Abstract
Background
Exercise training in heart failure (HF) is recommended but not routinely offered, because of logistic and safety-related reasons. In 2020, the German Society for Prevention&Rehabilitation and the German Society for Cardiology requested establishing dedicated “HF training groups.” Here, we aimed to implement and evaluate the feasibility and safety of one of the first HF training groups in Germany.
Methods
Twelve patients (three women) with symptomatic HF (NYHA class II/III) and an ejection fraction ≤ 45% participated and were offered weekly, physician-supervised exercise training for 1 year. Patients received a wrist-worn pedometer (M430 Polar) and underwent the following assessments at baseline and after 4, 8 and 12 months: cardiopulmonary exercise test, 6-min walk test, echocardiography (blinded reading), and quality of life assessment (Kansas City Cardiomyopathy Questionnaire, KCCQ).
Results
All patients (median age [quartiles] 64 [49; 64] years) completed the study and participated in 76% of the offered 36 training sessions. The pedometer was worn ≥ 1000 min per day over 86% of the time. No cardiovascular events occurred during training. Across 12 months, NT-proBNP dropped from 986 pg/ml [455; 1937] to 483 pg/ml [247; 2322], and LVEF increased from 36% [29;41] to 41% [32;46]%, (p for trend = 0.01). We observed no changes in exercise capacity except for a subtle increase in peak VO2% predicted, from 66.5 [49; 77] to 67 [52; 78]; p for trend = 0.03. The physical function and social limitation domains of the KCCQ improved from 60 [54; 82] to 71 [58; 95, and from 63 [39; 83] to 78 [64; 92]; p for trend = 0.04 and = 0.01, respectively. Positive trends were further seen for the clinical and overall summary scores.
Conclusion
This pilot study showed that the implementation of a supervised HF-exercise program is feasible, safe, and has the potential to improve both quality of life and surrogate markers of HF severity. This first exercise experiment should facilitate the design of risk-adopted training programs for patients with HF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Germany, the concept of ambulatory “cardiac training groups” (HSGs, Herzsportgruppen) supervised by a physician with emergency equipment and an experienced exercise physiologist was initiated and implemented as early as 1965. The HSGs aimed to safely enable patients with cardiac diseases to regain their neuromuscular and cardiovascular performance after a cardiac event, predominantly after a myocardial infarction [1]. Since then, more than 6,000 HSGs have been founded in Germany offering structured exercise training available on prescription [2].
Despite well-established evidence and guidelines recommending physical activity to improve health-related quality of life and to reduce hospitalization rates in patients with heart failure, their participation in the above-mentioned HSGs is heavily underrepresented, most likely because of their perceived higher risk for cardiovascular events during training sessions [3,4,5]. However, multiple studies over the last three decades consistently reported that the risk of events like sudden cardiac death, cardiac arrest, or myocardial infarction in exercising patients with cardiovascular diseases was small, and progressively diminished over the years [6]. Nevertheless, heart failure patients carry a higher baseline risk, which might be particularly increased for unfit or previously sedentary patients performing uncontrolled or even vigorous (un-)supervised training [7]. Therefore, and complementary to established HSGs, the German Society for Prevention and Rehabilitation and the German Society for Cardiology in 2020 claimed the establishment of dedicated “Heart Failure Training Groups” for patients with heart failure and limited exercise capacity, who cannot participate in conventional HSGs [6, 8].
The current prospective pilot study aimed to scientifically follow one of the very first heart failure training groups founded in Germany, examine its feasibility and safety, and investigate its effects on exercise capacity and quality of life in the time course of one year.
Methods
Study population
Between November 2018 and May 2019, 12 ambulatory patients with chronic heart failure were enrolled into the “HIP-in-Würzburg” pilot study, a non-randomized, monocentric, prospective cohort study. Adult patients were eligible if they had symptomatic heart failure (New York Heart Association functional class II or III) with a reduced left ventricular ejection fraction (LVEF) below 45%, and were physically and mentally capable of and willing to participate in a weekly training program. The study was conducted according to the Good Clinical Practice guidelines and the Declaration of Helsinki principles of 2002, and was approved by the responsible ethic committee of Würzburg, Germany (221/18-sc). All patients provided written informed consent.
