Abstract
Introduction
The complication rate after major abdominal surgery is from 35 to 50%. The multimodal prehabilitation covers all the pre-operative problems to guarantee a faster recovery and reduce the rate of morbidity and mortality after a colorectal procedure.
Methods
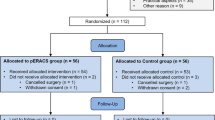
Observational study, in patients with CRC who underwent surgical treatment between November 2020 and September 2022. The data of the patients were placed in 2 groups: prehabilitation group (PPH) and no prehabilitation group (NPPH). Demographic data, type of cancer, operative data, and postoperative data were collected. Characteristics between the groups were compared after a propensity score matching (PSM) analysis for the detection of differences.
Results
After the PSM analysis, 46 patients were in PPH, and 63 patients were in NPPH. There was no significant difference in postoperative complications (p = 0.192). The median of comprehensive complication index (CCI) was 0 (p = 0.552). Patients in the NPPH had more hospital readmissions (p = 0.273) and more emergency room visits (p = 0.092). Multivariate log binomial regression adjusted for complications showed that pre-habilitation reduces the risk of a pos-operative complication (OR: 0.659, 95%CI, 0.434–1.00, p = 0.019).
Conclusions
The postoperative complication rate and LOS were similar between patients who receive operative multimodal prehabilitation for CRC surgery and those who did not. Prehabilitation was associated with reduced risk of postoperative complication after multivariate log binomial regression adjusted for complications. Patients who underwent prehabilitation had a slightly lower tendency for postoperative ER visits and hospital readmissions.



Similar content being viewed by others
Data availability
The datasets used during the current study is available from the corresponding author on reasonable request.
Material availability
No material from other sources was included in the article.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
van Rooijen S, Carli F, Dalton SO, Johansen C, Dieleman J, Roumen R, Slooter G (2017) Preoperative modifiable risk factors in colorectal surgery: an observational cohort study identifying the possible value of prehabilitation. Acta Oncol (Stockholm, Sweden) 56(2):329–334. https://doi.org/10.1080/0284186X.2016.1267872
Pouwels S, Stokmans RA, Willigendael EM, Nienhuijs SW, Rosman C, van Ramshorst B, Teijink JA (2014) Preoperative exercise therapy for elective major abdominal surgery: a systematic review. Int Surg J (London, England) 12(2):134–140. https://doi.org/10.1016/j.ijsu.2013.11.018
Kirchhoff P, Clavien PA, Hahnloser D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg 4(1):5. https://doi.org/10.1186/1754-9493-4-5
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102(5):462–479. https://doi.org/10.1002/bjs.9697
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248(2):189–198. https://doi.org/10.1097/SLA.0b013e31817f2c1a
Cavallaro P, Bordeianou L (2019) Implementation of an ERAS pathway in colorectal surgery. Clin Colon Rectal Surg 32(2):102–108. https://doi.org/10.1055/s-0038-1676474
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD et al (2019) Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS®) society recommendations: 2018. World J Surg 43(3):659–695. https://doi.org/10.1007/s00268-018-4844-y
de Queiroz FL, Lacerda-Filho A, Alves AC, de Oliveira FH, Neto PRF, de Almeida Paiva R (2021) Conditions associated with worse acceptance of a simplified accelerated recovery after surgery protocol in laparoscopic colorectal surgery. BMC Surg 21(1):229. https://doi.org/10.1186/s12893-021-01206-2
Steffens D, Beckenkamp PR, Hancock M, Solomon M, Young J (2018) Preoperative exercise halves the postoperative complication rate in patients with lung cancer: a systematic review of the effect of exercise on complications, length of stay and quality of life in patients with cancer. Br J Sports Med 52(5):344. https://doi.org/10.1136/bjsports-2017-098032
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, Kaneva P, Augustin B, Wongyingsinn M, Gamsa A, Kim DJ, Vassiliou MC, Feldman LS (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082. https://doi.org/10.1007/s00464-012-2560-5
Carli F, Charlebois P, Stein B, Feldman L, Zavorsky G, Kim DJ, Scott S, Mayo NE (2010) Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg 97(8):1187–1197. https://doi.org/10.1002/bjs.7102
