Abstract
Sepsis and septic shock are the leading causes of acute renal failure, multiple organ system dysfunction, and death in the intensive care unit. The pathogenesis of sepsis is complex and comprises a mosaic of interconnected pathways. Several attempts to improve patient outcomes by targeting specific components of this network have been unsuccessful. For these reasons, the ideal immunomodulating strategy would be one that restores immunologic stability rather than blindly inhibiting or stimulating one or another component of this complex network. Hence, the recent focus of immunomodulatory therapy in sepsis has shifted to nonspecific methods of influencing the entire inflammatory response without suppressing it. Here, we discuss the various modalities of extracorporeal blood purification, the existing evidence, and future prospects.
Similar content being viewed by others
Introduction
Extracorporeal therapies designed to remove substances from the circulation now include hemodialysis, hemofiltration, hemoadsorption, plasma filtration, cell-based therapies, and combinations of any of these. In recent years there have been considerable advances in our understanding and technical capabilities, but consensus over the optimal way and under what conditions to use these therapies does not exist. In general, these therapies have been adapted to sepsis from nephrology-based therapy (hemodialysis for renal failure) or from hematology-based therapy (plasma exchange for thrombotic thrombocytopenic purpura).
Continuous renal replacement therapies
More than a decade ago, Gotloib and coworkers [1] observed that renal replacement therapy could remove inflammatory mediators from the plasma of septic patients. Subsequently, Stein and coworkers [2] described an improvement in hemodynamics associated with hemofiltration in the pig following administration of intravenous endotoxin. A short time later these findings were confirmed by Grootendorst and coworkers [3], who also found that the ultrafiltrate removed from endotoxemic animals produced hemodynamic instability in healthy animals when it was infused intravenously [4]. At about this time, Lee and coworkers [5] reported a survival benefit associated with hemofiltration in septic pigs and Bellomo and coworkers [6] showed that some of the ILs and tumor necrosis factor (TNF) could be removed from the circulation of humans with sepsis. With these advances, blood purification as a treatment for human septic shock was born.
Since that time many technological advances have occurred, along with substantial changes in our basic understanding of sepsis and the inflammatory response. Modifications of existing technology and new approaches have created a vast array of possible therapies to use or investigate.
'Conventional' continuous renal replacement therapy
The various modalities of continuous renal replacement therapy (CRRT) differ in the kind of access (arteriovenous versus veno-venous), mechanism of solute transport (convective versus diffusive), and location where the replacement fluid enters the extracorporeal circuit (predilution versus post-dilution). In arteriovenous circuits blood is driven by the patient's blood pressure through a filter, via an extracorporeal circuit originating from an artery and terminating in a vein. However, in a veno-venous circuit, blood is driven by a peristaltic pump module (with appropriate air bubble and pressure monitors) through a filter via an extracorporeal circuit originating and terminating in a vein. Arteriovenous circuits carry all of the risks associated with arterial puncture (i.e. thrombosis, bleeding, etc.) and are disadvantageous in that the ultrafiltration and solute clearance are dependent on the patient's blood pressure and their efficiency is unpredictable [7]. For these reasons, veno-venous circuits using double-lumen catheters are considered safer, more efficient, and are now widely preferred in the management of renal failure. Given that the system requirements are only greater with immunomodulation, arteriovenous systems have been abandoned in the treatment of sepsis.
The term 'diffusion' describes a type of solute transport across a semipermeable membrane generated by a concentration gradient. The extent of diffusive clearance is determined by the molecular weight of the solute (or more precisely by the Einstein–Stokes radius of the molecule), the concentration gradient across the membrane, temperature, and the membrane surface area, thickness and pore size. Smaller solutes such as urea, creatinine, and electrolytes are cleared efficiently by diffusion, and as a solute's molecular weight increases diffusivity decreases. During CRRT the addition of countercurrent dialysate flow accomplishes diffusive clearance by maximizing the concentration gradient between blood and dialysate through the length of the membrane. The term 'convection' describes a process in which solutes are transported across a semipermeable membrane, along with movement of solvent (ultrafiltration) that occurs in response to a positive transmembrane pressure gradient. Here, the clearance depends on the ultrafiltration rate and sieving characteristics of the membrane and solute, and to a lesser extent on the molecular size of the solute. Dialysis membranes are further classified based on their ultrafiltration coefficients into high-flux and low-flux membranes (i.e. for a given transmembrane pressure gradient, high-flux membranes have a higher filtration rate than do low-flux membranes).
There are few data to state convincingly that convective clearance is better than diffusive clearance. However, studies comparing convective clearance and diffusive clearance have shown that middle-molecular-weight substances (peptides) and large molecules such as vancomycin are better removed by convection [8–10]. Some of the molecules implicated in sepsis and multiple organ dysfunction fall into the middle-molecular-weight range, and hence convective therapy may serve as a useful adjunctive therapy in septic shock [9]. In addition, convective treatments permit isotonic ultrafiltration, whereas in diffusive treatments osmotic changes in plasma may produce unwanted fluid shifts toward the intracellular compartment.
