Abstract
Purpose
Survival after local resection (LR) versus radical resection (RR) has been revealed comparable for patients with rectal and duodenal gastrointestinal stromal tumors (GISTs), but is unknown for jejunoileal (JI) GISTs. This study aimed to compare the long-term survival between patients with JI GISTs who underwent LR and RR, and to find out the prognostic factors for JI GISTs.
Methods
Patients diagnosed with JI GISTs in 1975–2019 were identified from Surveillance, Epidemiology, and End Results (SEER) database and grouped according to surgical modality. Propensity score matching (PSM) was performed to balance the LR and RR groups. Overall survival (OS) and disease-specific survival (DSS) were compared in the full and matched cohorts using Kaplan–Meier (KM) analysis. Subgroup sensitivity analyses were also performed. Risk factors associated with DSS were analyzed in multivariate Cox analysis following model selection.
Results
1107 patients diagnosed with JI GISTs were included in the study cohort. After PSM, OS and DSS were comparable in LR and RR groups. Consistently, the two groups had similar DSS in all subgroup analyses. Moreover, multivariate Cox analysis identified lymphadenectomy, older age, larger tumor size, distant metastasis, high and unknown mitotic rate, but not LR, as independent prognostic risk factors for JI GISTs.
Conclusions
We conducted the first population-based comparison between the effect of different surgical modes on survival for patients with JI GISTs. LR can be carried out safely without compromising oncological outcome, and should be considered as a treatment option in selected patients with JI GISTs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Though gastrointestinal stromal tumors (GISTs) are rare malignant tumors, they represent the most common sarcomas of the digestive system. GISTs could occur throughout the gastrointestinal tract and extragastrointestinally, but were found most frequently in stomach (50–60%), followed by jejunum and ileum (20–30%) [1, 2]. The most important prognostic factors for GISTs are tumor size, mitotic rate and tumor rupture [3, 4], but tumor site is also related with the risk of recurrence and prognosis since the nature of GISTs differ among locations [5]. Although jejunoileal (JI) GISTs are generally considered more aggressive than gastric GISTs, their characteristics remain controversial [6,7,8]. Indeed, only a few studies focused exclusively on JI GISTs with small sample sizes [8,9,10].
Surgery remains the only curative modality of therapy for GISTs if negative margins are ensured and tumor rupture are avoided [4]. Expanding resection margin and lymphadenectomy is unnecessary for GISTs since they rarely invade the adjacent organs or regional lymph nodes [11]. Moreover, studies have found that the positive microscopic margin (R1) may not influence survival for GISTs significantly, with or without adjuvant targeted therapy [12, 13]. Therefore, local resection (LR) such as wedge or segmental resection might be sufficient for GISTs whereas extended radical resection (RR) should be avoided [4, 14]. Comparable survival outcomes of LR versus RR have been found in duodenal and rectal GISTs [15,16,17], but it is questionable whether these findings could be expanded to other sites such as jejunum and ileum.
The aim of this study was to compare the survival outcome between patients with JI GISTs who underwent LR and RR. We also sought to identify the prognostic factors for JI GISTs.
Methods
Patient selection
Given the relatively low incidence of JI GISTs, we used Surveillance, Epidemiology, and End Results (SEER) database which collects data from population-based cancer registries that cover 34% of the U.S. population. This study used publicly available de-identified data involving no human participants, and thus was granted exemption by the institutional review board at Second Affiliated Hospital of Soochow University.
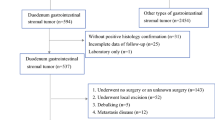
Patient selection is outlined in Fig. 1. Patients diagnosed with JI (International Classification of Diseases for Oncology, 3rd Edition [ICD-O-3] topography codes C17.1 and C17.2) GISTs (ICD-O-3 histology code 8936/3) from January 1 1975 through December 31 2019 were identified from the SEER database using SEER*Stat software version 8.4.0.1. Database names and detailed selection statements used for this study is provided in Supplementary Table 1. Patients were excluded for: (1) diagnosis not confirmed by histology, (2) non-primary tumor, (3) unknown survival months or loss to follow-up, (4) unknown cause of death, (5) unknown or unspecified tumor size, (6) surgery not performed or unknown, (7) unknown mode of surgery, or (8) local tumor destruction or debulking.
