Abstract
Background
The standard operation for mid- and low rectal cancer total mesorectal excision (TME) is routinely performed as minimally invasive surgery. TME is associated with temporary or permanent functional impairment of pelvic organs, causing reduced quality of life (QoL). Concerns have been raised that the newest minimally invasive approach, transanal TME (TaTME), may further reduce urogenital and anorectal functions.
Objective
To determine if functional outcomes affecting QoL are altered after TaTME. Primary end-point is the impact of TaTME on QoL and functional outcomes. Secondary end-point is assessing differences in QoL and functional outcomes after TME surgery from below (TaTME) or above (transabdominal TME).
Design, setting, and participants
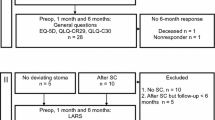
Observational study consisting of prospectively registered self-reported questionnaire data collected at baseline and follow-ups after TaTME. All patients who underwent TaTME during the Danish national implementation phase were included. Central surveillance of the implementation included questionnaires concerning QoL and functional outcomes. Analyses of functional results from the Danish cohort of the ROLARR trial (Jayne et al. in JAMA 318:1569–1580, (2017) are reported separately for perspective, representing the transabdominal approach to TME, i.e., laparoscopic- or robotic-assisted TME (LaTME/RoTME). Applied questionnaires include EORTC QLQ-C30, SF-36, LARS, ICIQ-MLUTS, ICIQ-FLUTS, IPSS, IIEF, SVQ, and FSFI.
Results
A total of 115 TaTME procedures were registered August 2016 to April 2019. LaTME/RoTME patients (n = 92) were operated on January 2011 to September 2014. A temporary postoperative decrease of QoL (global health status and functional scales) was observed, yet long-term results were unaffected by surgery in both groups. In TaTME patients, the anorectal dysfunction increased significantly (p < 0.001) from preoperative baseline to 13.5 months follow-up, where 67.5% (n = 52) reported major LARS symptoms. Urinary function was not significantly impaired after TME regardless of technique. The paucity of responses concerning sexual function precludes conclusions.
Conclusions
Although an initial reduction in QoL after TME occurs, it normalizes within the first year postoperatively. In concurrence with international results, we found that significant anorectal dysfunction is common after TaTME. No data on anorectal function was available for LaTME/RoTME patients for comparison. We found no indications that transanal TME is inferior to transabdominal TME surgery concerning urogenital functions or health-related QoL.




Similar content being viewed by others
Availability of data and materials
The manuscript contains third party material and obtained permissions are available on request by the publisher.
References
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580. https://doi.org/10.1001/jama.2017.7219
Veltcamp Helbach M, Koedam TWA, Knol JJ, Velthuis S, Bonjer HJ, Tuynman JB et al (2019) Quality of life after rectal cancer surgery: differences between laparoscopic and transanal total mesorectal excision. Surg Endosc 33:79–87. https://doi.org/10.1007/s00464-018-6276-z
van der Heijden JAG, van de Pas KGH, van den Broek FJC, van Dielen FMH, Slooter GD, Maaskant-Braat AJG (2022) Oncological and functional outcomes of transanal total mesorectal excision in a teaching hospital in the Netherlands. Ann Coloproctology 38:28–35. https://doi.org/10.3393/ac.2020.00773.0110
Perdawood SK, Thinggaard BS, Bjoern MX (2018) Effect of transanal total mesorectal excision for rectal cancer: comparison of short-term outcomes with laparoscopic and open surgeries. Surg Endosc 32:2312–2321. https://doi.org/10.1007/s00464-017-5926-x