Patient assessment
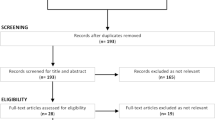
Study flow. All patients underwent a standardized clinical evaluation including assessment of medical history, quality of life (Kansas City Cardiomyopathy Questionnaire; KCCQ), and depressed mood (Patient Health Questionnaire; PHQ-9). Venous blood was sampled for routine cardiovascular markers. Additional investigations included a 12-lead resting electrocardiogram (ECG), standardized echocardiography, a 6-min walk test (6MWT), and a cardiopulmonary exercise test (CPET). All investigations were performed in identical fashion by trained staff at baseline and after 4, 8, and 12 months of follow-up.
Questionnaires
Both questionnaires were completed by the patients themselves, i.e., without interference of relatives or staff, at baseline and at each follow-up visit. Depressive symptoms were assessed by the validated German version of the PHQ-9 questionnaire that consists of nine questions, each one indexed with 0 to 3 points [9]. A total PHQ-9 sum score of 10 or above suggests the presence of depression [10]. Disease-specific quality of life was assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ), a 23-item, self-administered instrument that quantifies six domains (physical limitation, symptom frequency and stability, self-efficacy, social limitation, and quality of life) [11]. The items are further aggregated to the sum-scales “functional status” (physical limitation, symptom frequency and stability) and overall summary score (all items except self-efficacy and symptom stability). The scores are transformed to a 0-to-100-point scale, where lower scores represent more severe symptoms or limitations and scores of 100 indicate no symptoms, no limitations, and excellent quality of life [11, 12].
Echocardiography was performed according to practice guidelines by a certified echo technician [13] and focused on the following measurements: left ventricular systolic function (LVEF, assessed either by the biplane-modified Simpson method or visually by eye balling in the apical four-chamber view, in cases of poor ultrasound condition), left atrial diameter measured at the end-systole (LADs), left ventricular end-diastolic diameter (LVEDD), septal and posterior wall diameter, diastolic dysfunction (ratio E/A, E/e’, deceleration time), and presence of valvular disease. The LVEF measurements were re-assessed by an independent certified sonographer (FS), who was blinded to patient name, history, and follow-up time point.
Six-minute walk test (6MWT)
The 6MWT measures the distance a patient covers walking quickly on a flat, hard surface for 6 min. This submaximal exercise test was first validated in heart failure in 1985, and shows a very good correlation with NYHA functional class, bicycle ergometry and other parameters of physical functioning in patients with heart failure [14, 15]. The test was performed by experienced staff on a dedicated 20-m walkway in outpatient clinics under standardized conditions.
Cardiopulmonary exercise testing (CPET)
Serial spiroergometry was performed on the treadmill or bicycle ergometer according to the preference of the patient, and the following standard parameters were assessed: heart rate, blood pressure, minute ventilation (VE), respiratory exchange ratio (RER), maximal oxygen consumption (peakVO2) respiratory equivalent for oxygen (EqO2) and carbon dioxide (EqCO2). The type of CPET exercise procedure remained constant during the course of the study. A ramp protocol was used and gradually increased until physical exhaustion or achievement of termination criteria suggested by current guidelines [16].Before and immediately after exercise testing, capillary blood gas analysis was performed with assessment of standard parameters: pH, lactate, base excess, partial pressure of O2 (pO2) and CO2 (pCO2).
Training program and activity monitor
Group sessions
Patients met once per week as an additional group, i.e., separate from patients participating in the conventional cardiac training program. Before each training session, blood pressure, pulse and body mass were assessed in each patient. A certified HSG instructor offered an individualized training program to each participant with exercise intensity based on information derived from the baseline CPET. Patients were equipped with a heart rate monitor and activity tracker (Polar M430, Polar Electro Oy, Kempele, Finland), and were encouraged to adjust their training intensity according to the target heart rate (determined by means of CPET at 70% of peakVO2 ± 10 beats per minute). The information derived from the follow-up CPET was applied to adjust the target heart rate. In general, a moderate training intensity (11–13 on Borg’s 6–20 scale) was targeted [17]. Each training session lasted 60 min. The aim of each session was to improve muscular strength, endurance and coordination, as well as self-perception. The training consisted of the modules described in Table 1.
