Abstract
Despite numerous therapeutic advances in critical care medicine, the treatment of patients with severe sepsis and septic shock remains a major medical challenge. In the pathogenetic course of systemic inflammation (SIRS), excessive release of endogenous and exogenous pro-inflammatory mediators such as lipopolysaccharides (LPS), tumor necrosis factor (TNF)-α, interleukin (IL)-1 and IL-6 occurs and multiple organ failure (MOF) develops. This leads to devastating clinical outcomes. In a complex dynamic control system, pro-inflammatory stimuli yield upregulation of anti-inflammatory mediators (IL-10, transforming growth factor-beta [TGF-β]) which induce a counter-regulatory anti-inflammatory response. This eventually yields monocytic deactivation leading to failure of the cell-mediated immune system (immunoparalysis).
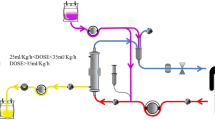
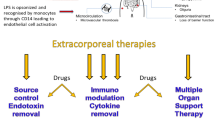
To reduce levels of circulating inflammatory and anti-inflammatory mediators, various approaches have been investigated, including selective and unselective intermittent and continuous extracorporeal treatment devices. Today, new blood purification technologies such as selective plasmapheresis and adsorption techniques provide new therapeutic avenues to target key mediators in septic patients. In this review, current and future adjunctive extracorporeal treatment strategies are discussed in the context of recent clinical trials.
Zusammenfassung
Trotz zahlreicher Fortschritte in der Intensivmedizin stellt die Behandlung von Patienten mit schwerer Sepsis und septischem Schock eine medizinische Herausforderung dar. In der Pathogenese der systemischen Inflammation (SIRS) kommt es zur exzessiven Freisetzung von multiplen endogenen und exogenen inflammatorischen Mediatoren [z. B. Lipopolysaccharid (LPS), Tumor-Nekrose-Faktor (TNF)-α, Interleukin (IL)-1, IL-6] und zur Entwicklung eines Multi- Organ-Versagen (MOV). Dies führt bekanntermaßen zu schlechten Überlebenszahlen septischer Patienten. Ein komplexes dynamisches Kontrollsystem führt in der Abfolge meist zur zeitnahen gegen-regulatorischen antiinflammatorischen Antwort mittels Induktion anti-inflammatorischer Mediatoren (IL-10, transforming growth factor-beta [TGF-β]). In einer großen Anzahl septischer Patienten kommt es durch eine Persistenz des inflammatorischen Reizes zu einer Deaktivierung von antigenpräsentierenden Zellen bzw. zu einem Versagen des zellvermittelten Immunsystems („Immunparalyse“).
Unselektive und selektive intermittierende und kontinuierliche extrakorporale Therapieverfahren wurden evaluiert, ob diese in der Lage sind, in inflammatorische durch den klinischen Verlauf günstig zu beeinflussen. Technologische Fortschritte im Hinblick auf die Entwicklung von extrakorporalen Plasmapherese- bzw. Adsorptionsverfahren bieten heute neue, effektive Möglichkeiten, Mediatoren aus der Blutbahn septischer Patienten zu entfernen. In der vorliegenden Übersichtsarbeit werden aktuell verfügbare und zukünftige adjunktive extrakorporale Therapiestrategien vorgestellt und vor dem Hintergrund aktueller Studien diskutiert.
Similar content being viewed by others
Literatur
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Annane D, Bellissant E, Cavaillon JM (2005) Septic shock. Lancet 365:63–78
Dellinger RP, Carlet JM, Gerlach H et al (2004) The surviving sepsis guidelines: not another “groundhog day”. Crit Care Med 32:1601–1602
Levy MM, Pronovost PJ, Dellinger RP et al (2004) Sepsis change bundles: converting guidelines into meaningful change in behavior and clinical outcome. Crit Care Med 32:S595–S597
Dellinger RP, Carlet JM, Masur H et al (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Levy MM, Fink MP, Marshall JC et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31:1250–1256
Cohen J (2002) The immunopathogenesis of sepsis. Nature 420:885–891
Volk HD, Reinke P, Docke WD (2000) Clinical aspects: from systemic inflammation to ‘immunoparalysis’. Chem Immunol 74:162–177
Docke WD, Randow F, Syrbe U et al (1997) Monocyte deactivation in septic patients: restoration by IFN-gamma treatment. Nat Med 3:678–681
Docke WD, Hoflich C, Davis KA et al (2005) Monitoring temporary immunodepression by flow cytometric measurement of monocytic HLA-DR expression: a multicenter study. Clin Chem
Hoflich C, Volk HD (2002) Immunomodulation in sepsis. Chirurg 73:1100–1104
Dremsizov TT, Kellum JA, Angus DC (2004) Incidence and definition of sepsis and associated organ dysfunction. Int J Artif Organs 27:352–359