The nomenclature of the CRRT modality depends on the type of access (arteriovenous versus veno-venous) and the mechanism of solute clearance used. If the clearance is purely diffusive then the term 'hemodialysis' is used, and if the clearance is purely convective then the term 'hemofiltration' is used. When both convective and diffusive clearances are used, the term 'hemodiafiltration' is applied. Continuous hemodiafiltration – a combination of convective and diffusive clearance – is the most efficient CRRT modality. In modalities that involve convective clearance, the ultrafiltrate produced during membrane transit is replaced completely or in part with a replacement solution to achieve volume control and blood purification. Ultrafiltration in excess of replacement results in patient weight loss [11]. The replacement fluid can be infused either before the filter (predilution) or after the filter (postdilution). The efficiency of postdilution CRRT is limited by the maximum acceptable value of filtration fraction and by the maximal blood flow that can be delivered by the access. Conversely, predilution CRRT is not limited by filtration fraction and therefore allows for higher ultrafiltration rates. This, along with increased replacement fluid rate and a more porous membrane, can enhance solute clearance. However, at a given ultrafiltration rate, predilution results in reduced solute clearance as compared with postdilution because of dilution of solutes at blood entry into the filter. Hence, ultrafiltration must be relatively increased to maintain the same efficiency of solute removal as is observed in postdilution mode [12–14]. Although definitive evidence is lacking, predilution fluid replacement also is believed to enhance filter patency during CRRT and to reduce need for anticoagulation [15].
Along with a surge in proinflammatory mediators, there is a parallel rise in anti-inflammatory substances in sepsis, which creates a state of 'immunoparalysis' that is characterized by immune effector cell (i.e. monocyte) dysfunction [16]. Both the proinflammatory and anti-inflammatory cascades interact with each other, and form a complex network that is constantly trying to balance and restore immunologic homeostasis [17]. Numerous therapies designed to intervene in the proinflammatory cascade alone have failed to alter the outcome of sepsis in recent years [18]. Hence, the recent focus of immunomodulatory therapy in sepsis has shifted to nonspecifically downregulating the entire inflammatory response without suppressing it, perhaps by using extracorporeal blood purification techniques. The rationale for such a strategy is that it would 'autoregulate' itself, such that as one component of the response increases, so too would the effect on that component [19].
Most of the immune mediators are water soluble and fall into the middle-molecular-weight category [20] and hence can theoretically be removed by a plasma water purification system such as hemofiltration. Based on the above rationale and observations, several investigators have studied the effects of CRRT in animal models of sepsis and have demonstrated some beneficial effects [21]. Subsequently, Kellum and coworkers [9] demonstrated that, although convective clearance (continuous veno-venous hemofiltration [CVVH]) was better than diffusion (continuous veno-venous hemodialysis) in reducing plasma TNF, the mode of clearance did not influence plasma concentrations of IL-6, IL-10, soluble L-selectin, or endotoxin. However, in a small clinical trial of early isovolemic CVVH at 2 l/hour, Cole and coworkers [22] were unable to demonstrate any reduction in the circulating concentrations of several cytokines and anaphylatoxins associated with septic shock, or could they show improved organ dysfunction following severe sepsis. Thus, the relative impact of conventional CRRT on inflammatory molecules is probably small and the impact on clinical outcomes uncertain. Hence, conventional CRRT is currently not recommended as a therapy for sepsis in patients without renal failure [14].
High-volume hemofiltration
Wide variation exists in the manner in which CRRT is prescribed worldwide. Although higher effluent flow rates are sometimes prescribed in Europe and Australia, because of the limitations of pump design, effluent flow rates during CRRT in the USA have traditionally been restricted to 2 l/hour or less. Recently, however, Ronco and coworkers [23] showed that higher CRRT doses (35 ml/kg per min) improved patient survival in acute renal failure (ARF) as compared with conventional doses (20 ml/kg per min), whereas further increases in dose to 45 ml/kg per min were not helpful. Because sepsis is a major cause or complicating factor associated with the development of ARF as well as mortality in this population, it is intriguing to speculate that increased inflammatory mediator removal with convection may have played a role in improving survival. Confirmation of this hypothesis awaits further large studies.
Although most of the inflammatory mediator molecules fall into the middle-molecular-weight category and can theoretically be removed by hemofiltration, they have very high generation rates relative to uremic toxins. Thus, the intensity of blood purification and the beneficial effects have been relatively modest with the traditionally used effluent flow rates of 1–2 l/hour (as used for management of ARF) [9, 22]. Subsequently, investigators seeking to achieve 'adequate blood purification' in sepsis hypothesized that higher ultrafiltration rates would be necessary. Defined by an ultrafiltration flow rate in excess of 35 ml/kg per hour and often as high as 75–120 ml/kg per hour [15], high-volume hemofiltration (HVHF) may be necessary to achieve 'clinically meaningful' convective removal of inflammatory mediators. To achieve high-volume hemofiltration (HVHF), it is necessary to use a high permeability membrane with a large surface area and sieving coefficient close to 1 for a wide spectrum of molecular weights.