Activity monitor
Daily step counts were collected to monitor physical activity behavior during waking hours. As patients had to get used to wearing and using the watch, the first interval for step count monitoring covered four weeks (“run-in-phase,” and patients were followed up at month four (FUP4), eight (FUP8) and 12 (FUP12). The analysis comprise of the data consisting for at least 600 min between 06:00 and 22:00 per day, and 1000 min per 24-h period in total.
Training at home
All patients were iteratively encouraged to increase their daily activity level, i.e., to observe their daily step count and also to exercise on days with no group meetings. The supervising physician set individual goals for home training, e.g., a 10% increase in the daily step. Depending on the patient’s success, further increase or reduction was advised to ensure motivation. Patients walking more than 10,000 steps per day were advised to include other exercising activities such as jogging, walking, or bike riding with heart rate control. Patients feeling unwell were advised to stop training at home. Each patient received weekly reports of the daily step count and activity level.
Clinical endpoints
The primary endpoint was defined as the 12-month change in peakVO2 at CPET. Secondary endpoints evaluated the safety of the training program (frequency of cardiovascular events as heart failure hospitalization and cardiovascular deaths during follow-up), changes over time in the distance walked during the 6MWT, as well as domains of quality of life, and improvements in echocardiographic and laboratory markers of heart failure. The incidence of cardiovascular events as heart failure hospitalization and cardiovascular deaths was also assessed. Owing to the pilot character of the study, no formal sample size calculation and power analysis were performed.
Data analysis
Continuous variables are reported as mean (standard deviation) or median (quartiles), and categorical variables as absolute and relative frequencies. Trend tests for continuous variables from a single sample were calculated with Page´s rank trend test in R [18]. For binary variables, two analyses were combined [18, 19]. First, for each individual the slope was calculated from the course of the binary data over time. For instance, the slope was regarded as positive/negative if the values increased (e.g., 0–1-1–1 or 0–0-1–1 etc.) or decreased (e.g., 1–1-1–0; 1–1-0–0 etc.) over time. If the values remained unaltered over time, the slope was zero. Then, a one-sample Wilcoxon rank test was performed, to ascertain whether slopes differed from zero. As trend tests require complete data sets, missing values (up to 1 per variable) were imputed through missing value analysis with linear interpolation [20]. For binary variables, the last value was carried forward. All p-values are two-sided and are considered exploratory by nature.
Results
Study population and adherence to study procedures
A total of 12 patients were recruited for this pilot study. Their characteristics are summarized in Table 2, and those of the entire group are in Table 3. The median age of the participants was 64 years (49; 73), 25% were female, 33% had ischemic cardiomyopathy, 59% were in NYHA functional class III, and 75% exhibited heart failure with reduced ejection fraction. At study start, 83% received pharmacotherapy fully compliant with current guidelines [3]. At each study visit, heart failure medication was re-checked and optimized whenever possible and all completed the study after 12 months. Only one patient had missed one follow-up visit (8-month visit), otherwise, follow-up was complete. In total, 36 training sessions could be offered within 12 months, and the average participation rate was 76% (range 49–92%). The last recruited patient (pt. #12) was only offered 30 training units, because of the COVID-19 pandemic-induced lockdown in Germany in March 2020.
Safety
During training sessions, no cardiac or any other adverse events occurred. During 12 months of follow-up, three patients (pts. #4, #7, #11) were hospitalized due to causes unrelated to training. Patient #4 experienced ventricular tachycardia/fibrillation and was shocked multiple times by his implanted cardioverter-defibrillator (ICD). An acute coronary syndrome could be excluded, but coronary angiography revealed progression of his underlying multi-vessel coronary artery disease. Patient #7 was hospitalized twice, once to exclude progression of his coronary artery disease and once for tachyarrhythmia, necessitating electrical cardioversion. Patient #9 was also hospitalized twice, once for implantation of a subcutaneous ICD and once for cardiac decompensation. Of note, 12 months prior to inclusion into the study, five out of the 12 patients had been hospitalized for various reasons: pt. #1 twice, first for elective right heart catheterization and then for cardiac decompensation; pt. #2 twice, for myocardial biopsy and for exclusion of acute coronary syndrome; pt. #4 for angina pectoris necessitating stent implantation; pt. #8 was admitted six times in total, three times for cardiac decompensation, once for right heart catheterization, once for MitraClip® implantation, and once for transplant evaluation; pt. #12 was admitted for heart transplant evaluation.
