Abstract
Objective
The aim of this study was to assess the association between high on-aspirin treatment platelet reactivity (HAPR) and the subsequent risk of restenosis after percutaneous coronary intervention (PCI) with predominantly drug-eluting stents.
Background
The association between HAPR and subsequent risk of restenosis after PCI is unclear.
Methods
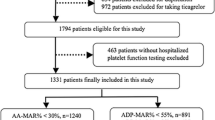
This study included 4839 patients undergoing PCI (02/2007–12/2011) in the setting of the Intracoronary Stenting and Antithrombotic Regimen-ASpirin and Platelet Inhibition (ISAR-ASPI) registry. Platelet function was assessed with impedance aggregometry using the multi-plate analyzer immediately before PCI and after intravenous administration of aspirin (500 mg). The primary outcome was clinical restenosis, defined as target lesion revascularization at 1 year. Secondary outcomes included binary angiographic restenosis and late lumen loss at 6- to 8-month angiography.
Results
The upper quintile cut-off of platelet reactivity measurements (191 AU × min) was used to categorize patients into a group with HAPR (platelet reactivity > 191 AU × min; n = 952) and a group without HAPR (platelet reactivity ≤ 191 AU × min; n = 3887). The primary outcome occurred in 94 patients in the HAPR group and 405 patients without HAPR (cumulative incidence, 9.9% and 10.4%; HR = 0.96, 95% CI 0.77–1.19; P = 0.70). Follow-up angiography was performed in 73.2% of patients. There was no difference in binary restenosis (15.2% vs. 14.9%; P = 0.79) or late lumen loss (0.32 ± 0.57 vs. 0.32 ± 0.59 mm; P = 0.93) between patients with HAPR versus those without HAPR.
Conclusions
This study did not find an association between HAPR, measured at the time of PCI, and clinical restenosis at 1 year after PCI.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients treated with percutaneous coronary intervention (PCI), drug-eluting stents (DES) have reduced the rates of restenosis and target lesion revascularization (TLR) compared with bare-metal stents (BMS) [1,2,3]. However, in-stent restenosis (ISR) after DES implantation can occur and it presents a clinical challenge in terms of therapy [4,5,6]. Given the principal role of platelets in acute thrombosis, pharmacological platelet inhibition is mandatory in PCI [7]. Early platelet response and platelet involvement in the cellular processes following PCI play an important role in the development of neo-intimal proliferation in response to vascular injury following PCI. Neo-intimal proliferation may subsequently lead to restenosis [8,9,10]. Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor is a guideline-recommended therapy for patients undergoing PCI [8,9,10]. The duration of DAPT varies depending on several factors, including the clinical presentation [10, 11]. Patients treated with PCI for ISR may benefit from prolonged DAPT [12]. High on-clopidogrel treatment platelet reactivity (HCPR) has been linked to a higher risk for ischemic events after PCI [13], and the evidence remains limited with respect to an association between HCPR subsequent ISR [14, 15]. Likewise, there are conflicting results with respect to an association between high on-aspirin treatment platelet reactivity (HAPR) and restenosis after PCI [16,17,18]. Reasoning from these facts, we undertook this study to investigate whether there is an association between HAPR and the subsequent risk of restenosis in patients undergoing PCI with predominantly DES implantation.
Methods
Patients
The study included 4839 patients undergoing PCI in 2 university hospitals (Deutsches Herzzentrum München and Medizinische Klinik and Poliklinik Innere Medizin I, Klinikum rechts der Isar, Technische Universität München, both in Munich, Germany) between February 2007 and December 2011. The source sample included 7090 patients enrolled in the Intracoronary Stenting and Antithrombotic Regimen-ASpirin and Platelet Inhibition (ISAR-ASPI) registry between February 2007 and May 2013 [19]. To be included in the current analysis, patients had to have been pretreated with aspirin, had platelet aggregation and clinical outcome (bleeding and ischemic events) data and Quantitative Coronary Angiography (QCA) data available. All patients received aspirin (an intravenous dose of 500 mg) and pre-treatment with an ADP receptor antagonist before the PCI procedure. In the post-PCI period, DAPT and other medications were prescribed as per standard practice. Aspirin, 100 mg twice daily, was recommended for an indeterminate duration. All patients had platelet function test measurements for HAPR performed immediately before the PCI procedure. Patients presenting with chronic coronary syndromes, unstable angina, ST-elevation myocardial infarction (STEMI), or non-ST-elevation myocardial infarction (NSTEMI) were included. Patients with cardiogenic shock and those who developed stent thrombosis at the index PCI were excluded. Data on mortality and stent thrombosis in the ISAR-ASPI registry have already been published [19]. The study conforms to the Declaration of Helsinki.
