Abstract
Background
There is a lack of data describing caregiver burden in primary care where most (informal) caregiving is provided.
Objective
The aims of the paper are to describe the burden of people caring for persons with dementia (PWD) in primary care in multiple dimensions and to analyze factors associated with specific dimensions of caregiver burden.
Material and methods
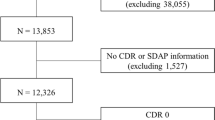
Analyses are based on cross-sectional data of the general physician-based, cluster-randomized, controlled intervention trial DelpHi-MV (Dementia: life and person-centered help). A sample of n = 310 community dwelling PWD screened positive for dementia (DemTect < 9) and their caregivers provided sociodemographic and disease-related data, caregiver burden was assessed in 20 dimensions using the Berlin inventory on relatives’ burden in dementia (Berliner Inventar zur Angehörigenbelastung – Demenz, BIZA-D).
Results
Depending on the dimension of objective burden due to caring, between 71.3 % and 92.3 % of the caregivers reported an objective burden. The average burden ranged from 3.68 to 9.81 (scale range 0–16). The subjective burden due to caring ranged from 0.1 to 1.1 (scale range 0–4). Between 22.6 and 51.6 % of our sample indicated burdens due to perceived conflicts. Logistic regression models associating caregiver burden with specifics of PWD and caregivers reached statistical significance for nearly all dimensions of the BIZA-D. Functional and cognitive impairment were statistically significant factors in 12 out of 20 and 5 out of 20 dimensions, respectively.
Conclusion
This is first quantitative in-depth analysis of burden for caregiver of people screened positive for dementia in primary care in Germany. In general, caregiver burden was perceived as being low to moderate by caregivers and lower than reported from other settings.
Zusammenfassung
Hintergrund
Ein Großteil der an Demenz erkrankten Menschen lebt in der eigenen Häuslichkeit. In der ambulanten Versorgung der Betroffenen spielen die Angehörigen eine wichtige Rolle. Über die Belastung der Angehörigen in diesem Setting ist jedoch nur wenig bekannt.
Ziel
Ziele dieses Beitrags sind die mehrdimensionale Beschreibung der Belastung von Angehörigen von Menschen mit Demenz (MmD) in der Häuslichkeit und die Analyse mit der Angehörigenbelastung assoziierter Faktoren der MmD.
Methode
Diese Analyse basiert auf querschnittlichen Daten der hausarztbasierten, cluster-randomisierten kontrollierten Interventionsstudie DelpHi-MV (Demenz: lebenswelt- und personenzentrierte Hilfen in Mecklenburg-Vorpommern). Eine Stichprobe von n = 310 in der Häuslichkeit lebender, positiv auf Demenz gescreenter Menschen (DemTects < 9) und deren Angehörigen wurden bezüglich Soziodemographie, krankheitsbezogener Daten und der Angehörigenbelastung untersucht. Die Angehörigenbelastung wurde in 20 Dimensionen durch das „Berliner Inventar zur Angehörigenbelastung – Demenz“ (BIZA-D) gemessen.
Ergebnisse
In Abhängigkeit von der untersuchten Dimension gaben zwischen 71,3 und 92,3 % der Angehörigen eine objektive Belastung an. Diese wurde im Durchschnitt, je nach Dimension, mit 3,68–9,81 auf einer Skala von 0–16 bewertet. Die subjektive Belastung variierte von 0,1 bis 1,1 auf einer Skala von 0–4. Zwischen 22,6 und 51,6 % unserer Stichprobe gaben eine Belastung aufgrund subjektiv wahrgenommener Bedürfniskonflikte an. Logistische Regressionsmodelle zur Analyse von mit Angehörigenbelastung assoziierten Faktoren der MmD waren statistisch signifikant für nahezu alle Dimensionen des BIZA-D. Funktionale Einschränkungen (ADL) und kognitive Einschränkungen waren dabei signifikant mit Belastung assoziierte Faktoren in 13 von 20 bzw. 5/20 Dimensionen.
