normal reference ranges of LVET were reported to be 418 ± 10 ms in females and 413 ± 10 ms in males, while the normal reference ranges of IVCT were reported to be 39 ± 9 ms in females and 33 ± 10 ms in males. In the current study, we found that the normal reference ranges of LVET were 393 ± 16 ms (95% PI 361–423 ms) in females and 372 ± 17 ms (95% PI 340–406 ms), while the normal reference ranges of IVCT were found to be 52 ± 9 ms (95% PI 34–70 ms) in females and 48 ± 10 ms (95% PI 28–68 ms). The difference in the normal reference ranges between the current study and the study by Weissler et al. in 1968 may be due to the different methods of measuring the cardiac time intervals. Furthermore, the prevalence of cardiovascular diseases in the general population has changed, which also may contribute to the difference in the normal reference ranges.
Another study by Biering-Sørensen et al. developed normal reference ranges for all the cardiac time intervals including MPI [8]. This study included participants from the fourth CCHS spanning from 2001 to 2003. A total of 974 participants (553 females and 421 males) without hypertension, diabetes, AF, heart failure and ischemic heart disease were included. The cardiac time intervals were measured by TDI M-mode. The normal reference ranges for the cardiac time intervals were reported as mean ± SD. However, the study did not report normal reference ranges for the cardiac time intervals corrected for heart rate. The authors found that all the cardiac time intervals except IVRT differed significantly between females and males. However, in the current study we found that all the cardiac time intervals including IVRT differed significantly between females and males. This is in accordance with the existing knowledge about sex-specific differences in cardiac structure and function [15, 16]. With increasing age, the IVCT increased in females, but not in males. It has previously been shown that both advanced age and female sex are associated with an increase ventricular systolic and diastolic stiffness even in the absence of cardiovascular diseases [17]. Therefore, we speculate that the increased ventricular systolic stiffness could potentially lead to the increase in IVCT observed in females.
We found that the IVRT increased with increasing age in both sexes, which is in agreement with previous study findings [18, 19]. Bukachi et al. reported that the IVRT increased with increasing age in participants from the general population (n = 128) aged 25–88 years [19].
In healthy subjects (n = 43), Reant et al. have reported the normal reference ranges for the LVET as mean ± SD and developed a regression equation relating the heart rate to the LVET [20]. However, this study was not dedicated to establish normal reference ranges. The healthy subjects were comprised of a group without heart disease, diabetes, or hypertension and with normal echocardiography and electrocardiogram. The LVET was measured using pulsed-wave Doppler [20]. The authors developed the following regression equation relating the heart rate to the LVET: (LVET = 1.5 × HR + LVET). Similarly, in our study we developed the following equation for the entire study population (LVET = 1.4 × HR + LVET).
In the current study, we found that the LVET did not increase in neither females nor males. In accordance with our findings, it has previously been demonstrated that in 278 healthy participants aged 23–80 years, the LVET did not increase [21]. In the fourth CCHS, it was reported that the LVET decreased with increasing age; however, this decline was not statistically significant [8]. In contrast to these two studies, it has been shown that in 512 elderly participants aged 60–90 years, the LVET increased with aging [7]. The elderly participants with heart failure and those who used digitalis were excluded. However, participants with other cardiovascular diseases and risk factors were not excluded, which can explain the differences between this study and our study findings regarding LVET. Hence, the increase in LVET may be due to other cardiovascular diseases and not only increasing age. Furthermore, the study focused primarily on elderly participants, whereas our study assessed the effect of age on the cardiac time intervals across four age categories.
When comparing our study with all the above-mentioned studies, we included a lager study sample of participants (n = 1969) free of cardiovascular diseases and risk factors. Additionally, our study sample was comprised of participants with a wide spectrum of ages spanning from 21 to 97 years, which make it possible to develop normal reference ranges for the cardiac time intervals across four age categories for each sex. The above-mentioned studies only report the normal reference ranges as mean ± SD. However, in our study the developed normal reference ranges are reported as mean ± SD with corresponding 95% PI.
The finding that only IVCT was increased in participants with abnormal LAVI may due to the fact that during the IVCT, the left atrial pressure (LA) increases. Hence, an increased duration of the IVCT may lead to higher LA pressure. Thus, increased LA pressure may result in an enlargement of the left atrium. In a previous study from the fourth round of the CCHS including 1915 participants from the general population, we found that the IVCT was an independent predictor of AF and complicated AF defined as occurrence of either stroke or heart failure following the diagnosis of AF. No associations between LVET, IVRT, MPI, and AF remained significant after multivariable adjustment [22].
