Abstract
Purpose
Surgery is the main treatment for non-metastatic colorectal cancer. Despite huge improvements in perioperative care, colorectal surgery is still associated with a significant burden of postoperative complications and ultimately costs for healthcare organizations. Systematic clinical auditing activity has already proven to be effective in measuring and improving clinical outcomes, and for this reason, we decided to evaluate its impact in a large area of northern Italy.
Methods
The Emilia-Romagna Surgical Colorectal Audit (ESCA) is an observational, multicentric, retro-prospective study, carried out by 7 hospitals located in the Emilia-Romagna region. All consecutive patients undergoing surgery for colorectal cancer during a 54-month study period will be enrolled. Data regarding baseline conditions, preoperative diagnostic work-up, surgery and postoperative course will be collected in a dedicated case report form. Primary outcomes regard postoperative complications and mortality. Secondary outcomes include each center’s adherence to the auditing (enrolment rate) and evaluation of the systematic feedback activity on key performance indicators for the entire perioperative process.
Conclusion
This protocol describes the methodology of the Emilia-Romagna Surgical Colorectal Audit. The study will provide real-world clinical data essential for benchmarking and feedback activity, to positively impact outcomes and ultimately to improve the entire healthcare process of patients undergoing colorectal cancer surgery.
Clinical trial registration
The study ESCA is registered on the clinicaltrials.gov platform (Identifier: NCT03982641).
Similar content being viewed by others
Introduction
“If you can not measure it, you can not improve it” (Lord Kelvin)
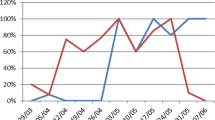
A clinical audit is a process which assesses whether healthcare is meeting standards, with the capacity to reduce care disparities as well as being a method to cut unnecessary costs. Where indicated, changes are implemented at an individual, team, or service level, and further monitoring is used to confirm improvement in healthcare delivery [1]. Reliable data, meticulous measurement, and systematic feedback to participants about their performances are the three pillars at the base of an effective clinical audit. Only good data can bring understanding of what does and does not improve the quality of healthcare, and a continuous assessment process allows for concrete advancement (Fig. 1).
The so-called “Hawthorne effect” (the awareness of being monitored positively influences the behavior of monitored individuals) also helps improve the process, as already widely demonstrated [2,3,4,5,6].
Medical literature offers a vast number of international clinical audits focused on colorectal cancer surgery [7,8,9,10]. The Dutch Colorectal Audit (DCRA) probably represents one of the most effective initiatives aiming at improving surgical quality outcomes [7]. DCRA started in 2009 and after just 8 years of activity more than 70,000 patients were included, showing a dramatic decrease in postoperative mortality from 3.4 to 1.8% for colon cancer and from 2.3 to 1% for rectal cancer [10]. Moreover, a significant reduction in costs for the entire healthcare system was observed along with a reduction in complications [11] and an optimization of resources such as the reduction in preoperative radiation therapy for rectal cancer without any impact on oncological outcomes[12].
In 2020, more than 43,000 people in Italy were diagnosed with colorectal cancer (CRC). Of these, approximately 800 of them lived in proximity of the centers taking part in this study [13]. Looking at the administrative data of the Emilia-Romagna region, huge variability was also observed in terms of volume and surgical outcomes, ranging respectively from 36 to 290 procedures per hospital and 2.26% up to 9.45% for 30-day mortality [14].
Following the path of the DCRA experience and given the heterogeneity of surgical outcomes among the hospitals in our region, we decided for the first time in Italy to promote a systematic clinical auditing pilot study focused on CRC surgical care and its possible benefit on outcomes.
Methods
Data governance and ethics
The protocol has been described according to the Standard Protocol Items: Recommendation for the Investigational Trials (SPIRIT) checklist [15] (Appendix). The ethical committee approved the project for each of the centers taking part according to local regulations, and it has been registered on the clinicaltrials.gov platform (Identifier: NCT03982641). The Romagna Ethical Committee (CEROM) approval number is 2278.