Numerous in vitro and animal studies have shown that synthetic filters used in hemofiltration can extract a wide array of substances that are involved in sepsis to a certain degree [24]. Early studies conducted by Grootendorst and coworkers [3, 4] using porcine endotoxic models showed a major attenuation of endotoxin-induced hypotension and an improvement in cardiac performance with HVHF. Subsequent animal studies also showed similar beneficial effects with HVHF in endotoxic animal models [25, 26]. These animal findings subsequently triggered some interest in the potential benefits of HVHF in human sepsis. HVHF has been shown to improve hemodynamics, decrease vasopressor requirement and perhaps improve survival in septic patients [27–30]. However, those studies were all done in either small number of patients or were nonrandomized and uncontrolled. Despite these early promising studies, larger trials looking at HVHF as an adjunctive therapy in human sepsis are needed before such therapy can be routinely advocated.
Continuous high-flux dialysis
Extending previous work on nomenclature for CRRT, the Definitions Workgroup for the Acute Dialysis Quality Initiative defined continuous high-flux dialysis (CHFD) as a form of CRRT that uses a highly permeable dialyzer with blood and dialysate flowing countercurrent, and in which ultrafiltrate production is controlled by blood pumps whereby there is a balance of filtration and backfiltration, with ultrafiltrate produced in the proximal portion of the fibers and reinfused by backfiltration in the distal portion of the fibers so that replacement fluid is not required [15]. This technique has mainly been developed to optimize the clearance of middle molecules without compromising the clearance of urea nitrogen. Another feature seen in some systems is an addition of a gravimetric pump in the ultrafiltration/dialysate outflow limb. This regulates both the net ultrafiltration rate and the dialysate outflow rate. Once the patient's dry weight has been reached, the circuit may operate at zero net filtration using dialysate at varying flow rates to provide back filtration in the distal limb of the circuit equal in amount to the ultrafiltrate generated in the proximal limb. In this mode, convective transport is therefore maintained without any need for replacement fluids [31]. Since this technique combines convective and diffusive clearances, urea clearances of up to 60 l/day and middle molecule clearance (specifically inulin) of up to 36 l/day have been demonstrated.
There is very limited data on the use of CHFD as a mode of blood purification in human sepsis. Lonneman and coworkers [32] compared the effects of standard CVVH with CHFD on ex vivo induced whole blood production of TNF and inhibitory TNF soluble receptor type I in 12 patients with sepsis and ARF. That study showed an increase in TNF production with time during CHFD as compared with CVVH and a significant increase in soluble receptor concentration in the dialysate during CHFD.
Hemo-adsorption
Although uncontrolled clinical studies of HVHF suggest that hemodynamic variables and even survival might be improved [30], the optimal flow rate to achieve 'adequate' clearance of 3 inflammatory mediators has yet to be determined. Furthermore, the application of HVHF routinely in humans raises substantial organizational, technical, and financial issues. Removal rates and clearances of the different inflammatory cytokines (e.g. TNF, IL-1, etc.) are limited by poor membrane passage and may be further reduced over time as the membrane becomes 'fouled' by plasma proteins. However, there is also evidence that clearance of mediators by hemofiltration may be due more to adsorption of mediators to the membrane, although convective clearance is still partly responsible [33, 34].
Hence, in the quest to achieve higher mediator clearance, newer membranes/devices with higher porosity and adsorptive capacity have been tried. 'Hemoperfusion' is a technique in which a sorbent is placed in direct contact with blood in an extracorporeal circuit. Nonspecific adsorbents, typically charcoal and resins, attract solutes through a variety of forces, including hydrophobic interactions, ionic (or electrostatic) attraction, hydrogen bonding, and van der Waals interactions. By manipulating the porous structure of solid phase sorbents, it is possible to increase the selectivity of nonspecific adsorbents for particular solutes. In this case, solute molecules are separated according to their size and by their ability to penetrate the porous network of the sorbent material [35]. The adsorptive capacity for resins and charcoals is often quite high, in excess of 500 m2/g adsorbent. Until recently, poor biocompatibility, as evidenced by thrombocytopenia and neu-tropenia [36], was the major clinical limitation of these materials. Newer resin adsorbents appear to have resolved this issue with the addition of a biocompatible coating [37]. In view of the high-molecular-weight adsorption characteristics of sorbents, it is possible to target larger molecules that exceed the molecular weight cutoff of synthetic high-flux dialysis membranes. This makes sorbents potentially ideal for intervention in sepsis. Sorbents have been applied in different treatment modalities, including hemoperfusion and hemoperfusion coupled with hemodialysis or with plasma filtration. The choice of modality is based mainly on the properties of the sorbent and the technique used.
