Abstract
Background
Cardiac arrhythmias and sleep-disordered breathing (SDB) are common comorbidities in heart failure with reduced ejection fraction (HFrEF). However, understanding of the association between arrhythmias and SDB is poor. This study assessed the occurrence and circadian distribution of ventricular arrhythmias in HFrEF patients with and without SDB.
Methods
This retrospective analysis included HFrEF patients admitted for unattended overnight cardiorespiratory polygraphy and 24-h Holter-ECG recording. Holter-ECG data (events/h) were categorized by time of day: morning, 06:00–13:59; afternoon, 14:00–21:59; nighttime, 22:00–05:59. Respiratory events were expressed using the apnea–hypopnea index (AHI) and an AHI ≥ 15/h was categorized as moderate to severe SDB.
Results
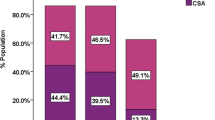
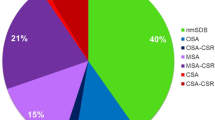
167 patients were included (82% male, age 65 ± 10.4 years, left ventricular ejection fraction 30.9 ± 7.9%); SDB was predominantly central sleep apnea (CSA) in 45.5%, obstructive sleep apnea (OSA) in 23.9% or none/mild (nmSDB) in 17.4%. Morning premature ventricular contractions (PVCs) were detected significantly more frequently in CSA versus nmSDB patients (44.4/h versus 1.8/h; p = 0.02). Non-sustained VT was more frequent in patients with CSA versus versus OSA or nmSDB (17.9 versus 3.2 or 3.2%/h; p = 0.003 and p = 0.005, respectively). There was no significant variation in VT occurrence by time of day in HFrEF patients with CSA (p = 0.3). CSA was an independent predictor of VT occurrence in HFrEF in multivariate logistic regression analysis (odds ratio 4.1, 95% confidence interval 1.5–11.4, p = 0.007).
Conclusion
CSA was associated with VT occurrence irrespective of sleep/wake status in HFrEF patients, and independently predicted the occurrence of VT. This association may contribute to chances by which CSA increases sudden death risk in HFrEF patients.





Similar content being viewed by others
References
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Topfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9:251–257. https://doi.org/10.1016/j.ejheart.2006.08.003
Arzt M, Woehrle H, Oldenburg O, Graml A, Suling A, Erdmann E, Teschler H, Wegscheider K, Schla HFI (2016) Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC Heart Fail 4:116–125. https://doi.org/10.1016/j.jchf.2015.09.014
Fox H, Purucker HC, Holzhacker I, Tebtmann U, Bitter T, Horstkotte D, Graml A, Woehrle H, Oldenburg O (2016) Prevalence of sleep-disordered breathing and patient characteristics in a coronary artery disease cohort undergoing cardiovascular rehabilitation. J Cardiopulm Rehabil Prev 36:421–429. https://doi.org/10.1097/HCR.0000000000000192
Koehler U, Kesper K, Timmesfeld N, Grimm W (2016) Cheyne-Stokes respiration in patients with heart failure. Int J Cardiol 203:775–778. https://doi.org/10.1016/j.ijcard.2015.11.054
Basic K, Fox H, Spiesshofer J, Bitter T, Horstkotte D, Oldenburg O (2016) Improvements of central respiratory events, Cheyne-Stokes respiration and oxygenation in patients hospitalized for acute decompensated heart failure. Sleep Med 27–28:15–19. https://doi.org/10.1016/j.sleep.2016.10.006
Javaheri S, Shukla R, Zeigler H, Wexler L (2007) Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol 49:2028–2034. https://doi.org/10.1016/j.jacc.2007.01.084
Serizawa N, Yumino D, Kajimoto K, Tagawa Y, Takagi A, Shoda M, Kasanuki H, Hagiwara N (2008) Impact of sleep-disordered breathing on life-threatening ventricular arrhythmia in heart failure patients with implantable cardioverter-defibrillator. Am J Cardiol 102:1064–1068. https://doi.org/10.1016/j.amjcard.2008.05.057
Khayat R, Jarjoura D, Porter K, Sow A, Wannemacher J, Dohar R, Pleister A, Abraham WT (2015) Sleep disordered breathing and post-discharge mortality in patients with acute heart failure. Eur Heart J 36:1463–1469. https://doi.org/10.1093/eurheartj/ehu522
Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U, Horstkotte D, Wegscheider K (2016) Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J 37:1695–1703. https://doi.org/10.1093/eurheartj/ehv624
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H (2015) Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med 373:1095–1105. https://doi.org/10.1056/NEJMoa1506459
Oldenburg O, Arzt M, Börgel J, Penzel T, Skobel CE, Fox H, Schöbel C, Bitter T, Stellbrink C (2017) Addendum zum Positionspapier “Schlafmedizin in der Kardiologie. Update 2014”. Somnologie 21:51–52. https://doi.org/10.1007/s11818-017-0104-x
Eulenburg C, Wegscheider K, Woehrle H, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H, Cowie MR (2016) Mechanisms underlying increased mortality risk in patients with heart failure and reduced ejection fraction randomly assigned to adaptive servoventilation in the SERVE-HF study: results of a secondary multistate modelling analysis. Lancet Respir Med 4:873–881. https://doi.org/10.1016/S2213-2600(16)30244-2
Linz D, Fox H, Bitter T, Spiesshofer J, Schobel C, Skobel E, Turoff A, Bohm M, Cowie MR, Arzt M, Oldenburg O (2016) Impact of SERVE-HF on management of sleep disordered breathing in heart failure: a call for further studies. Clin Res Cardiol 105:563–570. https://doi.org/10.1007/s00392-016-0970-4
Fox H, Bitter T, Horstkotte D, Oldenburg O (2017) Sleep-disordered breathing and arrhythmia in heart failure patients. Sleep Med Clin 12:229–241. https://doi.org/10.1016/j.jsmc.2017.01.003
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol 52:686–717. https://doi.org/10.1016/j.jacc.2008.05.002
Gami AS, Howard DE, Olson EJ, Somers VK (2005) Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 352:1206–1214. https://doi.org/10.1056/NEJMoa041832
Rowley JA, Badr MS (2017) Central sleep apnea in patients with congestive heart failure. Sleep Med Clin 12:221–227. https://doi.org/10.1016/j.jsmc.2017.03.001
Pedersen CT, Kay GN, Kalman J, Borggrefe M, Della-Bella P, Dickfeld T, Dorian P, Huikuri H, Kim YH, Knight B, Marchlinski F, Ross D, Sacher F, Sapp J, Shivkumar K, Soejima K, Tada H, Alexander ME, Triedman JK, Yamada T, Kirchhof P, Lip GY, Kuck KH, Mont L, Haines D, Indik J, Dimarco J, Exner D, Iesaka Y, Savelieva I (2014) EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Heart Rhythm 11:e166-196. https://doi.org/10.1016/j.hrthm.2014.07.024
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep M (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619. https://doi.org/10.5664/jcsm.2172
Fox H, Bitter T, Horstkotte D, Oldenburg O (2017) Resolution of cheyne-stokes respiration after treatment of heart failure with Sacubitril/Valsartan: a first case report. Cardiology 137:96–99. https://doi.org/10.1159/000455118
Omran H, Bitter T, Fox H, Horstkotte D, Oldenburg O (2015) [Association of sleep-disordered breathing and malignant arrhythmias in patients with ischemic and dilated cardiomyopathy]. Herzschrittmacherther Elektrophysiol 26:27–31. https://doi.org/10.1007/s00399-015-0354-x
Lanfranchi PA, Somers VK, Braghiroli A, Corra U, Eleuteri E, Giannuzzi P (2003) Central sleep apnea in left ventricular dysfunction: prevalence and implications for arrhythmic risk. Circulation 107:727–732
Linz D, Denner A, Illing S, Hohl M, Ukena C, Mahfoud F, Ewen S, Reil JC, Wirth K, Bohm M (2016) Impact of obstructive and central apneas on ventricular repolarisation: lessons learned from studies in man and pigs. Clin Res Cardiol 105:639–647. https://doi.org/10.1007/s00392-016-0961-5
Koehler U, Apelt S, Cassel W, Hildebrandt O, Nell C, Ranft S, Grimm W (2012) Sleep disordered breathing and nonsustained ventricular tachycardia in patients with chronic heart failure. Wien Klin Wochenschr 124:63–68. https://doi.org/10.1007/s00508-011-0083-z
Tomaello L, Zanolla L, Vassanelli C, LoCascio V, Ferrari M (2010) Sleep disordered breathing is associated with appropriate implantable cardioverter defibrillator therapy in congestive heart failure patients. Clin Cardiol 33:E27–E30. https://doi.org/10.1002/clc.20602