Schlussfolgerung
Dies ist die erste quantitative tiefergehende Analyse der Angehörigenbelastung in der Häuslichkeit lebender Menschen mit Demenz in Deutschland. Im Vergleich mit anderen Studien und Settings wurde die Angehörigenbelastung geringer und als eher leicht bis mittel eingeschätzt.
Similar content being viewed by others
References
Bastawrous M (2013) Caregiver burden – a critical discussion. Int J Nurs Stud 50:431–441
Bedard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M (2001) The Zarit Burden Interview: a new short version and screening version. Gerontologist 41:652–657
Bickel H (2004) Epidemiologie und Gesundheitsökonomie. In: Wallesch C‑W, Förstl H (eds) Demenzen. Thieme Referenzreihe Neurologie. Thieme, Stuttgart
Braun M, Scholz U, Hornung R, Martin M (2010) Caregiver burden with dementia patients. A validation study of the German language version of the Zarit Burden Interview. Z Gerontol Geriatr 43:111–119
Calabrese P, Kessler J (2000) Screening for cognitive impairment in dementia – the DemTect procedure. Eur Neuropsychopharmacol 10:369
Cummings JL (1997) The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology 48:S10–S16
Eichler T, Thyrian JR, Dreier A, Wucherer D, Kohler L, Fiss T et al (2014) Dementia care management: going new ways in ambulant dementia care within a GP-based randomized controlled intervention trial. Int Psychogeriatr 26:247–256
Erzigkeit H, Lehfeld H, Pena-Casanova J, Bieber F, Yekrangi-Hartmann C, Rupp M et al (2001) The Bayer-Activities of Daily Living Scale (B-ADL): results from a validation study in three European countries. Dement Geriatr Cogn Disord 12:348–358
Gauggel S, Birkner B (1999) Validity and reliability of a German version of the Geriatric Depression Scale (GDS). Z Klin Psychol Psychother 28:18–27
Hindmarch I, Lehfeld H, de Jongh P, Erzigkeit H (1998) The Bayer Activities of Daily Living Scale (B-ADL). Dement Geriatr Cogn Disord 9(Suppl 2):20–26
Kessler J, Markowitsch HJ, Denzler P (1990) Mini-Mental-Status-Test (MMST) [German Version]. Beltz Test GmbH, Göttingen
Meuser TM, Marwit SJ (2001) A comprehensive, stage-sensitive model of grief in dementia caregiving. Gerontologist 41:658–670
Pearlin LI, Mullan JT, Semple SJ, Skaff MM (1990) Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 30:583–594
Sanders S, Ott CH, Kelber ST, Noonan P (2008) The experience of high levels of grief in caregivers of persons with Alzheimer’s disease and related dementia. Death Stud 32:495–523
Sansoni J, Anderson KH, Varona LM, Varela G (2013) Caregivers of Alzheimer’s patients and factors influencing institutionalization of loved ones: some considerations on existing literature. Ann Ig 25:235–246
Sansoni J, Riccio P, Vellone E, Piras G (1999) Family dynamics: sleep quality of women caregivers of family members with Alzheimer disease. Prof Inferm 52:73–79
Sansoni J, Vellone E, Piras G (2004) Anxiety and depression in community-dwelling, Italian Alzheimer’s disease caregivers. Int J Nurs Pract 10:93–100
Schneekloth U, Wahl H‑W (2006) Möglichkeiten und Grenzen selbständiger Lebensführung in Privathaushalten im Lichte der Ergebnisse von MuG III. In: Schneekloth U, Wahl H‑W (eds) Selbstständigkeit und Hilfebedarf bei älteren Menschen in Privathaushalten – Pflegearrangements, Demenz, Versorgungsangebote, 1st edn. Kohlhammer, Stuttgart, pp 229–242
Seeher K, Low LF, Reppermund S, Brodaty H (2013) Predictors and outcomes for caregivers of people with mild cognitive impairment: a systematic literature review. Alzheimers Dement 9:346–355
Thyrian JR, Eichler T, Hertel J, Wucherer D, Dreier A, Michalowsky B et al (2015) Burden of behavioral and psychiatric symptoms in people screened positive for dementia in primary care: results of the DelpHi-Study. J Alzheimers Dis 46(2):451–459