Kellum JA, Angus DC (2002) Patients are dying of acute renal failure. Crit Care Med 30:2156–2157
Druml W (2004) Acute renal failure is not a “cute” renal failure! Intensive Care Med 30:1886–1890
Gormley SM, McBride WT, Armstrong MA et al (2002) Plasma and urinary cytokine homeostasis and renal function during cardiac surgery without cardiopulmonary bypass. Cytokine 17:61–65
Gotloib L, Barzilay E, Shustak A et al (1986) Hemofiltration in septic ARDS. The artificial kidney as an artificial endocrine lung. Resuscitation 13:123–132
Stein B, Pfenninger E, Grunert A et al (1990) Influence of continuous haemofiltration on haemodynamics and central blood volume in experimental endotoxic shock. Intensive Care Med 16:494–499
Grootendorst AF, van Bommel EF, van der HB et al (1992) High volume hemofiltration improves right ventricular function in endotoxin-induced shock in the pig. Intensive Care Med 18:235–240
Bellomo R, Honore PM, Matson J et al (2005) Extracorporeal blood treatment (EBT) methods in SIRS/Sepsis. Int J Artif Organs 28:450–458
Carcillo JA, Kellum JA (2002) Is there a role for plasmapheresis/plasma exchange therapy in septic shock, MODS, and thrombocytopenia-associated multiple organ failure? We still do not know – but perhaps we are closer. Intensive Care Med 28:1373–1375
Kellum JA, Bellomo R, Mehta R et al (2003) Blood purification in non-renal critical illness. Blood Purif 21:6–13
McMaster P, Shann F (2003) The use of extracorporeal techniques to remove humoral factors in sepsis. Pediatr Crit Care Med 4:2–7
Ronco C, Inguaggiato P, D’Intini V et al (2003) The role of extracorporeal therapies in sepsis. J Nephrol 16 (Suppl 7):S34–S41
Ronco C, Bonello M, Bordoni V et al (2004) Extracorporeal therapies in non-renal disease: treatment of sepsis and the peak concentration hypothesis. Blood Purif 22:164–174
Tetta C, D'Intini V, Bellomo R et al (2003) Extracorporeal treatments in sepsis: are there new perspectives? Clin Nephrol 60:299–304
Venkataraman R, Subramanian S, Kellum JA (2003) Clinical review: extracorporeal blood purification in severe sepsis. Crit Care 7:139–145
Kellum JA, Mehta RL, Angus DC et al (2002) The first international consensus conference on continuous renal replacement therapy. Kidney Int 62:1855–1863
Kellum JA, Angus DC, Johnson JP et al (2002) Continuous versus intermittent renal replacement therapy: a meta-analysis. Intensive Care Med 28:29–37
Ronco C, Bellomo R, Kellum JA (2002) Continuous renal replacement therapy: opinions and evidence. Adv Ren Replace Ther 9:229–244
Davenport A, Will EJ, Davidson AM (1993) Improved cardiovascular stability during continuous modes of renal replacement therapy in critically ill patients with acute hepatic and renal failure. Crit Care Med 21:328–338
De Vriese AS, Vanholder RC, Pascual M et al (1999) Can inflammatory cytokines be removed efficiently by continuous renal replacement therapies? Intensive Care Med 25:903–910
De Vriese AS, Colardyn FA, Philippe JJ et al (1999) Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol 10:846–853
Bellomo R, Boyce N (1993) Continuous venovenous hemodiafiltration compared with conventional dialysis in critically ill patients with acute renal failure. ASAIO J 39:M794–M797
Bellomo R, Tipping P, Boyce N (1993) Continuous veno-venous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med 21:522–526
Heering P, Morgera S, Schmitz FJ et al (1997) Cytokine removal and cardiovascular hemodynamics in septic patients with continuous venovenous hemofiltration. Intensive Care Med 23:288–296
Kellum JA, Johnson JP, Kramer D et al (1998) Diffusive vs convective therapy: effects on mediators of inflammation in patient with severe systemic inflammatory response syndrome. Crit Care Med 26:1995–2000
Cole L, Bellomo R, Hart G et al (2002) A phase II randomized, controlled trial of continuous hemofiltration in sepsis. Crit Care Med 30:100–106
Schetz M (1994) Removal of cytokines in septic patients using continuous veno-venous hemodiafiltration. Crit Care Med 22:715–716
Kellum JA, Mehta RL, Angus DC et al (2002) The first international consensus conference on continuous renal replacement therapy. Kidney Int 62:1855–1863
Honore PM, Joannes-Boyau O (2004) High volume hemofiltration (HVHF) in sepsis: a comprehensive review of rationale, clinical applicability, potential indications and recommendations for future research. Int J Artif Organs 27:1077–1082