Study organization, administration, and governance
The Emilia-Romagna Surgical Colorectal Audit (ESCA) is a multicenter, retro-prospective, observational non-profit study promoted by the IRCCS Istituto Romagnolo per lo Studio dei Tumori (IRST) “Dino Amadori” in Meldola and the Local Health Agency of Romagna (AUSL Romagna).
Members of the surgical units participating in the study contributed to its design gave feedback and reviewed the study protocol. ESCA is overseen by a study steering committee composed of surgeons, epidemiologists, statisticians, IT specialists, and healthcare administrators.
ESCA received a financial support from Johnson & Johnson Medical S.p.a Ethicon Division for data management and monitoring.
The objectives of the study are as follows:
-
1.
To systematically collect data of all patients undergoing surgical treatment for primary CRC from diagnosis up to 6 months after surgery;
-
2.
To evaluate risk adjusted post-operative complications and mortality;
-
3.
To evaluate adherence to the clinical audit activity of each participating center;
-
4.
To evaluate the possible positive effects on outcomes, both clinical and economic, of systematic measurement and monitoring (Hawthorne effect).
Setting and study population
Patients will be enrolled from the 7 hospitals located in the Emilia-Romagna region in Northern Italy (Table 1), during a 54-month study period. The recruitment target is around 800 patients per year on the basis of demographic data reported in previous years.
Inclusion criteria
All consecutive patients undergoing surgery for primary CRC between 15 April 2019 and 31 December 2023 will be enrolled in the study. All types of surgical procedures are included, irrespective of setting (urgent/emergent or elective), intent (curative or palliative), and approach (open or minimally invasive). Eligible patients are asked to sign an informed consent form. Cognitive impairment is not considered an exclusion criterion if informed consent is obtained by an appropriate healthcare proxy.
Exclusion criteria
Patients with multiple synchronous primary tumors are excluded from the analysis. Patients who are unwilling to sign an informed consent form are also excluded.
Patient’s withdrawal
Participating subjects have the right to withdraw at any time for any reason; data will be collected until the patient’s withdrawal point.
Study outcomes
The primary objective of this analysis is to assess the frequency of post-operative complications, unplanned re-interventions, re-admissions, and mortality rates (at 30, 90, and 180 days after surgery).
Secondary outcomes include adherence to the clinical audit by each center (intended as the percentage of enrolled eligible patients) along with the study timeframe and possible positive effects on outcomes, both clinical and economic, of systematic measurement and monitoring.
Key performance indicators, case-mix, benchmarking, and feed-back activity
A core set of key performance indicators (KPIs) will be assessed to measure performance and evaluate the quality of colorectal cancer surgery across the participating centers (Table 2). Each KPI will be estimated both as unadjusted and risk adjusted for differences in patients’ characteristics for a fair comparison among the participating hospitals.
Every 12 months, an anonymized report on volume and KPIs will be delivered to each hospital comparing data of all the participating centers. A set of relevant case-mix variables (patients’ frailty, tumor burden, type of surgery) will be also identified in order to produce a reliable comparison of outcomes between hospitals and give each center case-mix adjusted outcomes.
Data collected during the first 18 months (from April 2019 to October 2020) will be analyzed in order to evaluate preliminary results on primary and secondary outcomes. The first preliminary analysis will be used as benchmark to further implement the auditing activity.
Case-mix adjusted data will be presented using funnel plots with a 95% confidence interval (Fig. 2).
Reports of the enrolment rate, obtained by comparing the number of enrolled patients to the hospital discharge cards (HDC), will be sent to each center every 3 months. The aim of this feedback activity is to progressively obtain a 100% enrolment of eligible patients and thus provide “real-world data” that avoid bias related to patient selection.
Data collection and quality control
The data collection and management for this paper are performed using the OpenClinica open-source software for Electronic Data Capture (EDC), version 3.1 (Copyright OpenClinica LLC and collaborators, Waltham, MA, USA, www.OpenClinica.com). Case report forms are filled in for each patient by trained healthcare providers (attendings, residents) or properly trained data managers. Operative and postoperative data are retrieved both from electronic medical charts and administrative databases. Surgical data analysis, including detection of postoperative complications, will be done under the supervision of a staff surgeon.