Cardiovascular risk factors were defined according to the generally accepted criteria. Global left ventricular ejection fraction was measured using the area–length method on left ventricular angiograms. Patient’s weight and height were measured during the index hospitalization and used to calculate the body mass index. Glomerular filtration rate was estimated using the Modification of Diet in Renal Disease (MDRD) Study equation.
Blood sampling and platelet function testing
Blood for platelet function testing was sampled into 4.5 ml lepirudin-containing blood vials (25 µg/ml, Refludan, Dynabyte, Munich, Germany). Blood for platelet function testing was collected from the arterial sheath before the start of PCI and after intravenous administration of aspirin. Arachidonic acid (AA) and adenosine diphosphate (ADP)-induced platelet aggregation were measured with MEA on an impedance aggregometer (Multiplate analyzer), and results obtained were expressed as arbitrary aggregation units plotted against time (AU × min). Impedance aggregometry using the Multiplate analyzer (Roche Diagnostics, Basel, Switzerland) was used for quantitative analysis of platelet function (inhibition) triggered by arachidonic acid (AA). The increase of impedance caused by platelet attachment to the incorporated electrodes is converted into aggregation units (AU) and plotted against time (AU × min). The materials used for impedance aggregometry including the activator substance AA originated from the manufacturer Roche Diagnostics (Basel, Switzerland).
Study outcome measures and definitions
HAPR was defined as having a platelet aggregation value in the upper quintile (20%). The primary endpoint was clinical restenosis, defined as a target lesion revascularization (TLR) performed at follow-up angiography for a lesion with a diameter stenosis > 70% (irrespective of the clinical symptoms) or for a lesion with a diameter stenosis ≥ 50% with clinical symptoms or signs indicative of myocardial ischemia [20]. The primary endpoint was assessed at 1 year. Secondary endpoints consisted of binary angiographic restenosis (BAR) and late lumen loss (LLL) at 6–8-month follow-up angiography. The BAR was defined as a stenosis ≥ 50% lumen obstruction on control angiography. The LLL was calculated as the difference between the post-stenting minimal lumen diameter (MLD) and the MLD measured at follow-up coronary angiography. Angiographic assessment was performed offline by blinded personnel of the Quantitative Coronary Angiography (QCA) core laboratory using a validated automated edge detection system (CMS version 7.1, Medis Medical Imaging Systems, Leiden, The Netherlands). In-hospital bleeding, defined according to the Thrombolysis in Myocardial Infarction (TIMI) group criteria was also assessed.
Follow-up
Patients were hospitalized for at least 2 days after the index PCI. The post-discharge follow-up included telephone interviews at 30 days, 6 months and 1 year. Patients who had clinical symptoms underwent a comprehensive clinical, electrocardiographic, and laboratory assessment in the outpatient clinic. As a standard practice in our institutions, at the time of patient’s inclusion in the registry, all patients were scheduled to undergo coronary angiography 6 months after the procedure or whenever they showed symptoms or signs of myocardial ischemia. The data were prospectively collected and saved in an electronic database by personnel of the ISAResearch Center. Information from referring physicians and hospital readmissions was also incorporated into the database.