In Gram-negative sepsis, lipopolysaccharide and its fragments are instrumental in the initiation and perpetuation of the inflammatory response. Therefore, earlier extracorporeal devices were designed to remove the inciting stimulus (i.e. endotoxin). Attempts have been made to remove endotoxin from the circulation using polymyxin-B-immobilized fiber and charcoal hemoperfusion. Hemoperfusion with polymyxin-B-bound sepharose, immobilized with fiber, has been shown to have positive effects in an animal model of normotensive sepsis [38]. Subsequently, human studies have demonstrated that treatment with polymyxin-B-immobilized fiber reduces plasma levels of endotoxin, thrombomodulin, TNF release, and endothelin-1 levels in septic shock [39, 40]. In a pilot study (n = 16), Aoki and coworkers [41] showed that hemoperfusion with polymyxin-B-immobilized fiber significantly decreased endotoxin levels after 2 hours of direct hemoperfusion. Those investigators also showed that the hyperdynamic, high cardiac output state returned to normal levels after treatment, and in patients with arterial systolic pressure below 100 mmHg the pressure increased significantly from the pretreatment level. Fever was also alleviated by this therapy and did not return until the day after treatment. Nonetheless, no randomized controlled studies yet exist to support the effectiveness of this strategy in managing sepsis. Various other sorbents have been designed and used for blood purification, but are currently in the clinical testing phase. One such system is the molecular adsorbent regenerating system device, which employs a polysulfone high-permeability dialyzer with albumin on the dialysate side to aid transfer of protein-bound toxins across the membranes [42]. This system has mainly been used in the treatment of hepatic encephalopathy and fulminant hepatic failure, and good clinical studies in septic patients are lacking at the present time.
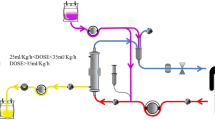
One of the techniques of hemo-adsorption is to separate the plasma from the blood using a plasma filter and then passing the filtered plasma through a synthetic resin cartridge, ultimately returning it to the blood. A second filter can be added to remove excess fluid and low-molecular-weight toxins. The use of a more open membrane (plasmafilter) coupled with adsorption may increase the adsorptive capacity of the system and achieve higher nonspecific clearance of inflammatory mediators [43]. Tetta and coworkers demonstrated both significant removal of both proinflammatory and anti-inflammatory mediators [44] and improved survival [45] using this technique in an animal model of sepsis. Subsequently, in a recent pilot study Ronco and coworkers [46] documented important physiologic benefits (hemodynamic stability and monocyte responsiveness) using this technique in septic patients. Using hemoperfusion with a different sorbent (CytoSorb™), in a lethal animal model of lipopolysaccharide-induced shock we recently demonstrated improved hemody-namics and survival time, along with significant decreases in plasma IL-6 and IL-10 levels, using hemoadsorption [47].
The above studies support a role for broad-spectrum hemo-adsorption of multiple inflammatory substances to augment the management of sepsis. These therapies offer new promise in the field of immunomodulation because they are both broad-spectrum (removing both proinflammatory and anti-inflammatory substances) and self-regulating (they remove substances in relation to their circulating concentrations) [48]. Broad-spectrum adsorption offers significant advantages over hemofiltration and is simpler to apply than plasmapheresis. Currently, extensive preclinical work is being undertaken to define the duration of therapy with sorbents, the timing of application, and device design [35].
Plasma therapies in critically ill patients
Although the terms 'plasmapheresis' and 'plasma exchange' are commonly used synonymously, the two techniques differ in important ways. Plasmapheresis is a two-step process in which first the separation of blood into its components (cells and plasma) is accomplished, by means of a centrifugal pump or filter. Then, the separated plasma is allowed to flow along column(s) containing different adsorbents, allowing the selective removal of components, and the processed plasma is reinfused back to the patient. Hence, in plasmapheresis no (or minimal) replacement fluids are necessary. By contrast, plasma exchange is a single-step process in which blood is separated into plasma and cells similarly using centrifugation pumps or a filter, and the cells are returned back to the patient while the plasma is replaced with either donor plasma or albumin [49]. Replacing volume lost with fresh frozen plasma is also done to replete any factor(s) (immunoglobu-lins, etc.) necessary to restore homeostasis and often to correct the underlying disorder for which the plasma therapy was done in the first place (e.g. thrombotic thrombocytopenic purpura). Plasma filtration has advantages over centrifugal plasma exchange in that it is less expensive and can be performed with the same machines as are used for CRRT.
Like other extracorporeal blood purification techniques, plasma therapies have been tried in the treatment of sepsis. Early animal studies done to evaluate efficacy in altering the inflammatory response have provided conflicting results [50–52]. In early human studies, plasma exchange has been shown to reduce effectively the plasma concentrations of various sepsis mediators [53–55]. However, wide variation exists in the pattern of mediator removal. For example, in a study conducted by Gardlund and coworkers [54], plasma exchange therapy in septic patients decreased the plasma levels of TNF but not of other cytokines. In contrast, Reeves and coworkers [56] showed that a wide variety of acute phase proteins and complement fragment C3 can effectively be removed by plasma exchange therapy in septic patients. However, in that study plasmafiltration did not influence mean concentrations of IL-6, granulocyte colony-stimulating factor, thromboxane B2, total white cell count, neutrophil count, or platelet count. There was also no improvement in survival with plasmafiltration in that study.
