Abstract
Objective
Timing of the operation for exchange of right ventricular (RV) to pulmonary artery (PA) conduits is a matter of considerable debate. We aimed to study the course of right ventricular dimension in patients undergoing conduit exchange.
Patients and methods
We retrospectively studied all patients who underwent implantation and or replacement of RV/PA conduits during the time period between 1990 and 2005. Clinical and echocardiographic data were recorded as obtained at follow-up visits.
Results
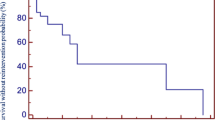
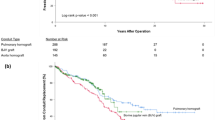
A total of 229 (144 boys and 85 girls) underwent surgery for implantation and or replacement of RV/PA conduits during the study period. Patients were assigned to three age groups including 37 infants, 125 children aged 1−10 years and 67 patients more than 10 years of age. 185 pulmonary (81%) and 44 aortic homografts (19%) were implanted. Fifty-eight of these 185 patients (25%) required exchange of conduits after a median time of 6.4 (8 months–12 years) (median (range)). The follow-up was 7.55 (0.1–17) years. The survival of the patients after homograft change was 98%. Freedom from failure for aortic and pulmonary homografts at an interval of 10 years for all patients was 38.5% for aortic and 56.2% for pulmonary homografts (P = 0.018; Mann–Whitney). Age at conduit exchange (coefficient: −4.917; P < 0.001) and right ventricular end-diastolic dimension (RVDD) before conduit exchange (coefficient: 8.255; P < 0.001) were related to RVDD as measured by M-mode echocardiography at follow-up (“best subset” regression analysis; R squared = 0.746). RVDD decreased in 48/58 patients, remained unchanged in 8/58 and increased in 2/59 patients at follow-up. An increased RVDD was positively correlated to the duration of artificial ventilation after the operation for conduit exchange (R = 0.56; P < 0.001).
Conclusions
Reoperation for exchange of degenerated conduits should be performed early to prevent the development of irreversible structural myocardial changes and persistence of right ventricular dilatation.






Similar content being viewed by others
References
Baskett RJ, Ross DB, Nanton MA, Murphy DA (1996) Factors in the early failure of cryopreserved homograft pulmonary valves in children: preserved immunogenicity? J Thorac Cardiovasc Surg 112:1170–1178
Brown JW, Ruzmetov M, Rodefeld MD, Vijay P, Turrentine MW (2005) Right ventricular outflow tract reconstruction with an allograft conduit in non-ross patients: risk factors for allograft dysfunction and failure. Ann Thorac Surg 80:655–663; discussion 663–664
Clarke DR, Bishop DA (1995) Ten year experience with pulmonary allografts in children. J Heart Valve Dis 4:384–391
Chaturvedi RR, Redington AN (2007) Pulmonary regurgitation in congenital heart disease. Heart 93:880–889
Dave HH, Buechel ER, Khatami AD, Kadner A, Rousson V, Bauersfeld U, Pretre R (2005) Early insertion of a pulmonary valve for chronic regurgitation helps restoration of ventricular dimensions. Ann Thorac Surg 80:1615–1621
Dearani JA, Danielson GK, Puga FJ, Schaff HV, Warnes CW, Driscoll DJ, Schleck CD, Ilstrup DM (2003) Late follow-up of 1095 patients undergoing operation for complex congenital heart disease utilizing pulmonary ventricle to pulmonary artery conduits. Ann Thorac Surg 75:399–411
Discigil B, Dearani JA, Puga FJ, Schaff HV, Hagler DJ, Warnes CA, Danielson GK (2001) Late pulmonary valve replacement after repair of tetralogy of Fallot. J Thorac Cardiovasc Surg 121:344–351
Forbess JM (2004) Conduit selection for right ventricular outflow tract reconstruction: contemporary options and outcomes. Semin Thorac Cardiovasc Surg Pediatr. Card Surg Annu 7:115–124
Gerestein CG, Takkenberg JJ, Oei FB, Cromme-Dijkhuis AH, Spitaels SE, van Herwerden LA, Steyerberg EW, Bogers AJ (2001) Right ventricular outflow tract reconstruction with an allograft conduit. Ann Thorac Surg 71:911–917
Grothoff M, Spors B, Abdul-Khaliq H, Abd El Rahman M, Alexi-Meskishvili V, Lange P, Felix R, Gutberlet M (2006) Pulmonary regurgitation is a powerful factor influencing QRS duration in patients after surgical repair for tetralogy of Fallot. Clin Res Cardiol 95:643–649
Hawkins JA, Bailey WW, Dillon T, Schwartz DC (1992) Midterm results with cryopreserved allograft valved conduits from the right ventricle to pulmonary artery. J Thorac Cardiovasc Surg 104:910–916
Jashari R, Van Hoeck B, Gaudino M, Daenen W, Van Geldorp T, Kalmar P, Goffin Y (2000) Are pulmonary homografts which were subjected to pulmonary hypertension more appropriate for aortic valve replacement than normal pulmonary homografts? A long-term multicentric echography study. Eur J Cardiothorac Surg 17:140–145
Kampmann C, Wiethoff CM, Wenzel A, Stolz G, Betancor M, Wippermann CF, Huth RG, Habermehl P, Knuf M, Emschermann T, Stopfkuchen H (2000) Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart 83:667–672
Meliones JN, Kern FH, Schulmann SR, Ungerleider RM, Greeley WJ (1996) Pathophysiological directed approach to congenital heart disease: a perioperative perspective. In: Greeley WJ (ed) Perioperative management of the patient with congenital heart disease. Williams & Wilkins, Baltimore, pp 1–42
Norozi K, Wessel A, Buchhorn R, Alpers V, Arnhold JO, Zooge M, Gayer S (2007) Is the ability index superior to the NYHA classification for assessing heart failure? Comparison of two classification scales in adolescents and adults with operated congenital heart defects. Clin Res Cardiol 96:542–547
Ross DN, Somerville J (1996) Correction of pulmonary atresia with a homograft aortic valve. Lancet 2(7479):1446–1447
Schamberger MS, Hurwitz RA (2000) Course of right and left ventricular function in patients with pulmonary insufficiency after repair of tetralogy of Fallot. Pediatr Cardiol 21:244–248
Stark J (1998) The use of valved conduits in pediatric cardiac surgery. Pediatr Cardiol 19:282–288
Therrien J, Siu SC, McLaughlin PR, Liu PP, Williams WG, Webb GD (2000) Pulmonary valve replacement in adults late after repair of tetralogy of Fallot: are we operating too late? J Am Coll Cardiol 36:1670–1675
Tiete AR, Sachweh JS, Groetzner J, Gulbins H, Muehl EG, Messmer BJ, Daebritz SH (2006) Systemic mechanical heart valve replacement in children under 16 years of age. Clin Res Cardiol 95:281–288
Warner KG, O’Brien PKH, Rhodes J, Kaur A, Robinson DA, Payne DD (2003) Expanding the indications for pulmonary valve replacement after repair of tetralogy of Fallot. Ann Thorac Surg 76:1066–1072
Wells WJ, Arroyo H Jr, Bremner RM, Wood J, Starnes VA (2002) Homograft conduit failure in infants is not due to somatic outgrowth. J Thorac Cardiovasc Surg 124:88–96
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loukanov, T., Sebening, C., Springer, W. et al. Replacement of valved right ventricular to pulmonary artery conduits: an observational study with focus on right ventricular geometry. Clin Res Cardiol 97, 169–175 (2008). https://doi.org/10.1007/s00392-007-0599-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-007-0599-4