Statistical methods
Continuous data are presented using mean ± standard deviation (SD) or median [25th–75th] percentiles. The distribution pattern of continuous data was assessed using the Kolmogorov–Smirnov test. Categorical data are presented as counts and proportions (%). Continuous variables were compared using the t test or Wilcoxon rank-sum test, as appropriate. Categorical data were compared using the chi-square test. Cumulative incidence of the primary outcome was calculated using the Kaplan–Meier method, and the differences in event-free survival were compared with the log-rank test. The Cox proportional hazards model was performed to assess the correlates of the primary outcome. The multiple linear regression model was used to assess the association of HAPR with BAR. The following variables were entered into the models: HAPR, age, sex, body mass index, arterial hypertension, hypercholesterolemia, smoking, clinical presentation, glomerular filtration rate, baseline C-reactive protein, ADP-induced platelet aggregation values, stent type, plus HAPR-by-clinical presentation interaction term. All analyses were performed using the R Statistical Software (R Statistical Software, Foundation for Statistical Computing, Vienna, Austria). A two tailed P value of < 0.05 was considered to confer statistical significance.
Results
Patients
The upper quintile cut-off of platelet reactivity measurements in our study was 191 AU × min. Based on the upper quintile cut-off of platelet reactivity measurements, patients were categorized into 2 groups: a group with HAPR (platelet reactivity ≥ 191 AU × min; n = 952 patients) and a group without HAPR (platelet reactivity < 191 AU × min; n = 3887 patients). Baseline data are shown in Table 1. Patients with versus without HAPR appear to differ with respect to several characteristics. Patients with HAPR were less likely to have arterial hypertension and hypercholesterolemia and had lower body mass index, lower glomerular filtration rate and higher levels of C-reactive protein compared with patients without HAPR. Overall, 2863 patients (59.2%) presented with chronic coronary syndromes and 1976 patients (40.8%) presented with acute coronary syndromes. The angiographic and the procedural characteristics (lesion-based analysis) are shown in Table 2. The majority of lesions in both groups (> 95%) were treated with a DES at the index PCI.
Primary endpoint (clinical restenosis)
The primary endpoint occurred in 94 of 952 patients with HAPR and 405 of 3887 patients without HAPR (cumulative incidence, 9.9% and 10.4%, respectively, hazard ratio [HR] = 0.96, 95% confidence interval [CI] 0.77–1.19; P = 0.70). In-hospital bleeding events (TIMI major or minor) occurred in 68 of 952 patients with HAPR and 232 of 3887 patients without HAPR (7.1% vs. 6.0%; P = 0.18).
The Cox proportional hazards model (see methods for variables we adjusted for) showed that HAPR was not an independent correlate of the primary endpoint (adjusted hazard ratio = 0.98, 95% confidence interval 0.78–1.23; P = 0.85, calculated per HAPR quintile). There was no HAPR-by-clinical presentation (chronic coronary syndromes or acute coronary syndromes) interaction with respect to the primary endpoint (P for interaction = 0.32).
Secondary endpoints (angiographic outcomes)
Repeat coronary angiography was performed in 73.2% of patients at 6–8 months after the index PCI. The angiographic outcomes for both groups are detailed in Table 3. There were no significant differences in the rates of BAR (15.2% vs. 14.9%; P = 0.79) or the degree of LLL (0.32 ± 0.57 vs. 0.32 ± 0.59 mm; P = 0.93; Fig. 1) between the two groups. HAPR was also not independently associated with the increased risk of BAR (adjusted odds ratio = 0.99 [0.97–1.01], P = 0.30, calculated per HAPR unit). There was no HAPR-by-clinical presentation (chronic coronary syndromes or acute coronary syndromes) interaction with respect to the BAR (P for interaction = 0.14).
Discussion
The main findings of this study may be summarized as follows: (1) HAPR assessed at the time of PCI was not associated with increased risk of clinical restenosis (defined as TLR) at 1 year after DES implantation. (2) There was no association between HAPR and angiographic results including BAR and LLL on repeat coronary angiography at 6–8 months after PCI.