Independent of the specific mediators removed, plasma exchange therapy has been shown to be associated with improvement in hemodynamic variables in some clinical studies [57–59]. However, all of those studies were limited in that they studied small numbers of patients and were uncontrolled. In septic patients (n = 12), Berlot and coworkers [59] showed that the cardiac index improved significantly after plasma exchange therapy (aimed at removing the full volume of plasma). Interestingly, this improvement in cardiac index was not associated with any changes in preload or afterload. However, the improvement in hemodynamic variables was transient and had no effect on the outcome of these patients. Furthermore, patients in the study received plasma replacement, and hence it is difficult to infer whether these changes in hemodynamic variables were due to removal of mediators or due to the replacement substances present in the donor plasma. In patients with septic shock, Ronco and coworkers [46] showed that coupled plasmafiltration-adsorption combined with hemodialysis was associated with improvement in hemodynamics and leukocyte responsiveness as compared with treatment with continuous veno-venous hemodiafiltration. Finally, in a recent retrospective observational study (n = 7), Ataman and coworkers [60] failed to demonstrate any significant improvement in cardiovascular parameters (heart rate and mean arterial pressure) during the first 24 hours after plasmapheresis.
In a retrospective study looking at outcomes in patients with sepsis treated with plasma exchange therapy, Barzilay and coworkers [61] showed that patients treated with hemodiafiltration associated with plasma exchange had a better survival than did patients treated with conventional hemofiltration or hemodiafiltration without any plasma exchange therapy. Patients who did not receive any blood purification therapy (control group) had the worst outcome. However, that retrospective study has numerous study design limitations (i.e. it was nonrandomized, underpowered, and the different treatment groups were not comparable to each other). Subsequently, in another nonrandomized study, 19 septic patients who underwent CVVH combined with plasmapheresis were compared with 24 patients who had been treated for their sepsis without any blood purification technique [62]. Although in that study the treatment group had an overall lower mortality than did the control group (42.1% versus 45.8%), the primary organ failure rates were higher in the treatment group.
Some authors have argued that plasma therapies are most likely to be effective when they are applied after early stabilization of shock and perhaps when targeting thrombotic microangiopathy rather than cytokines [63]. Most recently, Busund and colleagues [64] used partial plasma exchange therapy and showed a tendency toward improve outcome in adult patients with septic shock. Finally, in a preliminary report, Nguyen and colleagues [65] reported that children with thrombocytopenia (platelet count <100 000/mm3)-associated multiple organ failure had reduced or absent von Willi-brand factor cleaving protease activity, along with markedly increased plasminogen activator inhibitor-1 activity, both of which were reversed by plasma exchange therapy. These patients required a median of 11 days of plasma exchange to reverse their multiple organ failure. These findings suggest that prolonged plasma exchange may be required to reverse the thrombotic microangiopathy of thrombocytopenia-associated sepsis as well. Hence, outcomes with plasma exchange therapy may also be related to duration of treatment and the presence of underlying thrombotic microangiopathy. Thus, based on the limited and conflicting data available, it is difficult to know whether plasma exchange will be useful in the management of sepsis, either alone or in combination with other forms of blood purification. These techniques are also more cumbersome and costly than other forms of extracorporeal blood purification (i.e. HVHF and hemo-adsorption). However, the results of recent studies, especially those in patients with sepsis-associated thrombotic microangiopathy, argue in favor of larger clinical trials.
Conclusion
Although this wider approach to blood purification in sepsis seems logical, promising and opens new perspectives, many questions still remain unanswered, including the timing, duration, and frequency of these therapies in the clinical setting. However, for now one can safely conclude that these techniques are usually well tolerated and are effective in clearing 'mediators' of sepsis from the plasma, often improving physiologic parameters. Large multicenter trials evaluating their efficacy to improve clinical outcomes (i.e. mortality or organ failure), rather than surrogate markers such as plasma mediator clearance or transient improvement in physiologic variables, are required to define the precise role of these therapies in the management of sepsis. Given the available data to date, we speculate that immunomodulation using either HVHF or hemo-adsorption, or both, will be most useful in the early stages of severe sepsis and septic shock when high levels of inflammatory mediators appear in the circulation, whereas plasma therapies will be most useful later in the course of illness when thrombotic microangiopathy and endothelial injury begin to immerge. The most effective blood purification strategy may be the careful deployment of both of these therapies at right time.
Abbreviations
- ARF:
-
= acute renal failure
- CHFD:
-
= continuous high-flux dialysis
- CRRT:
-
= continuous renal replacement therapy
- CVVH:
-
= continuous veno-venous hemofiltration
- HVHF:
-
= high-volume hemofiltration
- IL:
-
= interleukin
- TNFss:
-
= tumor necrosis factor.
References
Gotloib L, Barzilay E, Shustak A, Wais Z, Jaichenko J, Lev A: Hemofiltration in septic ARDS. The artificial kidney as an artificial endocrine lung. Resuscitation 1986, 13: 123-132.
Stein B, Pfenninger E, Grunert A, Schmitz JE, Hudde M: Influence of continuous haemofiltration on haemodynamics and central blood volume in experimental endotoxic shock. Intensive Care Med 1990, 16: 494-499.