Study variables
Predictor variables (age, sex, race, marital status, year of diagnosis, income, area, tumor size, T stage, N stage, M stage, grade, mitotic rate, tumor site, chemotherapy, lymphadenectomy and mode of surgery), survival time and outcome variables (all-cause death [ACD] and disease-specific death [DSD]) used in this study were collected from SEER database and recoded.
T, N, and M stages were redefined according to the newest 8th edition of American Joint Committee on Cancer (AJCC) staging manual [3]. N0 was defined as no or unknown regional lymph node metastasis (LNM), and M0 was defined as no or unknown distant metastasis. Mitotic rate was recorded in SEER database since 2004, and was defined as low (≤ 5 mitoses per 5 mm2 or per 50 high-power field [HPF]) or high (> 5 mitoses per 5 mm2 or per 50 HPF) for patients with these data available, otherwise as unknown. Moreover, we grouped age (< 45, 45–79 and ≥ 80 years), tumor size (< 89 and ≥ 89 mm), T stage (T1-2, T3 and T4) and grade (I, II-IV and unknown) for survival analysis. Lymphadenectomy was defined by scope of regional lymph node surgery as no/unknown versus yes.
Mode of surgery is defined by site-specific surgery codes in SEER database. LR was defined as local tumor excision, or simple/partial removal of primary site (code 35–50 before 1998; code 20–30 since 1998). RR was defined as total removal of primary site, or partial/total removal of primary site with partial/total removal of other organs (code 60 before 1998; code 40 and 60 since 1998) [18]. Survival time was defined as months from diagnosis to ACD or last follow-up (December 31 2019). All patients in the study cohort completed full follow-up. DSD was identified by “Dead (attributable to this cancer dx)” in “SEER cause-specific death classification”.
Statistical analysis
Patients were divided into LR and RR groups based on their surgical modality. A 1:1 ratio propensity score matching (PSM) was performed based on age, sex, race, marital status, year of diagnosis, income, area, tumor size, T stage, N stage, M stage, grade, mitotic rate, tumor site, chemotherapy and lymphadenectomy to the two groups using “optimal” method in R package “MatchIt”. Before and after PSM, continuous variables were compared with unpaired Student’s t tests, while categorical variables were compared with Chi-square tests.
Survival analyses were performed using R package “survival”. Kaplan–Meier (KM) survival analysis with the log-rank test was used to assess the differences in overall survival (OS) and disease-specific survival (DSS) between the LR and RR groups. Survival probabilities at 5 year and 10 year were compared using “fixtdiff” function of R package “bpcp”. Hazard ratio (HR) for DSS with 95% confidence interval (CI) between the two groups was computed in the matched cohort and subgroups using the log-rank test.
Then, HR for DSS with 95% CI was estimated for each predictor variable using univariate Cox proportional hazards regression model (with Breslow’s ties). Furthermore, multivariate Cox models were fitted for mode of surgery, together with all possible combinations of variables with univariate p value < 0.1. To prevent overfitting, we performed automated model selection based on corrected Akaike Information Criterion (AICc) using “dredge” function in R package “MuMIn”. Models with ΔAICc (difference in AICc between a model and the model with the lowest AICc) < 2 were considered informationally equivalent. Predictor variables included in the simplest model (having the least number of variables) with the relatively smallest AICc were fitted into multivariate analysis, along with mode of surgery.
Statistical analysis was performed with R (version 4.2.1, R Core Team, Vienna, Austria). Best cutoff values for continuous variables were determined with X-tile (version 3.6.1, Yale University School of Medicine, New Haven, USA) (Supplementary Fig. 1). A two-sided p value < 0.05 was considered statistically significant. Values were presented as mean ± standard deviation for continuous variables and as number (%) for categorical variables.
Results
Patient characteristics and propensity score matching
Originally, 1318 patients with JI GISTs were extracted from SEER database, accounting for 35.6% of the total cases with small intestinal GISTs. Through patient selection, 1107 patients diagnosed from 1990 through 2019 were included in the final cohort (Fig. 1). The mean age at diagnosis for the full study cohort was 61.1 ± 14.3 years (Table 1). LR was conducted in 858 (77.5%) patients. The proportion of patients underwent LR increased from 70.8% (1990–2003) to 76.8% (2004–2011) and 80.5% (2012–2019).