Quality control and data authenticity will be performed by data managers and clinical research coordinators. Clinical data will be compared to routinely collect administrative information retrieved from regional registries to ensure reliability and completeness and to avoid selection bias. Registration of each patient is automatically linked to the regional administration database, which by law receives notification on all patients deceased in Emilia-Romagna.
Study variables
The full data set is composed of up to 172 possible variables, and it is organized in sections as follows.
Preoperative assessment
Preoperative functional assessment is conducted using the Eastern Collaborative Oncology Group Performance Status (ECOG PS) [16] and the American Society of Anaesthesiology (ASA) score [17, 18]. Patients aged ≥ 70 years are screened for frailty with the Katz Activities of Daily Living (ADL) [19] and the Flemish version of the Triage Risk Screening Tool (fTRST) [20, 21]. Comorbidities are assessed using the age adjusted Charlson Comorbidity Index (CCI) [22, 23] and the presence of malnourishment is evaluated using the nutritional risk score (NRS) [24]. All screening tests are reported in detail in Table 3. Baseline evaluation further includes information on the living conditions before surgery and polypharmacy.
The diagnostic work-up is then assessed including the following items:
-
1.
Number and location of primary cancer;
-
2.
Presence/absence of distant metastases;
-
3.
Date of preoperative endoscopy and pathology report of biopsy;
-
4.
Presence of cancer-related preoperative complications (anemia, colonic obstruction, perforation);
-
5.
Date and type of preoperative imaging studies (CT scan, MRI, PET-CT) as appropriate.
For rectal cancer patients undergoing pelvic MRI and/or neoadjuvant treatments, specific items will be also collected as reported in Table 4.
Surgery
Type of surgical procedure, regimen, length of surgery, and operative technique is collected. Possible intraoperative complications are identified and specified as well as the need for intraoperative blood transfusions. The radicality of surgery is assessed as well as type of anastomosis including characteristics and technique. If stoma is created, details are reported as appropriate. All surgical items are reported in detail in Table 5.
Postoperative course
Need of the post-operative intensive care unit (ICU), length of ICU stay, postoperative LOS, and discharge settings are all registered. Thirty-day postoperative morbidity is collected and classified according to Clavien–Dindo classification [25, 26]. Cumulative burden of postoperative complications is calculated for each patient according to the comprehensive complication index [27]. If re-intervention is needed, the reason for reintervention, operative procedure, approach, and need for postoperative ICU stay are all collected (Table 6).
Pathology
The pathology report includes cancer type and grade of differentiation according to the WHO classification [28], the number of retrieved and positive lymph-nodes, and lympho-vascular and perineural invasion. For patients with rectal cancer, additional information includes extra mural vascular invasion (EMVI), evaluation of distal and circumferential margins, TME quality according to the Quirke classification [29, 30], and grade of regression following neoadjuvant treatment according to Ryan/CAP [31]. Final tumor stage is reported according to the 7th edition of the TNM cancer staging system [32] (Table 7).
Follow-up
After hospital discharge, any postoperative oncological treatment will be reported (adjuvant chemotherapy and/or radiation therapy). Possible changes in living conditions, considered as a proxy for functional recovery, will be reported. Any emergency department access until postoperative day 30 and the reason for it will be collected as well as the need for re-hospitalization. Mortality at 30, 90, and 180 days postoperatively will be collected, together with the cause of death (Table 8).
Statistical considerations
All the analyses will be performed considering tumor location (colon or rectum) as a stratification factor. For continuous variables, the arithmetic mean and standard deviation (SD), as well as the median value and minimum–maximum, will be presented. Absolute frequencies together with the percentage relative frequencies will be reported while summarizing qualitative variables.
To evaluate the performance of surgical activity, absolute numbers and relative percentages of each performance indicator reported will be calculated. The mortality rate will be defined as the number of patients who died within 30, 90, and 180 days after surgery. Graphical representation will also be used: funnel plots will be displayed for each KPI, both in unadjusted and adjusted versions.
Appropriate statistical models (i.e., mixed models, logistical regression, multilevel models) will be developed to evaluate the relationship among analyzed indicators and potential explanatory factors as well as for standardization/adjustment purposes. Main covariates will include age, gender, ASA score, CCI, surgery setting (urgent vs. elective), and ECOG.