The normal values of the cardiac time intervals differed significantly between participants with normal GLS and abnormal GLS, and normal PALS and abnormal PALS, respectively. We excluded participants with cardiovascular diseases and risk factors to ensure a healthy study sample. However, the difference in normal values of the cardiac time intervals in participants with abnormal GLS or PALS may be due to the fact that both GLS and PALS are impaired before the cardiovascular diseases occur. We have previously shown that both GLS and PALS are independent predictors of cardiovascular morbidity and mortality in the general population [23,24,25].
In participants with hypertension, the LVET was significantly decreased, while the IVRT and MPI were significantly increased. Our findings are in agreement with previous studies that have demonstrated that the LVET was decreased, while the IVRT was increased in hypertensive patients [26,27,28].
In participants with AF, we found that the IVCT was increased, the LVET was decreased and the MPI increased. The IVRT did not differ between participants with and without AF. Our findings are in accordance with a previous study that have demonstrated that the LVET was decreased in patients with AF, while the pre-ejection time (PEP) including the IVCT increased [29].
Using the TDI M-mode method, the cardiac time intervals can be obtained with greater precision and better reproducibility as it is much easier to identify the clear color shifts caused by mitral valve movements throughout the cardiac cycle. By contrast, it can be difficult to accurately define the cardiac time intervals from velocity curves, when using the conventional pulsed-wave Doppler method [4, 5, 23, 30]. Moreover, the improvement of the TDI M-mode method may be due to the very high frame rate, typically from 160 to 200 frames per second, while the conventional pulsed-wave Doppler method uses a lower frame rate [31]. Additionally, when using the TDI M-mode method, the cardiac time intervals can be obtained regardless of heart rhythm, whereas the conventional method cannot assess the cardiac time intervals in patients with AF [12]. The cardiac time intervals can be obtained using the conventional pulsed-wave Doppler method as previously described by Tei and colleagues [32]. The interval between the onset and end of mitral inflow is equal to the sum of the IVCT, LVET, and IVRT (interval b). The duration of the LV outflow velocity profile is equal to the LVET (interval a). By subtracting b from a, the sum of the IVCT and IVRT can be obtained [32]. In patients with AF, there is no definite A wave or a′ wave due to lack of organized atrial activity [33]. Hence, the onset and end of mitral inflow and thereby the IVCT and IVRT cannot be assessed accurately due to the absence of A wave.
There is an increasing interest in the cardiac time intervals, since a novel drug (Omecamtiv mecarbil (OM)) acts specifically by increasing the LVET in patients with heart failure with reduced ejection fraction (HFrEF) [34]. Treatment with OM has very recently shown to improve outcomes in patients with HFrEF [35]. Therefore, it is of great clinical importance to develop age- and sex-based normal reference ranges for the cardiac time intervals. However, future studies are required to determine whether there is a desirable target of the cardiac time intervals in patients with HFrEF.
Study limitations
There are potential limitations to the current study. The CCHS is primarily composed of Caucasians, which limits the generalizability of our developed normal reference ranges for the cardiac time intervals to other populations with another composition. The cardiac time intervals can be measured by different methods including pulsed-wave Doppler, pulsed-wave TDI and TDI M-mode method [2]. These different methods of obtaining the cardiac time intervals may lead to different normal values. Therefore, our established normal reference ranges may not be generalizable to the cardiac time intervals obtained by other methods. Hence, future studies are required to assess the normal values of the cardiac time intervals for each method. In the current study, we don’t have data available regarding measurements of the cardiac time intervals using the pulsed-wave Doppler method. Therefore, we could not compare our findings based on the TDI M-mode method with measurements of the cardiac time intervals based on the conventional method from this cohort. Due to the high prevalence of cardiovascular diseases and risk factors among males, we excluded a higher proportion of males than females. Hence, our study sample was not fully representative of the general population.
A high prevalence of cardiovascular diseases and risk factors was among the participants aged > 65 years. Since we excluded participants with cardiovascular diseases and risk factors to ensure a healthy study sample, our group of participants aged > 65 years was small. Therefore, the assessment of the association of the cardiac intervals with age is limited. However, this group was larger, when comparing it to other studies that developed normal reference ranges for the cardiac time intervals.
Conclusion
In the current study, we established normal age- and sex-based reference ranges for the cardiac time intervals. Further, we developed both regression equations and age- and sex-based reference ranges relating the heart rate to the cardiac time intervals. We found that the duration of the cardiac time intervals differed significantly between females and males. With increasing age, the IVCT increased in females, but not in males. The LVET did not change in both sexes, while the IVRT increased in both sexes with increasing age. This emphasizes the need for age- and sex-based normal reference ranges for the cardiac time intervals.