Before PSM, LR and RR groups have significant differences in several variables (Table 1). The LR group had significantly smaller tumor and less T4 cases than the RR group. Patients in the LR group had less distant metastasis (M1) and ileal tumor, while they less frequently underwent chemotherapy and lymphadenectomy. In addition, marital status and year of diagnosis also differed significantly between groups. Therefore, we matched 249 patients in the LR group with 249 patients in the RR group based on propensity score.
After PSM, distributions of propensity score were similar between the two groups, and absolute standardized mean differences of all variables were < 0.1 (Supplementary Fig. 2). Comparison after PSM also showed the two groups not different significantly in all variables (p > 0.2), confirming a satisfactory balance (Table 1).
Survival analysis
Before PSM, LR group had similar OS (p = 0.16, Fig. 2a) but significantly better DSS (p = 0.0064, Fig. 2c) compared with the RR group. However, there were no significant differences between the LR and RR groups in long-term OS (5-year: 71.2% vs. 74.7%, p = 0.427; 10-year: 49.8% vs. 51.0%, p = 0.828) and DSS (5-year: 81.9% vs. 82.2%, p = 0.951; 10-year: 71.5% vs. 66.3%, p = 0.357) after PSM. KM analysis also showed that OS (HR 1.13, 95% CI 0.86–1.48, p = 0.382) and DSS (HR 0.92, 95% CI 0.64–1.34, p = 0.681) of the LR group was similar to that of the RR group (Fig. 2b, d).
Kaplan–Meier curves of overall-survival (OS) and disease-specific survival (DSS) for patients with jejunoileal gastrointestinal stromal tumors (JI GISTs) in the local resection and radical resection groups. a OS before propensity score matching (PSM); b OS after PSM; c DSS before PSM; d DSS after PSM
Subgroup sensitivity analyses
To further analyze the effects on DSS of LR and RR concomitant with other factors, subgroup log-rank tests were performed. The results showed that the LR group had similar DSS compared with the RR group across all subgroups (p > 0.05), which was consistent with the results of the overall matched population (Fig. 3).
Hazard ratios (HRs) for disease-specific survival (DSS) with 95% confidence intervals (CIs) of radical resection (RR) and local resection (LR) groups in all patients and the subgroups, assumed by log-rank test. An HR < 1 implies a better DSS of LR group than RR group whereas > 1 implies the opposite. UNK: unknown; Metro: metropolitan; Nonmetro: nonmetropolitan
Risk factors for disease-specific survival
Cox proportional hazards regression model was then used to identify the risk factors for DSS of JI GISTs. Univariate Cox analysis revealed that age, marital status, year of diagnosis, income, tumor size, T stage, N stage, M stage, grade, mitotic rate and chemotherapy were significantly associated with DSS for patients with JI GISTs (Table 2). In addition, lymphadenectomy also tended to increase the risk of DSS (p = 0.058).
All possible combinations of the variables above, together with mode of surgery, were then included in the multivariate analyses to study their interaction and relative contributions. Through model selection, a set of 17 models with ΔAICc < 2 was created. Three models had the least number of variables, among which Model 8 was considered the best with the relatively lowest AICc (AICc = 1149.8, ΔAICc = 1.06) which included age, lymphadenectomy, M stage, tumor size and mitotic rate (Supplementary Table 2). These five variables were further included in the multivariate Cox analysis together with mode of surgery, to prove their effects on DSS.
In multivariate Cox analysis, there was no significant difference between RR and LR on DSS (HR 0.97, 95% CI 0.66–1.41, p = 0.858, Table 2, Fig. 4). Significant increased risk of DSS was associated with older age (≥ 80 years), larger tumor size (≥ 89 mm), distant metastasis (M1), high and unknown mitotic rate, and lymphadenectomy (Table 2, Fig. 4).