Hospitals will be used as random effects to account for the presence of possible variability among hospitals. Other exploratory subgroup analyses will be performed.
Furthermore, to assess the effects of continuous monitoring and benchmarking on clinical outcomes, a before-and-after approach will be used. Specifically, assuming the time from the first subject surgery until the release of the first benchmarking report as the reference period (baseline, i.e., “before” period), the analysis will evaluate any significant changes occurred afterwards. Any changes on the outcomes will be, therefore, attributed to the benchmarking effect.
Missing values will be replaced and estimated using multiple imputations. A two-sided 95% confidence interval (95% CI) will be reported as appropriate.
Statistical analysis will be performed using R statistical software (v. 4.0.6) — www.r-project.org.
Discussion
Surgery is the main treatment modality for stages I–III colorectal cancer and frequently represents the most effective choice even in a palliative setting. Despite massive improvements in perioperative care and techniques, colorectal cancer surgery is still associated with a significant burden of postoperative complications which result in greater healthcare costs and severe functional sequalae for patients. If the value of healthcare is maximizing quality care at minimal cost [33], the large-scale participation in an audit, which constantly measure the care quality and the resources used associated for a benchmark feedback, represents a unique opportunity to significantly improve healthcare and limit expenditure.
Administrative data have already revealed their limitations when used to evaluate quality of care and can lead to misinterpretation when used to measure composite postoperative outcomes of complex and/or frail patients [34, 35]. However, together with mortality registries, they are essential for quality check control (enrollment rate) and completeness of data entry for specific items (re-admission rate, emergency department admission after discharge): for this reason, they were integrated into the entire ESCA auditing process.
Clinical data are more difficult and expensive to collect than administrative data, but these challenges are far outweighed by the opportunity clinical data can create in obtaining reliable information on the entire clinical process, ultimately improving quality and reducing hospital costs, as has been demonstrated by previously validated large national clinical audits such as NSQuIP [36] and DCRA [10]. The Dutch experience, thanks to the inclusion of the entire colorectal surgery population, represents to date, the most meaningful one given its “real-world” nature without selection bias and with risk-adjusted outcome data.
ESCA is an initiative which follows one of the main recommendations of the European Cancer Care Organization (ECCO) — Essential Requirements for Quality Cancer Care (ERQCC). The ERQCC recommended that clinical and process outcome data should be systematically measured and collected to give high quality care to patients [37].
With the paramount of a concrete enhancement of postoperative outcomes and a reduction of costs, ESCA aims to investigate, for the first time in Italy, the impact of systematic clinical auditing and feedback in the field of colorectal cancer surgery among a large population representative of a real-world population. Key performance indicators based on evidence-based guidelines, web-based registration of clinical data made by physicians integrated with administrative data and continuous feedback on the enrolment, and risk-adjusted outcomes are the critical elements of the study, which will provide strong and reliable data to measure and improve quality of colorectal cancer surgical care.
Future challenges will be to enhance this project at regional or national level and will use our experience to set regional and national quality standards.