Grootendorst AF, van Bommel EF, van der Hoven B, van Leengoed LA, van Osta AL: High volume hemofiltration improves right ventricular function in endotoxin-induced shock in the pig. Intensive Care Med 1992, 18: 235-240.
Grootendorst AF, van Bommel EF, van Leengoed LA, van Zanten AR, Huipen HJ, Groeneveld AB: Infusion of ultrafiltrate from endotoxemic pigs depresses myocardial performance in normal pigs. J Crit Care 1993, 8: 161-169.
Lee PA, Matson JR, Pryor RW, Hinshaw LB: Continuous arteriovenous hemofiltration therapy for Staphylococcus aureus -induced septicemia in immature swine. Crit Care Med 1993, 21: 914-924.
Bellomo R, Tipping P, Boyce N: Continuous veno-venous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med 1993, 21: 522-526.
Bellomo R, Parkin G, Love J, Boyce N: A prospective comparative study of continuous arteriovenous hemodiafiltration and continuous venovenous hemodiafiltration in critically ill patients. Am J Kidney Dis 1993, 21: 400-404.
Jeffrey RF, Khan AA, Prabhu P, Todd N, Goutcher E, Will EJ, Davison AM: A comparison of molecular clearance rates during continuous hemofiltration and hemodialysis with a novel volumetric continuous renal replacement system. Artif Organs 1994, 18: 425-428.
Kellum JA, Johnson JP, Kramer D, Palevsky P, Brady JJ, Pinsky MR: Diffusive vs. convective therapy: effects on mediators of inflammation in patient with severe systemic inflammatory response syndrome. Crit Care Med 1998, 26: 1995-2000. 10.1097/00003246-199812000-00027
Brunet S, Leblanc M, Geadah D, Parent D, Courteau S, Cardinal J: Diffusive and convective solute clearances during continuous renal replacement therapy at various dialysate and ultra-filtration flow rates. Am J Kidney Dis 1999, 34: 486-492.
Ronco R, Bellomo R: Nomenclature for continuous renal replacement therapies. In Critical Care Nephrology (Edited by: Ronco R, Bellomo R). Boston: Kluwer Academic Publishers 1998, 1169-1176.
Lebedo I: Predilution hemofiltration: a new technology applied to an old therapy! Int J Artif Organs 1995, 18: 735-742.
Ficheux A, Argiles A, Bosc JY, Mion C: Analysis of the influence of the infusion site on dialyser clearances measured in an in vitro system mimicking haemodialysis and haemodiafiltration. Blood Purif 1999, 17: 10-18. 10.1159/000014360
Kellum JA, Mehta RL, Angus DC, Palevsky P, Ronco C: The first international consensus conference on continuous renal replacement therapy. Kidney Int 2002, 62: 1855-1863. 10.1046/j.1523-1755.2002.00613.x
Acute Dialysis Quality Initiative.[http://www.adqi.net]
Adib-Conquy M, Adrie C, Moine P, Asehnoune K, Fitting C, Pinsky MR, Dhainaut JF, Cavaillon JM: NF-kappaB expression in mononuclear cells of patients with sepsis resembles that observed in lipopolysaccharide tolerance. Am J Respir Crit Care Med 2000, 162: 1877-1883.
Adrie C, Pinsky MR: The inflammatory balance in human sepsis. Intensive Care Med 2000, 26: 364-375. 10.1007/s001340051169
Abraham E, Matthay MA, Dinarello CA, Vincent JL, Cohen J, Opal SM, Glauser M, Parsons P, Fisher CJ Jr, Repine JE: Consensus conference definitions for sepsis, septic shock, acute lung injury, and acute respiratory distress syndrome: time for a reevaluation. Crit Care Med 2000, 28: 232-235. 10.1097/00003246-200001000-00039
Kellum JA, Venkataraman R: Blood purification in sepsis: an idea whose time has come? Crit Care Med 2002, 30: 1387-1388. 10.1097/00003246-200206000-00047
von Andrian UH, Mackay CR: T-cell function and migration. Two sides of the same coin. N Engl J Med 2000, 343: 1020-1034. 10.1056/NEJM200010053431407
Gomez A, Wang R, Unruh H, Light RB, Bose D, Chau T, Correa E, Mink S: hemofiltration reverses left ventricular dysfunction during sepsis in dogs. Anesthesiology 1990, 73: 671-685.
Cole L, Bellomo R, Hart G, Journois D, Davenport P, Tipping P, Ronco C: A phase II randomized, controlled trial of continuous hemofiltration in sepsis. Crit Care Med 2002, 30: 100-106.
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G: Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 2000, 356: 26-30. 10.1016/S0140-6736(00)02430-2
Silvester W: Mediator removal with CRRT: complement and cytokines. Am J Kidney Dis 1997,30(suppl 4):S38-S43.
Rogiers P, Zhang H, Smail N, Pauwels D, Vincent JL: Continuous venovenous hemofiltration improves cardiac performance by mechanisms other than tumor necrosis factor-alpha attenuation during endotoxic shock. Crit Care Med 1999, 27: 1848-1855. 10.1097/00003246-199909000-00024
Bellomo R, Kellum JA, Gandhi CR, Pinsky MR, Ondulik B: The effect of intensive plasma water exchange by hemofiltration on hemodynamics and soluble mediators in canine endotoxemia. Am J Respir Crit Care Med 2000, 161: 1429-1436.