Bitter T, Westerheide N, Prinz C, Hossain MS, Vogt J, Langer C, Horstkotte D, Oldenburg O (2011) Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J 32:61–74. https://doi.org/10.1093/eurheartj/ehq327
Bitter T, Fox H, Dimitriadis Z, Niedermeyer J, Prib N, Prinz C, Horstkotte D, Oldenburg O (2014) Circadian variation of defibrillator shocks in patients with chronic heart failure: the impact of Cheyne-Stokes respiration and obstructive sleep apnea. Int J Cardiol 176:1033–1035. https://doi.org/10.1016/j.ijcard.2014.07.294
Naughton MT (2012) Cheyne-Stokes respiration: friend or foe? Thorax 67:357–360. https://doi.org/10.1136/thoraxjnl-2011-200927
Oldenburg O, Spiesshofer J, Fox H, Bitter T, Horstkotte D (2015) Cheyne-Stokes respiration in heart failure: friend or foe? Hemodynamic effects of hyperventilation in heart failure patients and healthy volunteers. Clin Res Cardiol 104:328–333. https://doi.org/10.1007/s00392-014-0784-1
Yasuma F (2013) Is Cheyne-Stokes respiration friend or foe of heart failure? Thorax 68:106–107. https://doi.org/10.1136/thoraxjnl-2012-202725
Ryan CM, Juvet S, Leung R, Bradley TD (2008) Timing of nocturnal ventricular ectopy in heart failure patients with sleep apnea. Chest 133:934–940. https://doi.org/10.1378/chest.07-2595
Grimm W, Kesper K, Cassel W, Timmesfeld N, Hildebrandt O, Koehler U (2017) Cheyne-stokes respiration during wakefulness in patients with chronic heart failure. Sleep Breath 21:419–426. https://doi.org/10.1007/s11325-016-1433-x
La Rovere MT, Pinna GD, Maestri R, Robbi E, Mortara A, Fanfulla F, Febo O, Sleight P (2007) Clinical relevance of short-term day-time breathing disorders in chronic heart failure patients. Eur J Heart Fail 9:949–954. https://doi.org/10.1016/j.ejheart.2007.06.009
Javaheri S, Corbett WS (1998) Association of low PaCO2 with central sleep apnea and ventricular arrhythmias in ambulatory patients with stable heart failure. Ann Intern Med 128:204–207
Oldenburg O, Coats A (2017) CSA is not beneficial long term in heart failure patients with reduced ejection fraction. Int J Cardiol 227:474–477. https://doi.org/10.1016/j.ijcard.2016.11.003
Linz D, Woehrle H, Bitter T, Fox H, Cowie MR, Bohm M, Oldenburg O (2015) The importance of sleep-disordered breathing in cardiovascular disease. Clin Res Cardiol 104:705–718. https://doi.org/10.1007/s00392-015-0859-7
Oldenburg O, Arzt M, Bitter T, Bonnemeier H, Edelmann F, Fietze I, Podszus T, Schäfer T, Schöbel C, Skobel E, Skowasch D, Penzel T, Nienaber C (2015) Positionspapier “Schlafmedizin in der Kardiologie”. Der Kardiol 9:140–158. https://doi.org/10.1007/s12181-015-0654-8
Fox H, Bitter T, Horstkotte D, Oldenburg O, Gutleben KJ (2017) Long-term experience with first-generation implantable neurostimulation device in central sleep apnea treatment. Pacing Clin Electrophysiol 40:498–503. https://doi.org/10.1111/pace.13049
Oldenburg O, Fox H, Bitter T, Horstkotte D (2017) Adaptive servoventilation to treat sleep-disordered breathing in cardiac patients. Somnologie 21:82–83. https://doi.org/10.1007/s11818-017-0100-1
Lyons OD, Floras JS, Logan AG, Beanlands R, Cantolla JD, Fitzpatrick M, Fleetham J, John Kimoff R, Leung RS, Lorenzi Filho G, Mayer P, Mielniczuk L, Morrison DL, Ryan CM, Series F, Tomlinson GA, Woo A, Arzt M, Parthasarathy S, Redolfi S, Kasai T, Parati G, Delgado DH, Bradley TD, Investigators A-H (2017) Design of the effect of adaptive servo-ventilation on survival and cardiovascular hospital admissions in patients with heart failure and sleep apnoea: the ADVENT-HF trial. Eur J Heart Fail 19:579–587. https://doi.org/10.1002/ejhf.790
Acknowledgements
English language editing assistance was provided by Nicola Ryan, independent medical writer. No outside finding was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Omran, H., Bitter, T., Horstkotte, D. et al. Characteristics and circadian distribution of cardiac arrhythmias in patients with heart failure and sleep-disordered breathing. Clin Res Cardiol 107, 965–974 (2018). https://doi.org/10.1007/s00392-018-1269-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1269-4