References
Boudoulas H (1990) Systolic time intervals. Eur Heart J 11(Suppl I):93–104
Alhakak AS, Teerlink JR, Lindenfeld J, Böhm M, Rosano GMC, Biering-Sørensen T (2021) The significance of left ventricular ejection time in heart failure with reduced ejection fraction. Eur J Heart Fail 23(4):541–551
Alhakak AS, Møgelvang R, Schnohr P, Modin D, Brainin P, Gislason G et al (2020) The cardiac isovolumetric contraction time is an independent predictor of incident heart failure in the general population. Int J Cardiol 312:81–86
Kjaergaard J, Hassager C, Oh JK, Kristensen JH, Berning J, Sogaard P (2005) Measurement of cardiac time intervals by Doppler tissue M-mode imaging of the anterior mitral leaflet. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 18(10):1058–1065
Biering-Sørensen T, Mogelvang R, Pedersen S, Schnohr P, Sogaard P, Jensen JS (2011) Usefulness of the myocardial performance index determined by tissue Doppler imaging m-mode for predicting mortality in the general population. Am J Cardiol 107(3):478–483
Weissler AM, Harris WS, Schoenfeld CD (1968) Systolic time intervals in heart failure in man. Circulation 37(2):149–159
Willems JL, Roelandt J, De Geest H, Kesteloot H, Joossens JV (1970) The left ventricular ejection time in elderly subjects. Circulation 42(1):37–42
Biering-Sørensen T, Mogelvang R, de Knegt MC, Olsen FJ, Galatius S, Jensen JS (2016) Cardiac time intervals by tissue Doppler imaging M-mode: normal values and association with established echocardiographic and invasive measures of systolic and diastolic function. PLoS One 11(4):e0153636
Schnohr P, Jensen GB, Lange P, Scharling H, Appleyard M (2001) The copenhagen city heart study. Østerbroundersøgelsen: tables with data from the third examination 1991–1994. Eur Hear J Suppl 3:H1-83
Skaarup KG, Lassen MCH, Johansen ND, Olsen FJ, Lind JN, Jørgensen PG et al (2021) Age- and sex-based normal values of layer-specific longitudinal and circumferential strain by speckle tracking echocardiography: the Copenhagen City Heart Study. Eur Heart J Cardiovasc Imaging 23:jeab032
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 18(12):1440–1463
Biering-Sørensen T, Mogelvang R, Søgaard P, Pedersen SH, Galatius S, Jørgensen PG et al (2013) Prognostic value of cardiac time intervals by tissue Doppler imaging M-mode in patients with acute ST-segment-elevation myocardial infarction treated with primary percutaneous coronary intervention. Circ Cardiovasc Imaging 6(3):457–465
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Nielsen AB, Skaarup KG, Hauser R, Johansen ND, Lassen MCH, Jensen GB et al (2021) Normal values and reference ranges for left atrial strain by speckle-tracking echocardiography: the Copenhagen City Heart Study. Eur Heart J Cardiovasc Imaging 23(1):42–51
Hung CL, Gonçalves A, Shah AM, Cheng S, Kitzman D, Solomon SD (2017) Age- and sex-related influences on left ventricular mechanics in elderly individuals free of prevalent heart failure: the ARIC study (Atherosclerosis Risk in Communities). Circ Cardiovasc Imaging 10(1):e004510
Chung AK, Das SR, Leonard D, Peshock RM, Kazi F, Abdullah SM et al (2006) Women have higher left ventricular ejection fractions than men independent of differences in left ventricular volume: the Dallas Heart Study. Circulation 113(12):1597–1604
Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA (2005) Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation 112(15):2254–2262
Vancheri F, Vancheri S, Henein MY (2016) Effect of age on left ventricular global dyssynchrony in asymptomatic individuals: a population study. Echocardiogr Mt Kisco N 33(7):977–983
Bukachi F, Waldenström A, Mörner S, Lindqvist P, Henein MY, Kazzam E (2008) Age dependency in the timing of mitral annular motion in relation to ventricular filling in healthy subjects: Umea General Population Heart Study. Eur J Echocardiogr J Work Group Echocardiogr Eur Soc Cardiol 9(4):522–529
Reant P, Dijos M, Donal E, Mignot A, Ritter P, Bordachar P et al (2010) Systolic time intervals as simple echocardiographic parameters of left ventricular systolic performance: correlation with ejection fraction and longitudinal two-dimensional strain. Eur J Echocardiogr J Work Group Echocardiogr Eur Soc Cardiol 11(10):834–844