Heering P, Morgera S, Schmitz FJ, Schmitz G, Willers R, Schultheiss HP, Strauer BE, Grabensee B: Cytokine removal and cardiovascular hemodynamics in septic patients with continuous venovenous hemofiltration. Intensive Care Med 1997, 23: 288-296. 10.1007/s001340050330
Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P: High-volume haemofiltration in human septic shock. Intensive Care Med 2001, 27: 978-986. 10.1007/s001340100963
Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI, Zandstra DF: Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 1999, 25: 814-821. 10.1007/s001340050957
Honore PM, Jamez J, Wauthier M, Lee PA, Dugernier T, Pirenne B, Hanique G, Matson JR: Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med 2000, 28: 3581-3587.
Ronco C, Bellomo R: Continuous high flux dialysis: an efficient renal replacement. In Yearbook of Intensive Care and Emergency Medicine (Edited by: Vincent JL). Heidelberg: Springer Verlag 1996, 690-696.
Lonnemann G, Bechstein M, Linnenweber S, Burg M, Koch KM: Tumor necrosis factor-alpha during continuous high-flux hemodialysis in sepsis with acute renal failure. Kidney Int Suppl 1999, 72: S84-S87.
De Vriese AS, Colardyn FA, Philippe JJ, Vanholder RC, De Sutter JH, Lameire NH: Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol 1999, 10: 846-853.
Kellum JA, Dishart MK: Effect of hemofiltration filter adsorption on circulating IL-6 levels in septic rats. Crit Care 2002, 6: 429-433. 10.1186/cc1528
Winchester JF, Kellum JA, Ronco C, Brady JA, Quartararo PJ, Salsberg JA, Levin NW: Sorbents in acute renal failure and the systemic inflammatory response syndrome. Blood Purif 2003, 21: 79-84. 10.1159/000067860
Pond SM: Extracorporeal techniques in the treatment of poisoned patients. Med J Aust 1991, 154: 617-622.
Ronco C, Brendolan A, Winchester JF, Golds E, Clemmer J, Polaschegg HD, Muller TE, Davankov V, Tsyurupa M, Pavlova L, Pavlov M, La Greca G, Levin NW: First clinical experience with an adjunctive hemoperfusion device designed specifically to remove beta 2-microglobulin in hemodialysis. Contrib Nephrol 2001, 133: 166-173.
Doig GS, Martin CM, Sibbald WJ: Polymyxin-dextran antiendo-toxin pretreatment in an ovine model of normotensive sepsis. Crit Care Med 1997, 25: 1956-1961. 10.1097/00003246-199712000-00009
Nakamura T, Suzuki Y, Shimada N, Ebihara I, Shoji H, Koide H: Hemoperfusion with polymyxin B-immobilized fiber attenuates the increased plasma levels of thrombomodulin and von Willebrand factor from patients with septic shock. Blood Purif 1998, 16: 179-186. 10.1159/000014333
Nakamura T, Ushiyama C, Suzuki S, Shoji H, Shimada N, Ebihara I, Koide H: Polymyxin b-immobilized fiber reduces increased plasma endothelin-1 concentrations in hemodialysis patients with sepsis. Ren Fail 2000, 22: 225-234. 10.1081/JDI-100100867
Aoki H, Kodama M, Tani T, Hanasawa K: Treatment of sepsis by extracorporeal elimination of endotoxin using polymyxin B-immobilized fiber. Am J Surg 1994, 167: 412-417.
Ash SR: Extracorporeal blood detoxification by sorbents in treatment of hepatic encephalopathy. Adv Ren Replace Ther 2002, 9: 3-18. 10.1053/jarr.2002.30474
Opal SM: Hemofiltration-absorption systems for the treatment of experimental sepsis: is it possible to remove the 'evil humors' responsible for septic shock? Crit Care Med 2000, 28: 1681-1682. 10.1097/00003246-200005000-00088
Tetta C, Cavaillon JM, Schulze M, Ronco C, Ghezzi PM, Camussi G, Serra AM, Curti F, Lonnemann G: Removal of cytokines and activated complement components in an experimental model of continuous plasma filtration coupled with sorbent adsorption. Nephrol Dial Transplant 1998, 13: 1458-1464. 10.1093/ndt/13.6.1458
Tetta C, Gianotti L, Cavaillon JM, Wratten ML, Fini M, Braga M, Bisagni P, Giavaresi G, Bolzani R, Giardino R: Coupled plasma filtration-adsorption in a rabbit model of endotoxic shock. Crit Care Med 2000, 28: 1526-1533. 10.1097/00003246-200005000-00045
Ronco C, Brendolan A, Lonnemann G, Bellomo R, Piccinni P, Digito A, Dan M, Irone M, La Greca G, Inguaggiato P, Maggiore U, De Nitti C, Wratten ML, Ricci Z, Tetta C: A pilot study of coupled plasma filtration with adsorption in septic shock. Crit Care Med 2002, 30: 1250-1255. 10.1097/00003246-200206000-00015
Kellum JA, Somg MC, Venkataraman R, et al.: Improved survival with hemoadsorption in endotoxin induced shock in rats [abstract]. Am J Respir Crit Care Med 2002, 165: A176.