Pharmacotherapy of heart failure, biomarkers, and surrogates of heart failure severity
At baseline, 10 out of 12 patients received optimal medical therapy (OMT) according to the then-current ESC guidelines [3]. During follow-up, heart failure medication was further optimized: In one patient, beta-blocker was started and well tolerated; in three patients, ACEi/ARB changed to angiotensin receptor neprilysin inhibitor (ARNI), thus at the 12-month follow-up, eight patients were receiving ARNI (p for trend = 0.17). At the end of the study, all patients were on OMT (p for trend = 0.35; Table 4).
Despite no apparent changes in lipid lowering medication, total cholesterol and LDL cholesterol decreased from baseline to the end of the study (p for trend = 0.01 and 0.02; Table 5), whereas HDL cholesterol remained unaffected. Changes in NYHA functional class were nominally favorable but yielded no significant trend (Fig. 1 and Table 5). Subtle, yet significant improvements were further observed during follow-up for NT-proBNP levels (p for trend 0.01), and LVEF (p for trend < 0.01),
Quality of life and mood
The KCCQ clinical and overall summary score both had improved nominally after 12 months (p for trend = 0.05 and = 0.09, respectively: Table 5). A significant improvement in physical function and social limitation was observed across the 12-month period (p for trend = 0.04 and = 0.01, respectively). By contrast, all other subscales were not materially altered over time (Table 5). Depressive mood, as assessed by the PHQ-9 summary score, was unchanged during follow-up.
Exercise capacity
Exercise capacity was very heterogeneously distributed in the study sample at baseline, with median peakVO2 14.0 ml/min/kg (quartiles 10.7, 17.7: for details refer to Fig. 2). During follow-up, peakVO2 and peakVO2% of predicted tended to rise after 4 months and 8 months, but this increase was not consistently observed after 12 months (p for trend for both = 0.03; Table 5). The other CPET parameters did not change substantially (best p = 0.10; Table 5). Walking distance in the 6-min walking test increased 2.2–4.4%, but not significantly (p = 0.11). Daily step count and activity time, did not change over time (Fig. 3 and Table 5; p = 0.11 and p = 0.22, respectively). The wrist-worn pedometer was well tolerated and worn in over 86% of days at least 1000 min.
Discussion
The current non-randomized pilot study aimed to assess the safety, efficacy, and feasibility of an activity-monitored, physician-supported, dedicated training group for patients with heart failure. During a follow-up-time of 12 months, no training-associated events occurred; hospitalization rate was lower than the year prior to the study, and patients adhered reasonably well to the suggested time schedules (76% adherence to offered training sessions). Quantitative parameters measuring exercise capacity did not improve consistently, but amongst markers of wellbeing and heart failure severity some positive trends emerged regarding NT-proBNP levels, LVEF, and quality of life.
Physician-supported ambulatory training groups for patients with heart diseases, predominantly coronary artery disease, have a long tradition in Germany [1]. In contrast, patients with symptomatic heart failure were often excluded as their participation was considered unsafe, despite lacking data supporting such a notion, and despite opposite and strong recommendations from national and international guidelines [3, 21]. Only recently (January 2020) has this large patient group been specifically addressed in a position paper of the German Cardiac Society, which made a request to implement dedicated heart failure training groups in Germany. Meanwhile, a respective reimbursement scheme for heart failure training groups has been approved, which allow for the higher supervision efforts compared to conventional HSGs [6]. Due to the COVID-19 induced lockdown, uptake of heart failure training groups has been poor, thus experiences with and evidence arising from heart failure training groups are still sparse. The “HIP-in-Würzburg study” started in November 2018 before the position paper was published, and ended in March 2020. Thus, the study was largely unaffected by the pandemic regulations except for the last patient, who terminated the study 2 months earlier than intended.