Roodbeen SX, Spinelli A, Bemelman WA, Di Candido F, Cardepont M, Denost Q et al (2020) Local recurrence after transanal total mesorectal excision for rectal cancer: a multicenter cohort study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003757
Fernández-Martínez D, Rodríguez-Infante A, Otero-Díez JL, Baldonedo-Cernuda RF, Mosteiro-Díaz MP, García-Flórez LJ (2020) Is my life going to change?-a review of quality of life after rectal resection. J Gastrointest Oncol 11:91–101. https://doi.org/10.21037/jgo.2019.10.03
Rasmussen OO, Petersen IK, Christiansen J (2003) Anorectal function following low anterior resection. Colorectal Dis Off J Assoc Coloproctology G B Irel 5:258–261
Allaix ME, Rebecchi F, Giaccone C, Mistrangelo M, Morino M (2011) Long-term functional results and quality of life after transanal endoscopic microsurgery. Br J Surg 98:1635–1643. https://doi.org/10.1002/bjs.7584
van der Sande ME, Hupkens BJP, Berbée M, van Kuijk SMJ, Maas M, Melenhorst J et al (2019) Impact of radiotherapy on anorectal function in patients with rectal cancer following a watch and wait programme. Radiother Oncol J Eur Soc Ther Radiol Oncol 132:79–84. https://doi.org/10.1016/j.radonc.2018.11.017
De Nardi P, Testoni SGG, Corsetti M, Andreoletti H, Giollo P, Passaretti S et al (2017) Manometric evaluation of anorectal function in patients treated with neoadjuvant chemoradiotherapy and total mesorectal excision for rectal cancer. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver 49:91–97. https://doi.org/10.1016/j.dld.2016.09.005
Hirata Y, Nozawa H, Kawai K, Hata K, Tanaka T, Nishikawa T et al (2020) The influence of neoadjuvant chemoradiation for middle and lower rectal cancer on anorectal function. Anticancer Res 40:2199–208. https://doi.org/10.21873/anticanres.14181
Kye B-H, Kim H-J, Kim J-G, Kim S-H, Shim B-Y, Lee N-S et al (2013) Short-term effects of neoadjuvant chemoradiation therapy on anorectal function in rectal cancer patients: a pilot study. Radiat Oncol Lond Engl 8:203. https://doi.org/10.1186/1748-717X-8-203
Klein MF, Seiersen M, Bulut O, Bech-Knudsen F, Jansen JE, Gögenur I (2020) Short-term outcomes after transanal total mesorectal excision for rectal cancer in Denmark - a prospective multicentre study. Colorectal Dis Off J Assoc Coloproctology G B Irel. https://doi.org/10.1111/codi.15454
Ingeholm P, Gogenur I, Iversen LH (2016) Danish colorectal cancer group database. Clin Epidemiol 8:465–468. https://doi.org/10.2147/CLEP.S99481
Fayers PM AN, Bjordal K et al (2001) The EORTC QLQ-C30 scoring manual (3rd Edition). Eur Organ Res Treat Cancer
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255:922–928. https://doi.org/10.1097/SLA.0b013e31824f1c21
Croese AD, Lonie JM, Trollope AF, Vangaveti VN, Ho Y-H (2018) A meta-analysis of the prevalence of low anterior resection syndrome and systematic review of risk factors. Int J Surg Lond Engl 56:234–241. https://doi.org/10.1016/j.ijsu.2018.06.031
ICIQ Group [Internet]. North Bristol NHS (UK): Questionnaires for urinary, vaginal & bowel dysfunctions; 2004 [updated 2022; cited 2021 Feb 4]. Available from: https://iciq.net/
Coyne K, Kelleher C (2010) Patient reported outcomes: the ICIQ and the state of the art. Neurourol Urodyn 29:645–651. https://doi.org/10.1002/nau.20911
Jensen PT, Klee MC, Thranov I, Groenvold M (2004) Validation of a questionnaire for self-assessment of sexual function and vaginal changes after gynaecological cancer. Psychooncology 13:577–592. https://doi.org/10.1002/pon.757
