Abstract
Acute renal failure (ARF) is a frequent complication in patients with multiple organ failure and sepsis leading to a significant increase of mortality in these critically ill patients (50– 70%). While for years, ARF was considered an unavoidable complication of multiple organ failure and thus not essential for the progress, various studies in recent years have shown an independent and fundamental influence of ARF and therefore its therapy on the survival of the patient.
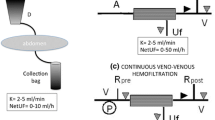
In the late 1970s continuous forms of treatment were introduced into the intensive care units. The first form of this treatment option was continuous arteriovenous hemofiltration (CAVH), primarily developed for the treatment of overhydrated patients resistant to diuretics. Using pump driven forms of the treatment, such as venovenous hemofiltration or venovenous dialysis (CVVHD), nearly all patients can be treated sufficiently. CAVH in the early 1980s rarely exceeded a daily hemofiltrate of 8–15 L, while more recent randomized studies have shown that CVVH should be performed with an exchange amount of at least 35 ml/kg/h, which corresponds to a daily exchange of 60–80 L.
With the abandonment of arterial puncture and the use of specialized equipment including CVVH machines, allowing a distinct balance in these critically ill, the most important disadvantages of the formerly used CAVH are eliminated but have also led to a loss of simplicity of the method.
Scientific work in the next decade should focus on (local) anticoagulation and determination of the optimal amounts of hemofiltrate for different diseases.
Zusammenfassung
Das akute Nierenversagen (ANV) in der Intensivmedizin ist heute immer Teil eines Multiorganversagens (MOV). Seine Prognose ist mit einer Letalität von 50–70% weiterhin schlecht. Während jahrelang das ANV als möglicherweise unvermeidbare Komplikation des MOV hingenommen und für die Prognose als nicht wegweisend eingeschätzt wurde, zeigen verschiedene Untersuchungen der letzten Jahre einen unabhängigen, fundamentalen Einfluss des ANV und damit vor allem seiner Therapie auf das Überleben der Patienten. Dabei gehören die Ende der 1970iger Jahre in die Behandlung eingeführten kontinuierlichen Therapieoptionen heute neben der intermittierenden Dialyse auf den Intensivstationen zur Standardtherapie.
Das erste kontinuierliche Nierenersatzverfahren, die kontinuierliche arterio-venöse Hämofiltration (CAVH), war ursprünglich für die Behandlung therapierefraktärer Entwässerung bei Patienten mit renaler und kardialer Insuffizienz entwickelt worden und war für die Behandlung von MOV-Patienten unzureichend. Mit den pumpenunterstützten Behandlungsverfahren wie der kontinuierlichen veno-venösen Hämofiltration (CVVH) oder Dialyse (CVVHD) sind Therapieoptionen geschaffen worden, die jeden Patienten ausreichend effektiv behandeln können. Betrug die ursprüngliche tägliche Austauschmenge 8–15 L, haben randomisierte Untersuchungen gezeigt, dass die Patienten mit MOV und ANV bei Einsatz der CVVH von einem Austauschvolumen von mindestens 35 ml/kgKG/h profitieren, was einem täglichen Filtratumsatz von 60–80 L entspricht.
Mit dem Verzicht auf eine arterielle Punktion und der Nutzung hochtechnisierter Maschinen, die parallel zur Behandlung die Bilanzierung der Behandlung ermöglichen, sind die wesentlichen Nachteile der ursprünglichen CAVH mittlerweile beseitigt, wenn auch die kontinuierliche Therapie hierdurch ihre Einfachheit verloren hat.
Gegenstand der Forschung der nächsten Jahre werden die Untersuchungen zur (lokalen) Antikoagulation und zur differenzierten Betrachtung unterschiedlicher Austauschvolumina für verschiedene Patientengruppen sein.
Similar content being viewed by others
Literatur
Bellomo R, Tipping P, Boyce N (1993) Continuous veno-venous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med 21:522–526
Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R (2008) Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med 36:610–617
Bouman CS, Oudemans-Van Straaten HM, Tijssen JG, Zandstra DF, Kesecioglu J (2002) Effects of early highvolume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med 30:2205–2211
Clark WR, Müller BA, Kraus MA, Macias WL (1997) Extracorporeal therapy requirements for patients with acute renal failure. J Am Soc Nephrol 8:804–812
Cole L, Bellomo R, Hart G, Journois D, Davenport P, Tipping P, Ronco C (2002) A phase II randomized controlled trial of continuous hemofiltration in sepsis. Crit Care Med 18:235–240
Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P (2001) High-volume hemofiltration in human septic shock. Intensive Care Med 27:978–986
Elahi MM, Yann Lim M, Joseph RN, Dhannapuneni RR, Spyt TJ (2004) Early hemofiltration improves survival in post-cardiotomy patients with acute renal failure. Eur J Cardiothorac Surg 26:1027–1031
Frank RD, Kierdorf HP (2003) Spezielle Antikoagulationsverfahren für die Nierenersatztherapie in der Intensivmedizin. Intensivmed 40:382–391
Getting LG, Reynolds HN, Scalea T (1999) Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early versus late. Intensive Care Med 25:805–813
Guerin C, Girard R, Selli JM, Ayzac L (2002) Intermittent versus continuous renal replacement therapy for acute renal failure in intensive care units: results from a multicenter prospective epidemiological survey. Intensive Care Med 28:1411–1418