References
Burgess R, Moorhead J (2020) New principles of best practice in clinical audit. Burgess, R (ed) 2nd ed. CRC Press. ISBN 9781003155393
McCambridge J, Witton J, Elbourne DR (2014) Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 67:267–277. https://doi.org/10.1016/j.jclinepi.2013.08.015
Govednik J, McGuckin M (2011) A Multicenter trend analysis of hand hygiene event rates in USA pre- and post joint commission and World Health Organization guidelines. Am J of Infect Control 39:E104–E105. https://doi.org/10.1016/j.ajic.2011.04.187
Mangione-Smith R, Elliott MN, McDonald L, McGlynn EA (2002) An observational study of antibiotic prescribing behavior and the Hawthorne effect. Health Serv Res 37:1603–1623. https://doi.org/10.1111/1475-6773.10482
Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, Knight TK, Hay JW, Doctor JN (2016) Effect of Behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA 315:562–570. https://doi.org/10.1001/jama.2016.0275
van de Graaf FW, Lange MM, Spakman JI, van Grevenstein WMU, Lips D, de Graaf EJR, Menon AG, Lange JF (2019) Comparison of systematic video documentation with narrative operative report in colorectal cancer surgery. JAMA Surg 154:381–389. https://doi.org/10.1001/jamasurg.2018.5246
Van Leersum NJ, Snijders HS, Henneman D, Kolfschoten NE, Gooiker GA, Ten Berge MG, Eddes EH, Wouters MW, Tollenaar RA, Bemelman WA, Van Dam RM (2013) The Dutch surgical colorectal audit. Eur J Surg Oncol 39:1063–1070. https://doi.org/10.1016/j.ejso.2013.05.008
Bakker IS, Snijders HS, Wouters MW, Havenga K, Tollenaar RAEM, Wiggers T, Dekker JWT (2014) High complication rate after low anterior resection for mid and high rectal cancer; results of a population-based study. Eur J Surg Oncol 40:692–698. https://doi.org/10.1016/j.ejso.2014.02.234
Zerillo JA, Schouwenburg MG, van Bommel ACM, Stowell C, Lippa J, Bauer D, Berger AM, Boland G, Borras JM, Buss MK et al (2017) An international collaborative standardizing a comprehensive patient-centered outcomes measurement set for colorectal cancer. JAMA Oncol 3:686–694. https://doi.org/10.1001/jamaoncol.2017.0417
de Neree Tot Babberich MPM, Detering R, Dekker JWT, Elferink MA, Tollenaar RAEM, Wouters MWJM, Tanis PJ, de Neree MPM, Detering R, Willem J et al (2018) Achievements in colorectal cancer care during 8 years of auditing in The Netherlands. Eur J Surg Oncol 44:1361–1370. https://doi.org/10.1016/j.ejso.2018.06.001
Govaert JA, van Dijk WA, Fiocco M, Scheffer AC, Gietelink L, Wouters MWJM, Tollenaar RAEM (2016) Nationwide outcomes measurement in colorectal cancer surgery: improving quality and reducing costs. J Am Coll of Surg 222:19-29.e2. https://doi.org/10.1016/j.jamcollsurg.2015.09.020
Gietelink L, Wouters MWJM, Marijnen CAM, van Groningen J, van Leersum N, Beets-Tan RGH, Tollenaar RAEM, Tanis PJ (2017) Changes in nationwide use of preoperative radiotherapy for rectal cancer after revision of the national colorectal cancer guideline. Eur J Surg Oncol 43:1297–1303. https://doi.org/10.1016/j.ejso.2016.12.019
AIOM, AIRTUM (2020) SIAPEC-IAP. I numeri del cancro in Italia 2020. Available on line: https://www.aiom.it/wp-content/uploads/2020/10/2020_Numeri_Cancro-operatori_web.pdf. Accessed 28 March 2022
Italian Ministry of Health. Programma Nazionale Esiti. Available online: https://pne.agenas.it/main/doc/Report_PNE_2021.pdf. Accessed 28 March 2022
Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, Hróbjartsson A, Mann H, Dickersin K, Berlin JA et al (2013) SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 158:200–207. https://doi.org/10.7326/0003-4819-158-3-201302050-00583
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Keats AS (1978) The ASA classification of physical status–a recapitulation. Anesthesiology 49:233–236
Owens WD, Felts JA, Spitznagel ELJ (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243. https://doi.org/10.1097/00000542-197810000-00003
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA 185:914–919. https://doi.org/10.1001/jama.1963.03060120024016
Deschodt M, Wellens NIH, Braes T, De Vuyst A, Boonen S, Flamaing J, Moons P, Milisen K (2011) Prediction of functional decline in older hospitalized patients: a comparative multicenter study of three screening tools. Aging Clin Exp Res 23:421–426. https://doi.org/10.1007/BF03325237