Discussion
In this SEER-based matched cohort study, we found that patients with JI GISTs receiving LR has comparable survival outcome (both OS and DSS) to those receiving RR. Lymphadenectomy, age, tumor size, distant metastasis, mitotic rate, but not LR, were identified as independent prognostic factors for JI GISTs. Comparable survival outcome was accordant with these risk factors or in subgroup sensitivity analyses.
Although LR is recommended as first choice nowadays, patients with GISTs mainly underwent RR before the era of imatinib [1, 19]. Coincidently, we observed an increasing trend of LR in JI GISTs during the last three decades (1990–2003: 70.8%; 2004–2011: 76.8%; 2012–2019: 80.5%). Previous studies have shown that LR including endoscopic resection has advantages of function preserving, less complications, faster postoperative recovery and noninferior long-term survival compared with RR for GISTs [15, 17, 20]. Similarly, these findings have also been verified in population-based studies [16, 21,22,23]. However, the effect of LR on survival remains unknown for JI GISTs so far.
For JI tumors, RR with extensive bowel resection may lead to short bowel syndrome, a malabsorptive disorder with severe fatigue and gastrointestinal symptoms [24]. In addition, RR in distal ileum often involves resection of the ileocecal valve, leading to postoperative chronic diarrhea [25]. Preservation of mesenteric vessels has also been shown to reduce postoperative complications in JI tumors [26]. However, although RR is related with more postoperative complications and lower quality of life (QOL), it is performed instead of LR in many JI tumors from an oncologic point of view [27]. On the contrary, our study revealed that LR has comparable effect on both OS and DSS to RR for patients with JI GISTs (Fig. 2). Consistently, this result was observed within all subgroups (Fig. 3), as well as in multivariate analysis (Fig. 4). Considering that LR reduces complications and improves QOL, our findings implied that surgeons can choose LR in most JI GISTs patients without concerns for oncologic outcomes.
Interestingly, patients receiving LR has significant better DSS than those receiving RR before PSM (p = 0.0064, Fig. 2c). However, this finding should be attributed to the selection bias of surgical modality. From the unbalanced variables before PSM (Table 1), we could infer that surgeons tend to perform LR in patients with less aggressive tumors (having smaller size and more locoregional stage). In addition, we observed that LR was performed more frequently for ileal GISTs, probably due to the anatomical complexity of jejunum, especially the proximal part [28].
Tumor size, distant metastasis and mitotic rate have been proved to be prognostic factors for GISTs and included in several risk stratification systems [29]. Our study found the similar result that JI GISTs patients with tumor size ≥ 89 mm, distant metastasis, or high/unknown mitotic rate had worse survival. In addition, we also identified age and lymphadenectomy as independent prognostic factors for JI GISTs.
The prognostic role of age remains controversial for GISTs. Researchers found that older age is significantly correlated with poorer prognosis in retrospective studies [30,31,32], while others found it insignificant [33]. In multivariate analysis, compared with young patients (< 45 years old), patients over 80 years old had significant worse DSS (p < 0.001) but middle-age (45–79 years) also tended to be associated with poor prognosis (p = 0.060). In fact, recent studies suggested that GISTs might have distinct biology in younger patients [34]. The predictor effects of age on survival and the biological features of GISTs in different age groups are worth study.
Though discouraged for prophylactical purpose by most guidelines, performing lymphadenectomy in GISTs is controversial in case of enlarged regional lymph nodes [4, 35]. Previous SEER-based study found that lymphadenectomy is associated with poor survival of GISTs but the association was not observed in small intestinal GISTs [36]. We reported that lymphadenectomy is also a prognostic risk factor for JI GISTs (p = 0.016) and might be considered harmful. Nevertheless, this result needs further validation in at a finer scale studies given the limitation of population-based study.