Previous studies in inpatients and outpatients with heart failure showed multiple benefits of exercise on cardiovascular outcome, quality of life, rehospitalization rate and—in longer-term studies—even mortality [22,23,24,25,26,27]. Although the positive effects on hard clinical endpoints were modest and not consistently reproducible, no major negative effects of physical exercise in heart failure have yet became apparent, and benefits are thought to outweigh the risks by far [3, 21]. In our study, no patient died during follow-up, and the number of hospitalizations was lower than the year prior to study entry. Of course, due to the natural progression of the disease, rhythm disturbances, hospitalizations, and other cardiovascular events may occur independently from the exercise training and more frequently than in healthier heart conditions. Hence, they should not necessarily lead to a discontinuation of training sessions [28, 29]. Physician-guided training might be of even of higher importance in patients with advanced heart diseases than in healthier cardiovascular subjects attending the conventional HSGs [6].
There is a discussion about which training modality is superior for patients with heart failure [30]. According to current recommendations, we chose a combination of endurance and strength training, as this combination is supposed to increase exercise capacity most effectively in this patient group [31, 32]. Exercise capacity is an acknowledged indicator of better prognosis in heart failure; hence, it is a central surrogate of the success of training programs [33]. In our analysis, we did not observe meaningful and consistent improvements in exercise capacity, derived by CPET, 6MWT or the activity indices. However, our pilot study was not statistically powered to detect such changes. Further, the baseline cardiovascular fitness level assessed peakVO2 was very heterogeneous amongst participants, ranging from 9 ml/min/kg to up to 26 ml/min/kg. Although we intended to provide an individualized training program, the fitter patients might have benefitted from greater exercise intensity, duration and/or frequency of training sessions and therefore may have been under-challenged by our training settings. Thus, selection of patients according to their physical capacity applying a stress test rather than simplistically relying on ejection fraction or NYHA functional class might be key in ensuring less heterogenous group composition and therefore more efficient training results. An increase in LVEF has also been observed in other studies examining the effect of exercise training [34]. Of note, we observed a few relevant changes in heart failure medication as three patients were switched from ACEi/ARB to ARNI during follow-up and one patient received ivabradine additionally. Our study lacked the statistical power to judge on the associated consequences of the adjusted medication.
Benefits in quality of life have been frequently reported in training studies in heart failure [35], and could be partially observed in this pilot study. We found a significant increase in the KCCQ physical function and social limitation domain and respective trends for the overall and clinical summary scores. The observed increments of about 10 score points are clinically relevant [36], and underscore the potential of structured exercise programs in this vulnerable patient group.
Limitations and strengths
The current pilot study was not powered, either in size or duration, to allow for reliable conclusions concerning the efficacy of heart failure training groups. However, we were able to evaluate the feasibility of weekly offered heart failure training groups in real life. In particular, positive secondary findings of such a regular schedule became apparent, including improved adherence and the optimization of guideline-recommended drug treatment. Further, patients in our study sample differed in several points from patients considered eligible for participation in heart failure training groups by the position paper (i.e., LVEF < 40%, NYHA functional class III, etc. [6].). The optimal criteria for group composition still need to be clarified. Further, equipping heart failure patients with a smartwatch including pedometer function might be an appealing method to track patients and motivate them to increase their individual daily activity. However, most patients with heart failure are elderly and not familiar with such advanced technology. Thus, proper handling of a smartwatch might have been an issue in our study, and a simple pedometer might have been more reliable.
Conclusion
In conclusion, the current pilot study found that the concept of a dedicated heart failure training group was feasible, safe, and yielded improved quality of life and symptoms burden over a 12-months period. Participation in such training groups should be offered to all patients with heart failure who are not confident to participate in HSGs. Our experiences and considerations could be used to establish local heart failure training groups and will inform future trials.
Availability of data and material
The submitted work is original and has not been published elsewhere in any form or language (neither partially nor in full).
Code availability
Not applicable.