Lang E, Hubmann M (1977) Systolic periods in dependence of age. Z Alternsforsch 32(6):509–517
Alhakak AS, Brainin P, Møgelvang R, Jensen GB, Jensen JS, Biering-Sørensen T (2020) The cardiac isovolumetric contraction time is an independent predictor of incident atrial fibrillation and adverse outcomes following first atrial fibrillation event in the general population. Eur Heart J Cardiovasc Imaging 21(1):49–57
Biering-Sørensen T, Biering-Sørensen SR, Olsen FJ, Sengeløv M, Jørgensen PG, Mogelvang R et al (2017) Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: the Copenhagen City Heart Study. Circ Cardiovasc Imaging 10(3):e005521
Modin D, Biering-Sørensen SR, Møgelvang R, Alhakak AS, Jensen JS, Biering-Sørensen T (2019) Prognostic value of left atrial strain in predicting cardiovascular morbidity and mortality in the general population. Eur Heart J Cardiovasc Imaging 20(7):804–815
Alhakak AS, Biering-Sørensen SR, Møgelvang R, Modin D, Jensen GB, Schnohr P et al (2022) Usefulness of left atrial strain for predicting incident atrial fibrillation and ischaemic stroke in the general population. Eur Heart J Cardiovasc Imaging 23(3):363–371
Dodek A, Burg JR, Kloster FR (1975) Systolic time intervals in chronic hypertension: alterations and response to treatment. Chest 68(1):51–55
de Simone G, Greco R, Mureddu G, Romano C, Guida R, Celentano A et al (2000) Relation of left ventricular diastolic properties to systolic function in arterial hypertension. Circulation 101(2):152–157
Bella JN, Palmieri V, Liu JE, Kitzman DW, Oberman A, Hunt SC et al (2001) Relationship between left ventricular diastolic relaxation and systolic function in hypertension: the Hypertension Genetic Epidemiology Network (HyperGEN) Study. Hypertens Dallas Tex 1979 38(3):424–428
Boudoulas H, Lewis RP, Sherman JA, Bush CA, Dalamangas G, Forester WF (1978) Systolic time intervals in atrial fibrillation. Chest 74(6):629–634
Alhakak AS, Sengeløv M, Jørgensen PG, Bruun NE, Johnsen C, Abildgaard U et al (2021) Left ventricular systolic ejection time is an independent predictor of all-cause mortality in heart failure with reduced ejection fraction. Eur J Heart Fail 23(2):240–249
Lin F-C, Hsieh I-C, Lee C-H, Wen M-S (2008) Introduction of tissue Doppler imaging echocardiography—based on pulsed-wave mode. J Med Ultrasound 16(3):202–209
Tei C (1995) New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol 26(2):135–136
Mitter SS, Shah SJ, Thomas JD (2017) A test in context: E/A and E/e’ to assess diastolic dysfunction and LV filling pressure. J Am Coll Cardiol 69(11):1451–1464
Cleland JGF, Teerlink JR, Senior R, Nifontov EM, Mc Murray JJV, Lang CC et al (2011) The effects of the cardiac myosin activator, omecamtiv mecarbil, on cardiac function in systolic heart failure: a double-blind, placebo-controlled, crossover, dose-ranging phase 2 trial. Lancet Lond Engl 378(9792):676–683
Teerlink JR, Diaz R, Felker GM, McMurray JJV, Metra M, Solomon SD et al (2021) Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N Engl J Med 384(2):105–116
Funding
Open access funding provided by Royal Library, Copenhagen University Library. Alia Saed Alhakak was funded by a research Grant from the Gangsted Foundation. The sponsor had no role in the study design, data collection, data analysis, data interpretation, or writing of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TBS reports receiving research grants from Sanofi Pasteur and GE Healthcare, being a Steering Committee member of an Amgen financed and a Boston Scientific financed trial, on advisory boards for Sanofi Pasteur and Amgen, and speaker honorariums from Novartis, Sanofi Pasteur and GSK. PGJ reports speaker honorarium from Novo Nordisk and Astra Zeneca. The remaining authors have nothing to disclose.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alhakak, A.S., Olsen, F.J., Skaarup, K.G. et al. Age- and sex-based normal reference ranges of the cardiac time intervals: the Copenhagen City Heart Study. Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02269-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-023-02269-2