There are some limitations in this SEER-based study. Firstly, the main limitation is that SEER database has shortcomings in information depth, lacking several important factors such as intraabdominal tumor rupture, margin status, and genetic mutation of KIT or PDGFRA. Although these factors are known to be associated with prognosis [1, 35, 37], inability to study them might influence our analysis. Furthermore, although integration of surgery with adjuvant imatinib therapy for GISTs has been proved to improve survival significantly, lack of information on regimen of chemotherapy in SEER Database hampered further investigation of imatinib in our cohort, underestimating its effect on survival. Secondly, this study did not include small intestinal GISTs with overlapping lesions, located at unspecified site, or located at Meckel diverticulum. However, given the rare incidence of these tumor, our findings might be generalized to most types of JI GISTs. Thirdly, GISTs might not be accurately diagnosed before GISTs-specific histologic code was applied in 2001. In early 2000s, the identification of GIST was fortified due to the progress in immunohistochemical diagnosis [38, 39]. However, 93.9% of our patients were diagnosed after 2001, ensuring a cohort with mostly reliable diagnosis. Lastly, our analysis had some biases inevitably as a retrospective study. However, while previous SEER-based studies used multivariate regression or PSM [21,22,23], the combination of both methodologies in our analysis further minimized the biases. Further prospective studies, especially multi-center randomized controlled trials, are needed to verify the effect of LR on JI GISTs. Evidence found in our report can be applied to guide future study design.
In conclusion, our study found that LR has comparable survival outcome to RR in patients with JI GISTs. To the best of our knowledge, this is the first study that compares the effect of different surgical modes on survival for patients with JI GISTs. Compared with single-center studies, our results might be better extrapolated to the general population given a larger sample size and longer follow-up. LR can be carried out safely without compromising oncological outcome, and should be considered as a treatment option in selected patients with JI GISTs.
Data availability
The datasets in this study were generated using data obtained from the SEER database, and are available at https://doi.org/10.6084/m9.figshare.22360540.v1.
References
Blay JY, Hindi N, Bollard J, Aguiar S Jr, Angel M, Araya B et al (2022) SELNET clinical practice guidelines for soft tissue sarcoma and GIST. Cancer Treat Rev 102:102312. https://doi.org/10.1016/j.ctrv.2021.102312
Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 23:70–83. https://doi.org/10.1053/j.semdp.2006.09.001
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67:93–99. https://doi.org/10.3322/caac.21388
von Mehren M, Kane JM, Riedel RF, Sicklick JK, Pollack SM, Agulnik M et al (2022) NCCN guidelines® insights: gastrointestinal stromal tumors, version 2.2022. J Natl Compr Canc Netw 20:1204–1214. https://doi.org/10.6004/jnccn.2022.0058
Han IW, Jang JY, Lee KB, Kang MJ, Kwon W, Park JW et al (2015) Clinicopathologic analysis of gastrointestinal stromal tumors in duodenum and small intestine. World J Surg 39:1026–1033. https://doi.org/10.1007/s00268-014-2810-x
Miettinen M, Makhlouf H, Sobin LH, Lasota J (2006) Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol 30:477–489. https://doi.org/10.1097/00000478-200604000-00008
Giuliano K, Nagarajan N, Canner J, Najafian A, Wolfgang C, Schneider E et al (2017) Gastric and small intestine gastrointestinal stromal tumors: Do outcomes differ? J Surg Oncol 115:351–357. https://doi.org/10.1002/jso.24514
Fernández JA, Ferreras D, Ruiz-Manzanera JJ, Olivares V, Ferri B, Frutos MD et al (2021) Characteristics and prognosis of jejunoileal gastrointestinal stromal tumours (GISTs) in the era of imatinib: a comparative study with gastric GISTs. Clin Transl Oncol 23:1368–1376. https://doi.org/10.1007/s12094-020-02528-y