Thyrian JR, Fiss T, Dreier A, Bowing G, Angelow A, Lueke S et al (2012) Life- and person-centred help in Mecklenburg-Western Pomerania, Germany (DelpHi): study protocol for a randomised controlled trial. Trials 13:56
Thyrian JR, Hoffmann W (2012) Dementia care and general physicians – a survey on prevalence, means, attitudes and recommendations. Cent Eur J Public Health 20:270–275
Torti FM Jr., Gwyther LP, Reed SD, Friedman JY, Schulman KA (2004) A multinational review of recent trends and reports in dementia caregiver burden. Alzheimer Dis Assoc Disord 18:99–109
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Zank S, Schacke C, Leipold B (2006) Berliner Inventar zur Angehörigenbelastung – Demenz (BIZA-D). Z Klin Psychol Psychother 35:296–305
Thyrian JR, Eichler T, Michalowsky B, Wucherer D, Reimann M, Hertel J, Richter S, Dreier A, Hoffmann W (2016) Community-dwelling people screened positive for dementia in primary care: A comprehensive, multivariate descriptive analysis using data from the DelpHi-study. J Alzheimers Dis 52(2):609–617
Acknowledgements
The assessment of data was conducted as part of the DelpHi-Trial. We thank the experienced field study team and research group (in alphabetical order): Kerstin Albuerne, Aniela Angelow, Grit Assmann, Vaska Böhmann, Georgia Böwing, Kathleen Dittmer, Thomas Fiss, Sarah Gardzella, Jana Hubert, Ulrike Kempe, Viktoriya Kim, Saskia Moll, Andrea Pooch, Steffen Richter, Christiane Schnick and Christine Winckler.
Funding
There was no funding received for the analyses reported in this manuscript. The DelpHi-MV study was funded by the German Center for Neurodegenerative Diseases (DZNE) and the University Medicine of Greifswald (no grant number, clinical Trials gov. Identifier: NCT01401582).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. R. Thyrian, P. Winter, T. Eichler, M. Reimann, D. Wucherer, A. Dreier, B. Michalowsky, K. Zarm and W. Hoffmann state that they have no conflict of interests.
The accompanying manuscript does not include studies on animals. Informed consent was obtained from all participants in the study. In the case of participants being unable to give informed consent, this was obtained from the legal representative.
Additional information
J. R. Thyrian designed the study, formulated the research questions, supervised the analysis and drafted the paper; P. Winter assisted with formulating the research questions, analyzing the data and writing the article; T. Eichler supported the data assessment and contributed to the writing of the manuscript; M. Reimann conducted the statistical analysis and assisted in writing the article; D. Wucherer supported the data assessment and the writing of the article; A. Dreier assisted in designing the study and writing the manuscript; B. Michalowsky helped conduct the study and assisted with writing the manuscript; K. Zarm gave critical thematic input and supported the writing of the article; W. Hoffmann supervised the design of the study, the data assessment and the analysis and supported the writing of the article.
Electronic Supplementary Material
391_2016_1119_MOESM1_ESM.docx
Table 4 Summary of logistic regression models for each of the different dimensions of caregiver burden based on specifics of persons with dementia cared for (random effects for GP included)
Rights and permissions
About this article
Cite this article
Thyrian, J.R., Winter, P., Eichler, T. et al. Relatives’ burden of caring for people screened positive for dementia in primary care. Z Gerontol Geriat 50, 4–13 (2017). https://doi.org/10.1007/s00391-016-1119-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-016-1119-9