References
Graf C, Bjarnason-Wehrens B, Löllgen H (2004) Outpatient Cardiac Rehabilitation Groups in Germany - Retrospect and Prospects. DEUTSCHE ZEITSCHRIFT FÜR SPORTMEDIZIN 55(12):339–346
Bjarnason-Wehrens B, Held K, Karoff M (2006) Heart groups in Germany-current situation and prospects. Herz 31(6):559–565. https://doi.org/10.1007/s00059-006-2870-2
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force M, Document R (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975. https://doi.org/10.1002/ejhf.592
Bjarnason-Wehrens B, Nebel R, Jensen K, Hackbusch M, Grilli M, Gielen S, Schwaab B, Rauch B, German Society of Cardiovascular P, Rehabilitation (2020) Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): a systematic review and meta-analysis. Eur J Prev Cardiol 27(9):929–952. https://doi.org/10.1177/2047487319854140
Franklin BA, Thompson PD, Al-Zaiti SS, Albert CM, Hivert MF, Levine BD, Lobelo F, Madan K, Sharrief AZ, Eijsvogels TMH, American Heart Association Physical Activity Committee of the Council on L, Cardiometabolic H, Council on C, Stroke N, Council on Clinical C, Stroke C (2020) Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective-an update: a scientific statement From the American Heart Association. Circulation 141(13):e705–e736. https://doi.org/10.1161/CIR.0000000000000749
Wienbergen H, Schwaab B, Bjarnason-Wehrens B, Guha M, Laszlo R, Burgstahler C, von Haehling S, Halle M, Zahn R, Hambrecht R (2020) Position paper of the German Cardiac Society (DGK) in cooperation with the German Society for Prevention and Rehabilitation of Cardiovascular Diseases (DGPR)—Physician support for outpatient cardiac rehabilitation groups. Kardiologe. https://doi.org/10.1007/s12181-020-00433-w
Maron BJ (2000) The paradox of exercise. N Engl J Med 343(19):1409–1411. https://doi.org/10.1056/NEJM200011093431911
Brüggemann I, Guha M (2019) Herzgruppen für Patienten mit hohem kardiovaskulärem Ereignisrisiko––Herzinsuffizienzgruppen. Diabetes, Stoffwechsel und Herz 28(4):218–221
Rief W, Nanke A, Klaiberg A, Braehler E (2004) Base rates for panic and depression according to the Brief Patient Health Questionnaire: a population-based study. J Affect Disord 82(2):271–276. https://doi.org/10.1016/j.jad.2003.11.006
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Green CP, Porter CB, Bresnahan DR, Spertus JA (2000) Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol 35(5):1245–1255. https://doi.org/10.1016/s0735-1097(00)00531-3
Spertus JA, Jones PG, Sandhu AT, Arnold SV (2020) Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care: JACC State-of-the-Art Review. J Am Coll Cardiol 76(20):2379–2390. https://doi.org/10.1016/j.jacc.2020.09.542
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270. https://doi.org/10.1093/ehjci/jev014
Uszko-Lencer N, Mesquita R, Janssen E, Werter C, Brunner-La Rocca HP, Pitta F, Wouters EFM, Spruit MA (2017) Reliability, construct validity and determinants of 6-minute walk test performance in patients with chronic heart failure. Int J Cardiol 240:285–290. https://doi.org/10.1016/j.ijcard.2017.02.109
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB (1985) The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 132(8):919–923
Albouaini K, Egred M, Alahmar A, Wright DJ (2007) Cardiopulmonary exercise testing and its application. Heart 93(10):1285–1292. https://doi.org/10.1136/hrt.2007.121558
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Bortz JLG, Boehnke K (1990) Verteilungsfreie Methoden in der Biostatistik. Springer, Berlin - Heidelberg
Lautsch EL, G. A. (1993) Binärdatenanalyse für Psychologen. Psychologie Verlags Union, Weinheim, Mediziner und Sozialwissenschaftler
Bortz J, Döring N (1995) Forschungsmethoden und Evaluation. Springer, Heidelberg
Bundesärztekammer BK (2019) Nationale Versorgungsleitlinie Chronische Herzinsuffizizienz, 3.Auflage. AWMF-Register-Nr: nvl-006. https://doi.org/10.6101/AZQ/000465