Restenosis may be secondary to neointimal hyperplasia as a consequence of vascular injury during PCI. PCI induces vascular injury and exposes sub-endothelial tissue inducing an adhesive platelet response. Platelet adhesion at the site of PCI-induced vascular injury can lead to local thrombus formation, which may be an important step in the development of restenosis. Platelet recruitment in the area of the neo-intimal injury can promote proliferation and migration of smooth muscle cells [21,22,23]. Preclinical studies have suggested a relationship between an early platelet response and subsequent development of restenosis. However, whether antithrombotic therapy can mitigate this response and reduce the risk of restenosis remains unclear [24,25,26,27]. Several pharmaco-therapeutic strategies were tested in this regard, including warfarin [28], heparin [29], bivalirudin [30], ticlopidine [31], thromboxane A2 blockers [16, 32], and a combination of aspirin and dipyridamole [33]. Some of these studies have demonstrated a reduction in early thrombotic events post PCI but not a reduction in restenosis rates [16, 30, 33].
HCPR is associated with a higher risk for thrombotic events after PCI [13]. However, clinical studies assessing the antirestenotic efficacy of clopidogrel have reported conflicting results [14, 15]. Schulz et al. [15] showed that HCPR was not associated with an increased risk of restenosis in 1608 patients with HCPR after DES implantation. Conversely, Fu et al. [14] showed that HCPR was independently associated with the increased risk of ISR. A sub-study of the Prolonging Dual Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia (PRODIGY) trial suggested that patients treated with repeat PCI for ISR may benefit from long-term (24 months) administration of DAPT [12].
Aspirin is a well-established therapy for patients with cardiovascular disease. The beneficial effects of aspirin in terms of reduction of vascular death, myocardial infarction, or stroke in patients with stable coronary heart disease or acute coronary syndromes are recognized and current guidelines recommend aspirin as standard maintenance therapy in these patients [8]. However, the impact of HAPR on clinical outcomes is less clear than the impact of HCPR. A previous publication from the ISAR-ASPI registry showed an association between HAPR and increased risk of death or stent thrombosis at 1 year after DES implantation [19]. Conversely, a prospective (Assessment of Dual AntiPlatelet Therapy with Drug-Eluting Stents) registry of 8665 patients did not show a significant association between HAPR and the risk for stent thrombosis, myocardial infarction or death. However, the study showed an inverse association between HAPR and bleeding with a significant 35% lower adjusted risk for bleeding in patients with HAPR after DES implantation [34].
Few small studies have investigated the association between HAPR and the risk for ISR [16,17,18]. A randomized study of 216 patients undergoing angioplasty for a previously untreated native coronary artery lesions showed that aspirin reduced the rate of restenosis at 6 months in lesion-based analysis (25% vs. 38%) compared with placebo demonstrating a small benefit of aspirin in reducing the restenosis after angioplasty [17]. LLL was also less in aspirin-treated patients compared with placebo-treated patients (16 ± 22% vs. 22 ± 25%) [17]. Savage et al. [16] reported that aspirin protected against late ischemic events after angioplasty even though angiographic restenosis was not significantly reduced. Finally, Pamuckcu et al. [18] assessed the association between aspirin resistance and ISR in 204 patients with coronary artery disease after coronary stent implantation. Aspirin resistance was higher (31.3% vs. 10.7%) in patients who developed ISR compared with those who did not develop ISR. The current investigation may be the first large-scale study assessing the association between HAPR and clinical and angiographic parameters of restenosis after DES implantation. The data showed that there was no difference in the occurrence of the primary endpoint, 1-year rates of clinical restenosis between patients with and without HAPR. In addition, the rate of BAR and the degree of LLL on coronary angiography at 6- to 8-month post-PCI did not differ among patients with or without HAPR.
Limitations
The current study has several limitations. This is an observational retrospective analysis of registry-based data. As such, it has the limitations inherent to this type of studies. In addition, baseline (off-treatment) platelet function values are missing and therefore we could not perform an assessment of aspirin response. However, at the time of the study, only the Multiplate analyzer was used as part of routine platelet function testing following PCI. Thus, we acknowledge the lack of other assays to assess platelet reactivity such as calibrated automated thrombogram (CAT) assay. Therefore, it is unclear whether our findings can be extrapolated to other platelet function testing devices. At the time of patients’ inclusion in the registry, a maintenance dose of aspirin of 100 mg twice daily was recommended as per local practice. Although it does not reflect current recommendations with respect to the maintenance dose of aspirin after PCI, we do not believe that the higher dose of aspirin as used in current study has had an impact on the main study outcomes. Follow-up angiography was not performed in approximately 27% of the patients. Finally, the study findings were based on a single platelet reactivity measurement, and consequently we have no follow-up or serial data on the chronic platelet response.