Ronco C, Bellomo R, Homel P et al (2000) Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 356:26–30
Kellum JA, Dishart MK (2002) Effect of hemofiltration filter adsorption on circulating IL-6 levels in septic rats. Crit Care 6:429–433
Cole L, Bellomo R, Journois D et al (2001) High-volume haemofiltration in human septic shock. Intensive Care Med 27:978–986
Honore PM, Jamez J, Wauthier M et al (2000) Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med 28:3581–3587
Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI et al (1999) Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 25:814–821
Ratanarat R, Brendolan A, Piccinni P et al (2005) Pulse high-volume haemofiltration for treatment of severe sepsis: effects on hemodynamics and survival. Crit Care 9:R294–R302
Brendolan A, D'Intini V, Ricci Z et al (2004) Pulse high volume hemofiltration. Int J Artif Organs 27:398–403
Reiter K, Bellomo R, Ronco C et al (2002) Pro/con clinical debate: is high-volume hemofiltration beneficial in the treatment of septic shock? Crit Care 6:18–21
Lonnemann G, Bechstein M, Linnenweber S et al (1999) Tumor necrosis factor-alpha during continuous highflux hemodialysis in sepsis with acute renal failure. Kidney Int (Suppl):S84–S87
Ronco C, Bellomo R, Hensel M (1997) Continuous “high flux” dialysis: an effective renal replacement therapy for intensive care patients. Zentralbl Chir 122:378–382
Tetta C, Cavaillon JM, Schulze M et al (1998) Removal of cytokines and activated complement components in an experimental model of continuous plasma filtration coupled with sorbent adsorption. Nephrol Dial Transplant 13:1458–1464
Tetta C, Gianotti L, Cavaillon JM et al (2000) Coupled plasma filtration-adsorption in a rabbit model of endotoxic shock. Crit Care Med 28:1526–1533
Bosch T (2003) Recent advances in therapeutic apheresis. J Artif Organs 6:1–8
Palmer JD, Rifkind D (1974) Neutralization of the hemodynamic effects of endotoxin by polymyxin B. Surg Gynecol Obstet 138:755–759
Yonekawa M (2005) Cytokine and endotoxin removal in critically Ill patients. Ther Apher Dial 9:A37
Uriu K, Osajima A, Hiroshige K et al (2002) Endotoxin removal by direct hemoperfusion with an adsorbent column using polymyxin B-immobilized fiber ameliorates systemic circulatory disturbance in patients with septic shock. Am J Kidney Dis 39:937–947
Vincent JL, Laterre PF, Cohen J et al (2005) A pilot-controlled study of a polymyxin B-immobilized hemoperfusion cartridge in patients with severe sepsis secondary to intra-abdominal infection. Shock 23:400–405
Reinhart K, Meier-Hellmann A, Beale R et al (2004) Open randomized phase II trial of an extracorporeal endotoxin adsorber in suspected Gramnegative sepsis. Crit Care Med 32:1662–1668
Bengsch S, Boos KS, Nagel D et al (2005) Extracorporeal plasma treatment for the removal of endotoxin in patients with sepsis: clinical results of a pilot study. Shock 23:494–500
Amoureux MC, Rajapakse N, Hegyi E et al (2004) Endotoxin removal from whole blood by a novel adsorption resin: efficiency and hemocompatibility. Int J Artif Organs 27:480–487
Staubach KH, Boehme M, Zimmermann M et al (2003) A new endotoxin adsorption device in Gram-negative sepsis: use of immobilized albumin with the MATISSE adsorber. Transfus Apher Sci 29:93–98
Schefold JC, von Haehling S, Corsepius M et al (2007) A novel selective extracorporeal intervention in sepsis: immunoadsorption of endotoxin, interleukin-6, and complement-activating product 5a. Shock, in press
Leese T, Holliday M, Heath D et al (1987) Multicentre clinical trial of low volume fresh frozen plasma therapy in acute pancreatitis. Br J Surg 74:907–911
Busund R, Koukline V, Utrobin U et al (2002) Plasmapheresis in severe sepsis and septic shock: a prospective, randomised, controlled trial. Intensive Care Med 28:1434–1439
Schmidt J, Mann S, Mohr VD et al (2000) Plasmapheresis combined with continuous venovenous hemofiltration in surgical patients with sepsis. Intensive Care Med 26:532–537
Kellum JA, Song M, Venkataraman R (2004) Hemoadsorption removes tumor necrosis factor, interleukin-6, and interleukin-10, reduces nuclear factor-kappaB DNA binding, and improves short-term survival in lethal endotoxemia. Crit Care Med 32:801–805
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schefold, J.C., Hasper, D., Storm, C. et al. Die extrakorporale Therapie septischer Patienten. Intensivmed 44, 57–63 (2007). https://doi.org/10.1007/s00390-007-0758-x
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00390-007-0758-x