Heger P, Probst P, Wiskemann J, Steindorf K, Diener MK, Mihaljevic AL (2020) A systematic review and meta-analysis of physical exercise prehabilitation in major abdominal surgery (PROSPERO 2017 CRD42017080366). Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 24(6):1375–1385. https://doi.org/10.1007/s11605-019-04287-w
Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R, Momblán D, Balust J, Blanco I, Martínez-Pallí G (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267(1):50–56. https://doi.org/10.1097/SLA.0000000000002293
Gillis C, Buhler K, Bresee L, Carli F, Gramlich L, Culos-Reed N, Sajobi TT, Fenton TR (2018) Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology 155(2):391-410.e4. https://doi.org/10.1053/j.gastro.2018.05.012
Munafò MR, Stevenson J (2001) Anxiety and surgical recovery. Reinterpreting the literature. J Psychosom Res 51(4):589–596. https://doi.org/10.1016/s0022-3999(01)00258-6
Bausys A, Kryzauskas M, Abeciunas V, Degutyte AE, Bausys R, Strupas K, Poskus T (2022) Prehabilitation in modern colorectal cancer surgery: a comprehensive review. Cancers (Basel) 14(20):5017. https://doi.org/10.3390/cancers14205017.PMID:36291801;PMCID:PMC9599648
Onerup A, Angenete E, Bock D, Haglind E (2022) Association between self-assessed preoperative level of physical activity and postoperative complications - an observational cohort analysis within a randomized controlled trial (PHYSSURG-C). Eur J Surg Oncol 48(4):883–889. https://doi.org/10.1016/j.ejso.2021.10.033
de Klerk M, van Dalen DH, Nahar-van Venrooij LMW, Meijerink WJHJ, Verdaasdonk EGG (2021) A multimodal prehabilitation program in high-risk patients undergoing elective resection for colorectal cancer: a retrospective cohort study. Eur J Surg Oncol 47(11):2849–2856. https://doi.org/10.1016/j.ejso.2021.05.033
Gillis C, Loiselle SE, Fiore J. F, Jr, Awasthi, R. Wykes L. Liberman AS, Stein B, Charlebois P, Carli F. Prehabilitation with whey protein supplementation on perioperative functional exercise capacity in patients undergoing colorectal resection for cancer: A pilot double-blinded randomized placebo-controlled trial. J Acad Nutr Diet 2016;116(5):802–812. https://doi.org/10.1016/j.jand.2015.06.007
Bousquet-Dion G, Awasthi R, Loiselle SÈ, Minnella EM, Agnihotram RV, Bergdahl A, Carli F, Scheede-Bergdahl C (2018) Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol (Stockholm, Sweden) 57(6):849–859. https://doi.org/10.1080/0284186X.2017.1423180
Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B, Denehy L. Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: A systematic review and meta-analysis. Frontiers Surg 2021;8:628848. https://doi.org/10.3389/fsurg.2021.628848
Husebø AML, Karlsen B, Husebø SE. Health professionals' perceptions of colorectal cancer patients' treatment burden and their supportive work to ameliorate the burden - a qualitative study. BMC Health Serv Res 2020;20(1):661. https://doi.org/10.1186/s12913-020-05520-y
Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, Stein B, Charlebois P, Ghitulescu G, Morin N, Jagoe T, Scheede-Bergdahl C, Minnella EM, Fiore JF, Jr. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-Day postoperative complications for frail patients undergoing resection of colorectal cancer: A randomized clinical trial. JAMA Surgery 2020;155(3):233–242. https://doi.org/10.1001/jamasurg.2019.5474
Karlsson E, Farahnak P, Franzén E, Nygren-Bonnier M, Dronkers J, van Meeteren N, Rydwik E. Feasibility of preoperative supervised home-based exercise in older adults undergoing colorectal cancer surgery - A randomized controlled design. PloS one 2019;14(7):e0219158. https://doi.org/10.1371/journal.pone.0219158
van Rooijen S, Carli F, Dalton S, Thomas G, Bojesen R, Le Guen M, Barizien N, Awasthi R, Minnella E, Beijer S, Martínez-Palli G, van Lieshout R, Gögenur I, Feo C, Johansen C, Scheede-Bergdahl C, Roumen R, Schep G, Slooter G (2019) Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: the first international randomized controlled trial for multimodal prehabilitation. BMC Cancer 19(1):98. https://doi.org/10.1186/s12885-018-5232-6
Funding
This review received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception and design: DL and LG. Conducted research: FL. Data analysis and interpretation: DL, FL, PR, AL, SS, and JC. Manuscript writing and final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Estrada, D.M.L., de Queiroz, F.L., Guerra, L.I. et al. Comparative study using propensity score matching analysis in patients undergoing surgery for colorectal cancer with or without multimodal prehabilitation. Int J Colorectal Dis 38, 256 (2023). https://doi.org/10.1007/s00384-023-04547-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04547-x