Hamed H, Wahab MA, Elmahdy Y, El-Wahab RMA, El-Magd EA (2023) Gastrointestinal stromal tumors of the small intestine: the challenge of diagnosis and the outcome of management. World J Surg Oncol 21:85. https://doi.org/10.1186/s12957-023-02968-0
Liao CH, Yeh CN, Wang SY, Fu CY, Tsai CY, Liu YY et al (2015) Surgical option for intestinal gastrointestinal stromal tumors–perioperative and oncological outcomes of laparoscopic surgery. Anticancer Res 35:1033–1040
Etherington MS, DeMatteo RP (2019) Tailored management of primary gastrointestinal stromal tumors. Cancer 125:2164–2171. https://doi.org/10.1002/cncr.32067
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58. https://doi.org/10.1097/00000658-200001000-00008
McCarter MD, Antonescu CR, Ballman KV, Maki RG, Pisters PW, Demetri GD et al (2012) Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg 215:53–59; discussion 59–60. https://doi.org/10.1016/j.jamcollsurg.2012.05.008
Koo DH, Ryu MH, Kim KM, Yang HK, Sawaki A, Hirota S et al (2016) Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat 48:1155–1166. https://doi.org/10.4143/crt.2016.187
Lee SY, Goh BK, Sadot E, Rajeev R, Balachandran VP, Gönen M et al (2017) Surgical strategy and outcomes in duodenal gastrointestinal stromal tumor. Ann Surg Oncol 24:202–210. https://doi.org/10.1245/s10434-016-5565-9
Wei YZ, Cai ZB, Zhu CL, Zhou YM, Zhang XF (2021) Impact of surgical modalities on long-term survival outcomes of patients with duodenal gastrointestinal stromal tumor. Ann Surg Oncol 28:4668–4674. https://doi.org/10.1245/s10434-020-09497-0
Guo W, Yang Z, Wei Y, Qin X, Li C, Huang R et al (2020) Radical excision versus local resection for primary rectal gastrointestinal stromal tumors. Cohort Study. Int J Surg (London, England) 77:190–197. https://doi.org/10.1016/j.ijsu.2020.03.068
Randle RW, Ahmed S, Newman NA, Clark CJ (2014) Clinical outcomes for neuroendocrine tumors of the duodenum and ampulla of Vater: a population-based study. J Gastrointest Surg 18:354–362. https://doi.org/10.1007/s11605-013-2365-4
Cavnar MJ, Wang L, Balachandran VP, Antonescu CR, Tap WD, Keohan M et al (2017) Rectal gastrointestinal stromal tumor (GIST) in the era of imatinib: organ preservation and improved oncologic outcome. Ann Surg Oncol 24:3972–3980. https://doi.org/10.1245/s10434-017-6087-9
Wang C, Gao Z, Shen K, Cao J, Shen Z, Jiang K et al (2020) Safety and efficiency of endoscopic resection versus laparoscopic resection in gastric gastrointestinal stromal tumours: a systematic review and meta-analysis. Eur J Surg Oncol 46:667–674. https://doi.org/10.1016/j.ejso.2019.10.030
Yin L, Wang J, Zhao R, Chen K, Ji Z, Ji G et al (2022) Comparable long-term survival of patients with colorectal or gastric gastrointestinal stromal tumors treated with endoscopic vs. surgical resection. Surg Endosc 36:4215–4225. https://doi.org/10.1007/s00464-021-08755-w
Wei J, Zhong J, Chen Z, Huang Q, Wei F, Wang Q et al (2022) Survival outcome of local vs. radical excision in rectal gastrointestinal stromal tumor: a SEER database analysis. BMC Surg 22:21. https://doi.org/10.1186/s12893-022-01485-3
Yan H, Liu X, Yin L, Han H, Jin Y, Zhu X et al (2022) Effects of endoscopic therapy and surgical resection on long-term survival outcomes in patients with duodenal gastrointestinal stromal tumors: a surveillance, epidemiology, and end result program analysis. Surg Endosc 36:8030–8038. https://doi.org/10.1007/s00464-022-09231-9
Kalaitzakis E, Carlsson E, Josefsson A, Bosaeus I (2008) Quality of life in short-bowel syndrome: impact of fatigue and gastrointestinal symptoms. Scand J Gastroenterol 43:1057–1065. https://doi.org/10.1080/00365520802078325
Folaranmi S, Rakoczy G, Bruce J, Humphrey G, Bowen J, Morabito A et al (2011) Ileocaecal valve: how important is it? Pediatr Surg Int 27:613–615. https://doi.org/10.1007/s00383-010-2841-9
Bartsch DK, Windel S, Kanngießer V, Jesinghaus M, Holzer K, Rinke A et al (2022) Vessel-sparing lymphadenectomy should be performed in small intestine neuroendocrine neoplasms. Cancers (Basel). https://doi.org/10.3390/cancers14153610