Conclusions
In patients with coronary artery disease, HAPR assessed at the time of PCI was not associated with increased risk of clinical restenosis (defined as TLR) at 1-year post-PCI compared to patients without HAPR. In addition, the risk of binary angiographic restenosis and the degree of late lumen loss on 6- to 8-month repeat coronary angiography were similar between the two groups. Further prospective studies may be useful to further elucidate any association between the degree of peri-procedural platelet inhibition and the subsequent risk of restenosis after DES implantation.
Data availability
The authors confirm that the data used for this study might be shared after reasonable request and submission of an analysis plan to the corresponding author.
Abbreviations
- AA:
-
Arachidonic acid
- ADP:
-
Adenosine diphosphate
- AU:
-
Aggregation unit
- BAR:
-
Binary angiographic restenosis
- BMS:
-
Bare-metal stent
- CI:
-
Confidence interval
- DES:
-
Drug-eluting stent
- HAPR:
-
High on-aspirin treatment platelet reactivity
- HCPR:
-
High on-clopidogrel treatment platelet reactivity
- HR:
-
Hazard ratio
- IRS:
-
In-stent restenosis
- LLL:
-
Late lumen loss
- MI:
-
Myocardial infarction
- MLD:
-
Minimal lumen diameter
- NSTEMI:
-
Non-ST-elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- ST:
-
Stent thrombosis
- STEMI:
-
ST-elevation myocardial infarction
- TIMI:
-
Thrombolysis in Myocardial Infarction
- TLR:
-
Target lesion revascularization
- QCA:
-
Quantitative Coronary Angiography
References
Kastrati A, Mehilli J, Pache J, Kaiser C, Valgimigli M, Kelbaek H, Menichelli M, Sabate M, Suttorp MJ, Baumgart D, Seyfarth M, Pfisterer ME, Schomig A (2007) Analysis of 14 trials comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med 356:1030–1039
Stettler C, Wandel S, Allemann S, Kastrati A, Morice MC, Schomig A, Pfisterer ME, Stone GW, Leon MB, de Lezo JS, Goy JJ, Park SJ, Sabate M, Suttorp MJ, Kelbaek H, Spaulding C, Menichelli M, Vermeersch P, Dirksen MT, Cervinka P, Petronio AS, Nordmann AJ, Diem P, Meier B, Zwahlen M, Reichenbach S, Trelle S, Windecker S, Juni P (2007) Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet 370:937–948
Cassese S, Byrne RA, Tada T, Pinieck S, Joner M, Ibrahim T, King LA, Fusaro M, Laugwitz KL, Kastrati A (2014) Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart 100:153–159
Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R (2010) In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol 56:1897–1907
Alfonso F, Byrne RA, Rivero F, Kastrati A (2014) Current treatment of in-stent restenosis. J Am Coll Cardiol 63:2659–2673
Cassese S, Byrne RA, Schulz S, Hoppman P, Kreutzer J, Feuchtenberger A, Ibrahim T, Ott I, Fusaro M, Schunkert H, Laugwitz KL, Kastrati A (2015) Prognostic role of restenosis in 10 004 patients undergoing routine control angiography after coronary stenting. Eur Heart J 36:94–99
Schomig A, Neumann FJ, Kastrati A, Schuhlen H, Blasini R, Hadamitzky M, Walter H, Zitzmann-Roth EM, Richardt G, Alt E, Schmitt C, Ulm K (1996) A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med 334:1084–1089
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, Group ESCSD (2019) 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 40:87–165
Silber S, Albertsson P, Aviles FF, Camici PG, Colombo A, Hamm C, Jorgensen E, Marco J, Nordrehaug JE, Ruzyllo W, Urban P, Stone GW, Wijns W, Task Force for Percutaneous Coronary Interventions of the European Society of C (2005) Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eu Heart J 26:804–847
Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Juni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A (2015) 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). EuroIntervention 10:1024–1094