Heering P, Ivens K, Thümer O, Morgera S, Heintzen M, Passlick-Deetjen J, Willers R, Strauer BE, Grabensee B (1999) The use of different buffers during continuous hemofiltration in critically ill patients with acute renal failure. Intensive Care Med 25:1244–1251
Heering P, Morgera S, Schmitz FJ, Schmitz G, Willers R, Schultheiss HP, Strauer BE, Grabensee B (1997) Cytokine removal and cardiovascular hemodynamics in septic patients with continuous hemofiltration. Intensive Care Med 23:288–296
Honore PM, Jamez J, Wauthier M, Lee PA, Dugernier T, Pirenne B, Hanique G, Matson JR (2000) Prospective evaluation of short-term, highvolume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med 28:3581–3587
Kellum JA, Angus DC, Johnson JP, Leblanc M, Griffin M, Ramakrishnan N, Linde-Zwirble WT (2002) Continuous versus intermittent renal replacement therapy: a meta-analysis. Intensive Care Med 28:29–37
Kierdorf HP (1991) Continuous versus intermittent treatment: Clinical results in acute renal failure. Contrib Nephrol 93:1–12
Kierdorf HP (2006) Nierenersatztherapie in der Intensivmedizin: Klassische Verfahren. Nephrologe 2:88–96
Kierdorf HP (2006) Organversagen Niere: Diagnostik und Therapie. Dtsch Med Wochenschr 131:2475–2479
Kierdorf HP (2006) Sepsis und akutes Nierenversagen. Intensivmed 43:175–188
Kierdorf HP, Leue C, Arns C (1999) Lactate- or bicarbonate-buffered solutions in continuous extracorporeal renal replacement therapies. Kidney Int 72:S32–S36
Kolff WJ (1947) New ways of treating uremia. Churchill Livingstone, London New York
Kramer P, Wigger W, Rieger J, Matthaei D, Scheler F (1977) Arteriovenous haemofiltration: A new and simple method for treatment of overhydrated patients resistant to diuretics. Klin Wochenschr 55:1121–1122
Lameire N, Van Biesen W, Vanholder R (2005) Acute renal failure. Lancet 365:417–430
Mehta RL (1996) Modalities of dialysis in acute renal failure. Seminars in Dialysis 9:469–475
de Mendonca A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F (2000) Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med 26:915–921
Metnitz PGH, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, Le Gall J-R, Druml W (2002) Effect of Acute Renal Failure Requiring Renal Replacement Therapy on Outcome in Critically Ill Patients. Crit Care Med 30:2051–2058
Morgera S, Rocktaschel J, Haase M, Lehmann C, von Heymann C, Ziemer S, Priem F, Hocher B, Gohl H, Kox WJ, Buder HW, Neumayer HH (2003) Intermittent high permeability hemofiltration in septic patients with acute renal failure. Intensive Care Med 29:1889–1895
Paganini EP, Tapolyai M, Goormastic M, Halstenberg W, Kozlowski L, Leblanc M (1996) Establishing a dialysis therapy/Patients outcome link in ICU acute dialysis for patients with ARF. Am J Kid Dis 28:81–89
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G (2000) Effects of different doses in continuous venovenous hemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 355:26–30
Ronco C, Brendolan A, Dentini V, Ricci Z, Wratten ML, Bellomo R (2003) Coupled plasma filtration adsorption: rationale, technical development and early clinical experience. Blod Purif 21:409–416
Saudan P, Niederberger M, De Seigneux S, Romand J, Pugin J, Perneger T, Martin PY (2006) Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int 70:1312–1317
Schiffl H, Lang SM, König A, Strasser T, Haider MC, Held E (1994) Biocompatible membranes in acute renal failure: prospective case controlled study. Lancet 344:570–572
Schrier WR, Wang W (2004) Acute renal failure and sepsis. N Engl J Med 351:159–169
Schultheis R, BringsW, GloecknerWM, Sieberth HG (1985) Device for controlled cyclic substitution during spontaneus filtration. In: Continuous arteriovenous haemofiltration (CAVH). Int Conf on CAVH, Aachen 1984, pp 64– 66. Karger, Basel
Sieberth HG, Freiberg J, Heinze J, Kostock G, Quiring FR, Schäfer E (1975) Der Einfluß nichtrenaler Organfunktionsstörungen auf die Überlebenschancen beim akuten Nierenversagen. Intensivmed 12:195–199
Sieberth HG, Kierdorf HP (1999) Is cytokine removal by continuous hemofiltration feasable? Kidney Int 56:S79–S83
Sigler MH (1997) Transport characteristics of the slow therapies: Implications for achieving adequacy of dialysis in acute renal failure. Adv Ren Replace Ther 4:68–73
Storck M, Hartl WH, Zimmerer E, Inthorn D (1991) Comparison of pump-driven and spontaneous continuous haemofiltration in postoperative acute renal failure. Lancet 337:452–455
Tonelli M, Manns B, Feller-Kopman D (2002) Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis 40:875–885
Vinsonneau C, Camus C, Combes A, Costa de Beauregard MA, Klouche K, Boulain T, Pallot JL, Chiche JD, Taupin P, Landais P, Dhainaut JF, Hemodiafe Study Group (2006) Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple- organ dysfunction syndrome: a multicentre randomised trial. Lancet 368:379–385
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kierdorf, H.P. Kontinuierliche Nierenersatztherapie in der Behandlung des akuten Nierenversagens: Geschichte und Entwicklung. Intensivmed 45, 194–204 (2008). https://doi.org/10.1007/s00390-008-0881-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00390-008-0881-3