Taylor RS, Walker S, Smart NA, Piepoli MF, Warren FC, Ciani O, O’Connor C, Whellan D, Keteyian SJ, Coats A, Davos CH, Dalal HM, Dracup K, Evangelista L, Jolly K, Myers J, McKelvie RS, Nilsson BB, Passino C, Witham MD, Yeh GY, Zwisler AO, ExTra MIIC (2018) Impact of exercise-based cardiac rehabilitation in patients with heart failure (ExTraMATCH II) on mortality and hospitalisation: an individual patient data meta-analysis of randomised trials. Eur J Heart Fail 20(12):1735–1743. https://doi.org/10.1002/ejhf.1311
van der Meer S, Zwerink M, van Brussel M, van der Valk P, Wajon E, van der Palen J (2012) Effect of outpatient exercise training programmes in patients with chronic heart failure: a systematic review. Eur J Prev Cardiol 19(4):795–803. https://doi.org/10.1177/1741826711410516
Taylor RS, Long L, Mordi IR, Madsen MT, Davies EJ, Dalal H, Rees K, Singh SJ, Gluud C, Zwisler AD (2019) Exercise-Based Rehabilitation for Heart Failure: Cochrane Systematic Review, Meta-Analysis, and Trial Sequential Analysis. JACC Heart Fail 7(8):691–705. https://doi.org/10.1016/j.jchf.2019.04.023
Piepoli MF, Davos C, Francis DP, Coats AJ, ExTra MC (2004) Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ 328(7433):189. https://doi.org/10.1136/bmj.37938.645220.EE
Mediano MFF, Leifer ES, Cooper LS, Keteyian SJ, Kraus WE, Mentz RJ, Fleg JL (2018) Influence of baseline physical activity level on exercise training response and clinical outcomes in heart failure: the HF-ACTION Trial. JACC Heart Fail 6(12):1011–1019. https://doi.org/10.1016/j.jchf.2018.09.012
Patti A, Merlo L, Ambrosetti M, Sarto P (2021) Exercise-Based Cardiac Rehabilitation Programs in Heart Failure Patients. Heart Fail Clin 17(2):263–271. https://doi.org/10.1016/j.hfc.2021.01.007
Tenenbaum A, Freimark D, Ahron E, Koren-Morag N, Schwamenthal E, Fisman EZ, Shechter M, Tanne D, Kachlon D, Motro M, Adler Y (2006) Long-term versus intermediate-term supervised exercise training in advanced heart failure: effects on exercise tolerance and mortality. Int J Cardiol 113(3):364–370. https://doi.org/10.1016/j.ijcard.2005.11.098
Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. Nat Rev Cardiol 8(1):30–41. https://doi.org/10.1038/nrcardio.2010.165
Cornelis J, Beckers P, Taeymans J, Vrints C, Vissers D (2016) Comparing exercise training modalities in heart failure: a systematic review and meta-analysis. Int J Cardiol 221:867–876. https://doi.org/10.1016/j.ijcard.2016.07.105
Gomes-Neto M, Duraes AR, Conceicao LSR, Roever L, Silva CM, Alves IGN, Ellingsen O, Carvalho VO (2019) Effect of combined aerobic and resistance training on peak oxygen consumption, muscle strength and health-related quality of life in patients with heart failure with reduced left ventricular ejection fraction: a systematic review and meta-analysis. Int J Cardiol 293:165–175. https://doi.org/10.1016/j.ijcard.2019.02.050
Miche E, Roelleke E, Wirtz U, Zoller B, Tietz M, Huerst M, Radzewitz A (2008) Combined endurance and muscle strength training in female and male patients with chronic heart failure. Clin Res Cardiol 97(9):615–622. https://doi.org/10.1007/s00392-008-0660-y
Williams MA, Pozehl B (2015) Reasonable expectations: how much aerobic capacity, muscle strength, and quality of life can improve with exercise training in heart failure. Heart Fail Clin 11(1):37–57. https://doi.org/10.1016/j.hfc.2014.08.003
Tucker WJ, Beaudry RI, Liang Y, Clark AM, Tomczak CR, Nelson MD, Ellingsen O, Haykowsky MJ (2019) Meta-analysis of exercise training on left ventricular ejection fraction in heart failure with reduced ejection fraction: a 10-year update. Prog Cardiovasc Dis 62(2):163–171. https://doi.org/10.1016/j.pcad.2018.08.006
Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, Fine LJ, Howlett JG, Keteyian SJ, Kitzman DW, Kraus WE, Miller NH, Schulman KA, Spertus JA, O’Connor CM, Weinfurt KP, Investigators H-A (2009) Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301(14):1451–1459. https://doi.org/10.1001/jama.2009.457