Bjoern MX, Nielsen S, Perdawood SK (2019) Quality of life after surgery for rectal cancer: a comparison of functional outcomes after transanal and laparoscopic approaches. J Gastrointest Surg Off J Soc Surg Aliment Tract. https://doi.org/10.1007/s11605-018-4057-6
Choy KT, Yang TWW, Prabhakaran S, Heriot A, Kong JC, Warrier SK (2021) Comparing functional outcomes between transanal total mesorectal excision (TaTME) and laparoscopic total mesorectal excision (LaTME) for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. https://doi.org/10.1007/s00384-021-03849-2
Heijden JA, Koëter T, Smits LJ, Sietses C, Tuynman JB, Maaskant-Braat AJ, Klarenbeek BR, Wilt JH (2020) Functional complaints and quality of life after transanal total mesorectal excision: a meta-analysis. Br J Surg 107:489–98. https://doi.org/10.1002/bjs.11566
Camilleri-Brennan J, Steele RJ (1998) Quality of life after treatment for rectal cancer. Br J Surg 85:1036–1043. https://doi.org/10.1046/j.1365-2168.1998.00808.x
Deijen CL, Tsai A, Koedam TWA, Veltcamp Helbach M, Sietses C, Lacy AM et al (2016) Clinical outcomes and case volume effect of transanal total mesorectal excision for rectal cancer: a systematic review. Tech Coloproctology 20:811–824. https://doi.org/10.1007/s10151-016-1545-0
Lee L, Kelly J, Nassif GJ, deBeche-Adams TC, Albert MR, Monson JRT (2020) Defining the learning curve for transanal total mesorectal excision for rectal adenocarcinoma. Surg Endosc 34:1534–1542. https://doi.org/10.1007/s00464-018-6360-4
Sylla P, Knol JJ, D’Andrea AP, Perez RO, Atallah SB, Penna M et al (2019) Urethral injury and other urologic injuries during transanal total mesorectal excision: an international collaborative study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003597
Park SY, Choi G-S, Park JS, Kim HJ, Ryuk J-P, Yun S-H (2014) Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg 38:1834–1842. https://doi.org/10.1007/s00268-013-2419-5
Vironen JH, Kairaluoma M, Aalto A-M, Kellokumpu IH (2006) Impact of functional results on quality of life after rectal cancer surgery. Dis Colon Rectum 49:568–578. https://doi.org/10.1007/s10350-006-0513-6
Junginger T, Kneist W, Heintz A (2003) Influence of identification and preservation of pelvic autonomic nerves in rectal cancer surgery on bladder dysfunction after total mesorectal excision. Dis Colon Rectum 46:621–628. https://doi.org/10.1007/s10350-004-6621-2
Lange MM, Maas CP, Marijnen C a. M, Wiggers T, Rutten HJ, Kranenbarg EK et al (2008) Urinary dysfunction after rectal cancer treatment is mainly caused by surgery. Br J Surg 95:1020–1028. https://doi.org/10.1002/bjs.6126
Pontallier A, Denost Q, Van Geluwe B, Adam J, Celerier B, Rullier E (2016) Potential sexual function improvement by using transanal mesorectal approach for laparoscopic low rectal cancer excision. Surg Endosc 30:4924–4933. https://doi.org/10.1007/s00464-016-4833-x
Acknowledgements
The authors wish to thank Dr. Jayne et al., authors of the ROLARR trial [1], for supplying raw data from the Danish cohort. Furthermore, we thank the Scientific Committee of the Danish Colorectal Cancer Group (DCCG.dk) for its collaboration.
Funding
Dr. Bjoern was partially supported by the Louis-Hansen Foundation (private foundation). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
MXB and MFK wrote the main manuscript text and MXB prepared all figures and tables. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bjoern, M., Clausen, F., Seiersen, M. et al. Quality of life and functional outcomes after transanal total mesorectal excision for rectal cancer—results from the implementation period in Denmark. Int J Colorectal Dis 37, 1997–2011 (2022). https://doi.org/10.1007/s00384-022-04219-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04219-2