Kellum JA: Immunomodulation in sepsis: the role of hemofiltration. Minerva Anestesiol 1999, 65: 410-418.
Berlot G, Lucangelo U, Galimberti G: Plasmapheresis in sepsis. Curr Opin Crit Care 2000, 6: 437-441. 10.1097/00075198-200012000-00012
Busund R, Lindsetmo RO, Rasmussen LT, Rokke O, Rekvig OP, Revhaug A: Tumor necrosis factor and interleukin 1 appearance in experimental gram-negative septic shock. The effects of plasma exchange with albumin and plasma infusion. Arch Surg 1991, 126: 591-597.
Busund R, Lindsetmo RO, Balteskard L, Rekvig OP, Revhaug A: Repeated plasma therapy induces fatal shock in experimental septicemia. Circ Shock 1993, 40: 268-275.
Natanson C, Hoffman WD, Koev LA, Dolan DP, Banks SM, Bacher J, Danner RL, Klein HG, Parrillo JE: Plasma exchange does not improve survival in a canine model of human septic shock. Transfusion 1993, 33: 243-248. 10.1046/j.1537-2995.1993.33393174451.x
Leese T, Holliday M, Heath D, Hall AW, Bell PR: Multicentre clinical trial of low volume fresh frozen plasma therapy in acute pancreatitis. Br J Surg 1987, 74: 907-911.
Gardlund B, Sjolin J, Nilsson A, Roll M, Wickerts CJ, Wretlind B: Plasma levels of cytokines in primary septic shock in humans: correlation with disease severity. J Infect Dis 1995, 172: 296-301.
Stegmayr B: Apheresis of plasma compounds as a therapeutic principle in severe sepsis and multiorgan dysfunction syndrome. Clin Chem Lab Med 1999, 37: 327-332.
Reeves JH, Butt WW, Shann F, Layton JE, Stewart A, Waring PM, Presneill JJ: Continuous plasmafiltration in sepsis syndrome. Plasmafiltration in Sepsis Study Group. Crit Care Med 1999, 27: 2096-2104. 10.1097/00003246-199910000-00003
Stegmayr BG: Plasmapheresis in severe sepsis or septic shock. Blood Purif 1996, 14: 94-101.
Mok Q, Butt W: The outcome of children admitted to intensive care with meningococcal septicaemia. Intensive Care Med 1996, 22: 259-263.
Berlot G, Gullo A, Fasiolo S, Serra L, Silvestri L, Worz M: Hemo-dynamic effects of plasma exchange in septic patients: preliminary report. Blood Purif 1997, 15: 45-53.
Ataman K, Jehmlich M, Kock S, Neumann S, Leischik M, Filipovic Z, Hopf HB: Short-term cardiovascular effects of plasma-pheresis in norepinephrine-refractory septic shock. Intensive Care Med 2002, 28: 1164-1167. 10.1007/s00134-002-1375-6
Barzilay E, Kessler D, Berlot G, Gullo A, Geber D, Ben Zeev I: Use of extracorporeal supportive techniques as additional treatment for septic-induced multiple organ failure patients. Crit Care Med 1989, 17: 634-637.
Schmidt J, Mann S, Mohr VD, Lampert R, Firla U, Zirngibl H: Plasmapheresis combined with continuous venovenous hemofiltration in surgical patients with sepsis. Intensive Care Med 2000, 26: 532-537. 10.1007/s001340051200
Carcillo JA, Kellum JA: Is there a role for plasmapheresis/plasma exchange therapy in septic shock, MODS, and thrombocytopenia-associated multiple organ failure? We still do not know – but perhaps we are closer. Intensive Care Med 2002, 28: 1373-1375. 10.1007/s00134-002-1428-x
Busund R, Koukline V, Utrobin U, Nedashkovsky E: Plasma-pheresis in severe sepsis and septic shock: a prospective, randomised, controlled trial. Intensive Care Med 2002, 28: 1434-1439. 10.1007/s00134-002-1410-7
Nguyen TC HM, Han YY, Seidberg N, Carcillo JA: Randomized controlled trial of plasma exchange therapy for thrombocytopenia associated multiple organ failure in children [abstract]. Pediatr Res 2001, 49: 42A.
Acknowledgements
As well as the affiliations listed at the top of the article, all authors are also from the "Clinical Research, Investigation, and Systems Modeling of Acute illness Laboratory" (CRISMA Laboratory), Pittsburgh, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
RV and JK have received research grants from Renaltech International and Gambro.
Rights and permissions
About this article
Cite this article
Venkataraman, R., Subramanian, S. & Kellum, J.A. Clinical review: Extracorporeal blood purification in severe sepsis. Crit Care 7, 139 (2003). https://doi.org/10.1186/cc1889
Published:
DOI: https://doi.org/10.1186/cc1889