Spertus J, Peterson E, Conard MW, Heidenreich PA, Krumholz HM, Jones P, McCullough PA, Pina I, Tooley J, Weintraub WS, Rumsfeld JS, Cardiovascular Outcomes Research C (2005) Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J 150(4):707–715. https://doi.org/10.1016/j.ahj.2004.12.010
Stevens LA, Coresh J, Greene T, Levey AS (2006) Assessing kidney function–measured and estimated glomerular filtration rate. N Engl J Med 354(23):2473–2483. https://doi.org/10.1056/NEJMra054415
Acknowledgements
We thank all our patients for participation into the HIP-in-Würzburg study. Further the trainers and physicians of the Sportbund DJK training center Würzburg for the excellent supervision and care during the training sessions, and the Sportbund DJK training center Würzburg for providing the premises.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Comprehensive Heart Failure Center funded by the German Federal Ministry of Education and Research [Bundesministerium für Bildung und Forschung (BMBF)] with the grant number: 01EO1504.
Author information
Authors and Affiliations
Contributions
GG and JW performed statistical analyses and wrote the manuscript. JW, NS CR, CM, MB, FS collected the data and contributed significant intellectual content to the manuscript. RL, PD, BS processed the smart watch data and contributed significant intellectual content to the manuscript. CR, BS, SS and MB designed the study. SF and SS were instrumental for grant application and contributed significant intellectual content to the manuscript. US performed and supervised statistical analyses. SS performed statistical analyses, wrote the manuscript and supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
GG received grant support from the Federal Ministry of Education and Research, The German Heart Foundation, the German Society for Cardiology and has been a consultant for AstraZeneca, Abiomed, Bayer, Boehringer Ingelheim, Novartis, Orion GmbH, Pfizer and Vifor, all outside of the current study. BS received funding for a previous exercise study from Polar. CM reports research cooperation with the University of Würzburg and Tomtec Imaging Systems funded by a research grant from the Bavarian Ministry of Economic Affairs, Regional Development and Energy, Germany; advisory and speakers honoraria as well as travel grants from AKCEA, Alnylam, Amgen, Boehringer Ingelheim, EBR Systems Orion Pharma, Pfizer, SOBI, and Tomtec; principal investigator in trials sponsored by Alnylam and AstraZeneca; financial support from the interdisciplinary center for clinical research - IZKF Würzburg, all outside this current study. SF received grant support from the German Research Foundation, the BMBF and has been a consultant for Abiomed, Amgen, Akzea, AstraZeneca, Bayer, Berlin-Chemie, Biotronik, Braun, Bristol-Myers Squibb, Boehringer, Daiichi Sankyo, Medtronic, MSD, Novartis, Novonordisk, Pfizer, Sanofi-Aventis, Servier, Siemens, Vifor, and Zoll - all outside of the current study. SS received grant support from the Federal Ministry of Education and Research, The German Heart Foundation, the German Society for Cardiology and has participated in trials conducted by or has been a consultant for Akcea, AstraZeneca, Bayer, Boehringer Ingelheim, IONIS, Novartis, Pfizer, Sanofi, Vifor, all outside of the current study. All other authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
The study was approved by the responsible ethic committee of Würzburg, Germany (221/18-sc).
Consent to Participate
All patients were adults and provided written informed consent to participate to the study.
Consent for publication
Written informed consent for publication of their clinical data was obtained from all patients before study inclusion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Güder, G., Wilkesmann, J., Scholz, N. et al. Establishing a cardiac training group for patients with heart failure: the “HIP-in-Würzburg” study. Clin Res Cardiol 111, 406–415 (2022). https://doi.org/10.1007/s00392-021-01892-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01892-1