Antithrombotic Trialists C (2002) Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 324:71–86
Campo G, Tebaldi M, Vranckx P, Biscaglia S, Tumscitz C, Ferrari R, Valgimigli M (2014) Short- versus long-term duration of dual antiplatelet therapy in patients treated for in-stent restenosis: a PRODIGY trial substudy (Prolonging Dual Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia). J Am Coll Cardiol 63:506–512
Tantry US, Bonello L, Aradi D, Price MJ, Jeong YH, Angiolillo DJ, Stone GW, Curzen N, Geisler T, Ten Berg J, Kirtane A, Siller-Matula J, Mahla E, Becker RC, Bhatt DL, Waksman R, Rao SV, Alexopoulos D, Marcucci R, Reny JL, Trenk D, Sibbing D, Gurbel PA, Working Group on On-Treatment Platelet R (2013) Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol 62:2261–2273
Fu Z, Dong W, Shen M, Xue H, Guo J, Jing J, Han Y, Yang X, Chen Y (2014) Relationship between hyporesponsiveness to clopidogrel measured by thrombelastography and in stent restenosis in patients undergoing percutaneous coronary intervention. Clin Biochem 16–17:197–202
Schulz S, Sibbing D, Braun S, Morath T, Mehilli J, Massberg S, Byrne RA, Schomig A, Kastrati A (2010) Platelet response to clopidogrel and restenosis in patients treated predominantly with drug-eluting stents. Am Heart J 160:355–361
Savage MP, Goldberg S, Bove AA, Deutsch E, Vetrovec G, Macdonald RG, Bass T, Margolis JR, Whitworth HB, Taussig A (1995) Effect of thromboxane A2 blockade on clinical outcome and restenosis after successful coronary angioplasty. Multi-Hospital Eastern Atlantic Restenosis Trial (M-HEART II). Circulation 92:3194–3200
Taylor RR, Gibbons FA, Cope GD, Cumpston GN, Mews GC, Luke P (1991) Effects of low-dose aspirin on restenosis after coronary angioplasty. Am J Cardiol 68:874–878
Pamukcu B, Oflaz H, Nisanci Y (2005) The role of platelet glycoprotein IIIa polymorphism in the high prevalence of in vitro aspirin resistance in patients with intracoronary stent restenosis. Am Heart J 149:675–680
Mayer K, Bernlochner I, Braun S, Schulz S, Orban M, Morath T, Cala L, Hoppmann P, Schunkert H, Laugwitz KL, Kastrati A, Sibbing D (2014) Aspirin treatment and outcomes after percutaneous coronary intervention: results of the ISAR-ASPI registry. J Am Coll Cardiol 64:863–871
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW, Academic Research Consortium (2007) Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 115:2344–2351
Le Breton H, Plow EF, Topol EJ (1996) Role of platelets in restenosis after percutaneous coronary revascularization. J Am Coll Cardiol 28:1643–1651
Ip JH, Fuster V, Israel D, Badimon L, Badimon J, Chesebro JH (1991) The role of platelets, thrombin and hyperplasia in restenosis after coronary angioplasty. J Am Coll Cardiol 17:77B-88B
Casscells W (1992) Migration of smooth muscle and endothelial cells. Critical events in restenosis. Circulation 86:723–729
Willerson JT, Yao SK, McNatt J, Benedict CR, Anderson HV, Golino P, Murphree SS, Buja LM (1991) Frequency and severity of cyclic flow alternations and platelet aggregation predict the severity of neointimal proliferation following experimental coronary stenosis and endothelial injury. Proc Natl Acad Sci USA 88:10624–10628
Willerson JT, Eidt JF, McNatt J, Yao SK, Golino P, Anderson HV, Buja LM (1991) Role of thromboxane and serotonin as mediators in the development of spontaneous alterations in coronary blood flow and neointimal proliferation in canine models with chronic coronary artery stenoses and endothelial injury. J Am Coll Cardiol 17:101B-B110
Hermann A, Weber AA, Schror K (2002) Clopidogrel inhibits platelet adhesion and platelet-dependent mitogenesis in vascular smooth muscle cells. Thromb Res 105:173–175