Zattoni D, Montroni I, Saur NM, Garutti A, Bacchi Reggiani ML, Galetti C, Calogero P, Tonini V (2019) A simple screening tool to predict outcomes in older adults undergoing emergency general surgery. J Am Geriatr Soc 67:309–316. https://doi.org/10.1111/jgs.15627
Chang C-M, Yin W-Y, Wei C-K, Wu C-C, Su Y-C, Yu C-H, Lee C-C (2016) Adjusted age-adjusted Charlson comorbidity index score as a risk measure of perioperative mortality before cancer surgery. PLoS One 11:e0148076. https://doi.org/10.1371/journal.pone.0148076
Tian Y, Jian Z, Xu B, Liu H (2017) Age-adjusted Charlson comorbidity index score as predictor of survival of patients with digestive system cancer who have undergone surgical resection. Oncotarget 8:79453–79461. https://doi.org/10.18632/oncotarget.18401
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z (2003) Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr (Edinburgh, Scotland) 22:321–336. https://doi.org/10.1016/s0261-5614(02)00214-5
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7. https://doi.org/10.1097/SLA.0b013e318296c732
Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA (2020) The 2019 WHO classification of tumours of the digestive system. Histopathology 76:182–188. https://doi.org/10.1111/his.13975
Quirke P (2003) Training and quality assurance for rectal cancer: 20 years of data is enough. Lancet Oncol 4:695–702. https://doi.org/10.1016/s1470-2045(03)01248-8
Quirke P, Morris E (2007) Reporting colorectal cancer. Histopathology 50:103–112. https://doi.org/10.1111/j.1365-2559.2006.02543.x
Ryan R, Gibbons D, Hyland JMP, Treanor D, White A, Mulcahy HE, O’Donoghue DP, Moriarty M, Fennelly D, Sheahan K (2005) Pathological response following long-course neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Histopathology 47:141–146. https://doi.org/10.1111/j.1365-2559.2005.02176.x
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. https://doi.org/10.1245/s10434-010-0985-4
Porter ME (2010) What is value in health care? N Engl J Med 363:2477–2481. https://doi.org/10.1056/NEJMp1011024
Hall BL, Hirbe M, Waterman B, Boslaugh S, Dunagan WC (2007) Comparison of mortality risk adjustment using a clinical data algorithm (American College of Surgeons National Surgical Quality Improvement Program) and an administrative data algorithm (Solucient) at the case level within a single institution. J Am Coll Surg 205:767–777. https://doi.org/10.1016/j.jamcollsurg.2007.08.013
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Variation in hospital mortality associated with inpatient surgery. N Engl J Med 361:1368–1375. https://doi.org/10.1056/NEJMsa0903048
Ingraham AM, Richards KE, Hall BL, Ko CY (2010) Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg 44:251–267. https://doi.org/10.1016/j.yasu.2010.05.003
Beets G, Sebag-Montefiore D, Andritsch E, Arnold D, Beishon M, Crul M, Dekker JW, Delgado Bolton R, Fléjou JF, Grisold W et al (2017) ECCO essential requirements for quality cancer care: colorectal cancer. a critical review. Crit Rev Oncol Hematol 110:81–93. https://doi.org/10.1016/j.critrevonc.2016.12.001
Acknowledgements
We would like to express our special thanks of gratitude to Dr. Jan Willem Dekker and Professor Rob Tollenaar for inspiring and supporting our team with their experience of the Dutch ColoRectal Audit and Dutch Institute for Clinical Auditing.
Funding
The project was partially funded via financial support from Johnson & Johnson Medical S.p.a Ethicon Division. The funding was provided without restrictions and was utilized for data management and monitoring.
Author information
Authors and Affiliations
Consortia
Contributions
IM, FG, GU,GE, IM, PC, GG, FC, AL, LA, NG, VD, MM, MA, and the ESCA collaborative group contributed to the study design. FG drafted the manuscript, supervised by IM and VD. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The protocol study was approved by the Scientific and Medical Committee of IRST and the Ethics Committee (EC) of each center. The Romagna Ethical Committee (CEROM) approval number is 2278.
Patient informed consent
Informed consent will be obtained from all subjects involved in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Massa, I., Ghignone, F., Ugolini, G. et al. Emilia-Romagna Surgical Colorectal Cancer Audit (ESCA): a value-based healthcare retro-prospective study to measure and improve the quality of surgical care in colorectal cancer. Int J Colorectal Dis 37, 1727–1738 (2022). https://doi.org/10.1007/s00384-022-04203-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04203-w