Hallet J, Law C (2021) Extent of lymph node dissection for small bowel neuroendocrine tumors. World J Surg 45:197–202. https://doi.org/10.1007/s00268-020-05710-z
Meneses E, Elkbuli A, Baroutjian A, McKenney M, Boneva D (2020) Perforated proximal jejunal gastrointestinal stromal tumor pT4N0M0 presenting with severe sepsis: a case report and literature review. Ann Med Surg (Lond) 57:76–81. https://doi.org/10.1016/j.amsu.2020.07.024
Khoo CY, Chai X, Quek R, Teo MCC, Goh BKP (2018) Systematic review of current prognostication systems for primary gastrointestinal stromal tumors. Eur J Surg Oncol 44:388–394. https://doi.org/10.1016/j.ejso.2017.12.006
Liu X, Qiu H, Zhang P, Feng X, Chen T, Li Y et al (2018) Prognostic factors of primary gastrointestinal stromal tumors: a cohort study based on high-volume centers. Chin J Cancer Res 30:61–71. https://doi.org/10.21147/j.issn.1000-9604.2018.01.07
Cho MY, Sohn JH, Kim JM, Kim KM, Park YS, Kim WH et al (2010) Current trends in the epidemiological and pathological characteristics of gastrointestinal stromal tumors in Korea, 2003–2004. J Korean Med Sci 25:853–862. https://doi.org/10.3346/jkms.2010.25.6.853
Tran T, Davila JA, El-Serag HB (2005) The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol 100:162–168. https://doi.org/10.1111/j.1572-0241.2005.40709.x
Cavnar MJ, Seier K, Curtin C, Balachandran VP, Coit DG, Yoon SS et al (2021) Outcome of 1000 patients with gastrointestinal stromal tumor (GIST) treated by surgery in the pre- and post-imatinib eras. Ann Surg 273:128–138. https://doi.org/10.1097/SLA.0000000000003277
O’Connor DB, Conlon KC (2017) Gastrointestinal stromal tumors in younger patients: a start but more to do! JAMA Surg 152:451. https://doi.org/10.1001/jamasurg.2016.5048
Casali PG, Blay JY, Abecassis N, Bajpai J, Bauer S, Biagini R et al (2022) Gastrointestinal stromal tumours: ESMO-EURACAN-GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 33:20–33. https://doi.org/10.1016/j.annonc.2021.09.005
Li C, Su D, Xie C, Chen Q, Zhou J, Wu X (2019) Lymphadenectomy is associated with poor survival in patients with gastrointestinal stromal tumors. Ann Transl Med 7:558. https://doi.org/10.21037/atm.2019.09.60
Joensuu H, Vehtari A, Riihimäki J, Nishida T, Steigen SE, Brabec P et al (2012) Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. Lancet Oncol 13:265–274. https://doi.org/10.1016/S1470-2045(11)70299-6
Choi AH, Hamner JB, Merchant SJ, Trisal V, Chow W, Garberoglio CA et al (2015) Underreporting of gastrointestinal stromal tumors: is the true incidence being captured? J Gastrointest Surg 19:1699–1703. https://doi.org/10.1007/s11605-015-2860-x
Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ et al (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 33:459–465. https://doi.org/10.1053/hupa.2002.123545
Funding
This study was funded by Clinical Medical Team Introduction Program of Suzhou (SZYJTD201804); Science and Technology Development Project of Suzhou (SYSD2020111); and People’s Livelihood Science and Technology Project of Suzhou (SYSD2019105).
Author information
Authors and Affiliations
Contributions
Yongyou Wu, Wei Peng and Shangcheng Yan conceived and designed the study. Ming Cheng, Jingyu Zhang, Tianhua Liu, Mengchao Sheng, Rui Ren, and Qiang Chen collected and organized the data. Shangcheng Yan and Wei Peng analyzed and interpreted the data. Shangcheng Yan and Wei Peng drafted the manuscript. Yongyou Wu and Wei Gong revised and finalized the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study used publicly available de-identified data involving no human participants, and thus was granted exemption by the institutional review board at Second Affiliated Hospital of Soochow University.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yan, S., Peng, W., Cheng, M. et al. Survival outcome of local versus radical resection for jejunoileal gastrointestinal stromal tumors: a propensity score-matched population-based analysis. Int J Colorectal Dis 38, 253 (2023). https://doi.org/10.1007/s00384-023-04548-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04548-w