Herbert JM, Tissinier A, Defreyn G, Maffrand JP (1993) Inhibitory effect of clopidogrel on platelet adhesion and intimal proliferation after arterial injury in rabbits. Arterioscler Thromb 13:1171–1179
Urban P, Buller N, Fox K, Shapiro L, Bayliss J, Rickards A (1988) Lack of effect of warfarin on the restenosis rate or on clinical outcome after balloon coronary angioplasty. Br Heart J 60:485–488
Ellis SG, Roubin GS, Wilentz J, Douglas JS Jr, King SB 3rd (1989) Effect of 18- to 24-hour heparin administration for prevention of restenosis after uncomplicated coronary angioplasty. Am Heart J 117:777–782
Serruys PW, Herrman JP, Simon R, Rutsch W, Bode C, Laarman GJ, van Dijk R, van den Bos AA, Umans VA, Fox KA et al (1995) A comparison of hirudin with heparin in the prevention of restenosis after coronary angioplasty. Helvetica Investigators. N Engl J Med 333:757–763
Kastrati A, Schuhlen H, Hausleiter J, Walter H, Zitzmann-Roth E, Hadamitzky M, Elezi S, Ulm K, Dirschinger J, Neumann FJ, Schomig A (1997) Restenosis after coronary stent placement and randomization to a 4-week combined antiplatelet or anticoagulant therapy: six-month angiographic follow-up of the Intracoronary Stenting and Antithrombotic Regimen (ISAR) Trial. Circulation 96:462–467
Serruys PW, Rutsch W, Heyndrickx GR, Danchin N, Mast EG, Wijns W, Rensing BJ, Vos J, Stibbe J (1991) Prevention of restenosis after percutaneous transluminal coronary angioplasty with thromboxane A2-receptor blockade. A randomized, double-blind, placebo-controlled trial. Coronary Artery Restenosis Prevention on Repeated Thromboxane-Antagonism Study (CARPORT). Circulation 84:1568–1580
Schwartz L, Bourassa MG, Lesperance J, Aldridge HE, Kazim F, Salvatori VA, Henderson M, Bonan R, David PR (1988) Aspirin and dipyridamole in the prevention of restenosis after percutaneous transluminal coronary angioplasty. N Engl J Med 318:1714–1719
Stone GW, Witzenbichler B, Weisz G, Rinaldi MJ, Neumann FJ, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri E, Gurbel PA, Xu K, Parise H, Kirtane AJ, Brodie BR, Mehran R, Stuckey TD, Investigators A-D (2013) Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 382:614–623
Funding
Open Access funding enabled and organized by Projekt DEAL. There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Schunkert reports personal fees from MSD SHARP & DOHME, AMGEN, Bayer Vital GmbH, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Servier, Brahms, Bristol-Myers Squibb, Medtronic, Sanofi Aventis and Synlab, grants from Astra-Zeneca, outside the submitted work. Prof. Sibbing reports personal fees from Bayer AG, Sanofi Aventis, Astra Zeneca, Pfizer, grants and personal fees from Roche Diagnostics, personal fees from Ferrer and Daiichi Sankyo, outside the submitted work. Prof. Schüpke reports grants from the Else Kröner Fresenius Stiftung (Else Kröner Memorial Sipendium), grants from the German Center for Cardiovascular Research (DZHK) for the ISAR-REACT 5 trial, personal fees from Bayer Vital GmbH, outside the submitted work. Dr. Bernlochner reports personal fees from Sysmex Europe GmbH, outside the submitted work. The other authors have no conflict of interest to declare.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mayer, K., Ndrepepa, G., Schroeter, M. et al. High on-aspirin treatment platelet reactivity and restenosis after percutaneous coronary intervention: results of the Intracoronary Stenting and Antithrombotic Regimen-ASpirin and Platelet Inhibition (ISAR-ASPI) Registry. Clin Res Cardiol 112, 1231–1239 (2023). https://doi.org/10.1007/s00392-023-02161-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-023-02161-z