Abstract
Aim
To compare the number of appendicitis cases and its complications, during the first months of the COVID-19 pandemic in Sweden and the UK and the corresponding time period in 2019.
Method
Reports of emergency abdominopelvic CT performed at 56 Swedish hospitals and 38 British hospitals between April and July 2020 and a corresponding control cohort from 2019 were reviewed. Two radiologists and two surgeons blinded to the date of cohorts analyzed all reports for diagnosis of appendicitis, perforation, and abscess. A random selection of cases was chosen for the measurement of inter-rater agreement.
Result
Both in Sweden (6111) and the UK (5591) fewer, abdominopelvic CT scans were done in 2020 compared to 2019 (6433 and 7223, respectively); p < 0.001. In the UK, the number of appendicitis was 36% lower in April–June 2020 compared to 2019 but not in Sweden. Among the appendicitis cases, there was a higher number of perforations and abscesses in 2020, in Sweden. In the UK, the number of perforations and abscesses were initially lower (April–June 2020) but increased in July 2020. There was a substantial inter-rater agreement for the diagnosis of perforations and abscess formations (K = 0.64 and 0.77).
Conclusion
In Sweden, the number of appendicitis was not different between 2019 and 2020; however, there was an increase of complications. In the UK, there was a significant decrease of cases in 2020. The prevalence of complications was lower initially but increased in July. These findings suggest variability in delay in diagnosis of appendicitis depending on the country and time frame studied.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In 2020, the COVID-19 pandemic had a major impact on many aspects of life worldwide. The pandemic called for novel, unprecedented, and untested measures. The effects of these measures and the unintended consequences of COVID-19 and implemented policies will form the basis for studies for many years in the future even and if normality returns.
In many countries, the pandemic has caused an increasing burden on the healthcare system, which led to down-prioritization and delays in elective diagnoses and surgeries. The effects on emergency care, however, are less well understood. Due to its stochastic nature, the incidence of emergency pathologies should be the least influenced; however, lockdown measures have led to unexpected and unforeseen decreases in emergencies. Furthermore, there is reason to believe that emergencies were not immune to postponements and delays either. Acute appendicitis, a common emergency pathology, should in theory be less impacted than other emergency pathologies such as some forms of trauma (with decreasing incidence due to decreased social interactions during lock-down), or non-COVID chest infections (with decreased incidence due to increased hygiene measures, but increased diagnostics due to being a differential diagnosis to COVID-19 pneumonia), for example.
Multiple studies have been published regarding appendicitis during COVID-19; however, the results have been somewhat conflicting. Delay in diagnosis (on the part of patient/guardian and/or health care) can lead to higher frequency of complications. There is no exact consensus on what constitutes complication in appendicitis. Perforation signs (such as wall-defect, non-regional fibrino-purulent exudate, abscess, and extra intestinal faecal/bowel material are usually considered the most common complications seen at surgery [1]. These signs correspond to defects in mucosal enhancement or wall of appendix, extraintestinal air (local or free), and abscess formation on CT, which we adopted for this study. Most studies have pointed out a decrease in the number of uncomplicated appendicitis but similar number of complicated, suggesting spontaneous resolution of uncomplicated cases. Others have noted the consequent increase in the proportion of complicated cases and in some cases also an increase in the absolute number (prevalence) of complicated cases coupled to a longer prehospital delay [2,3,4,5,6,7].
Normally, appendicitis and its complications require a surgical treatment. Especially during the COVID-19 pandemic, due to many factors, there has been a push to conservative treatment [8], which, in turn, has relied more on an image-based diagnosis. CT (computed tomography) represents the best diagnostic modality in terms of availability and accuracy [9]. The pooled sensitivity and specificity of low-dose CT are 96% and 93%, respectively, while the same figures for standard-dose CT are 96% and 92%, respectively, as reported in a recent meta-analysis [10].
Telemedicine Clinic Ltd. provides out-of-hours emergency teleradiology reporting to a large number of client hospitals in several European countries and has therefore unique access to vast volumes of emergency CT cases. These cases are reported by board-certified, trial-case-selected radiologists with more than 5 years’ experience in emergency radiology.
In this study, the goal was to compare the incidence of appendicitis and its complications (perforation and abscess) in a large cohort of emergency abdominopelvic CT reports obtained in two different European countries during the first months of the COVID-19 pandemic and compare it to the corresponding pre-pandemic period.
Materials and methods
Case selection
All emergency, out-of-hours abdominopelvic CT scans reported by Telemedicine Clinic Ltd. during April to June 2019 and 2020 for the UK and Sweden were collected. Cases were electronically sent to from 56 hospitals in the Sweden and 38 hospitals in the UK. Out-of-hours was defined as 10 pm to 7.30 am local time for Sweden everyday, and 5 pm to 9 am local time for the UK. These hours are based on the needs of the client hospital and their contracts. Additionally, for the UK, data from July 2019 and 2020 were collected. The hospitals are listed in the Supplementary Table.
Cases which were performed out-of-hours but not on an emergency basis were excluded. The initial cohorts consisted of 11,395 and 9975 emergency reports in 2019 and 2020, respectively (Fig. 1).
The reports were filtered for the keyword “app” which narrowed the cohort to a total of 7612 cases. Reports including a history of appendectomy, no mention of appendix or appendicitis in the report, clear unequivocal denial of appendicitis, or description of a normal appendix were excluded by the case selector, author MRT.
Case allocation and reader assessment
A total of 1547 reports were the core of the further analysis. Electronic reports were anonymous and did not show any dates including the date or time of the scanning. The reports were then coded and divided randomly among four senior, board-certified surgeons and radiologists (two each). Each reviewer received 280 unique reports (that only they assessed) in addition to 427 common reports (which were assessed by all readers). The readers were blinded as to which cases are the common or unique ones. The common cases were used for the assessment of agreements.
The readers were asked to score the reports from 1 to 5 regarding the diagnosis of appendicitis, appendiceal perforation, and abscess where 1 was considered definitely negative for diagnosis, 2 probably negative, 3 unclear, 4 probably positive, and 5 definitely positive. For further analysis, scores 4 and 5 were considered positive, while scores 1 and 2 were considered negative, and score 3 was considered unclear.
Measurement of agreement and further analysis of common cases
The reports were divided into three groups according to scores: 1 + 2, 3, and 4 + 5. Fleiss’ Kappa was used for inter-rater agreement levels defined as 0.20 or less as slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 as moderate agreement, 0.61–0.80 as good or substantial agreement, and 0.81 and above as excellent or perfect agreement.
The final score was based on the most scores received if scored the same by three or four readers. In other instances, the reports were presented to a fifth reader, an emergency radiologist (FL) to assign a final score. FL had access to the scores assigned by the four scorers but was blinded to who the reader had been for each score.
Final analyses
The final analyses were done only on reports with probable or definite diagnoses of appendicitis (scores 4 and 5). In these cases, the demographics (age, gender), the prevalence of perforation, and abscess both in terms of proportion (number of complicated cases divided by the number of appendicitis) and the absolute number (prevalence) of complications were compared between 2019 and 2020. The statistical analysis was done for differences between years with X2 when applicable. A p-value of < 0.05 was considered statistically significant.
Ethical aspects
All data regarding patient identification were anonymized prior to extraction, and therefore, ethical approval for the study was not required. There are no individual data in any form. All datasets could be deposited upon request.
Results
Demographics
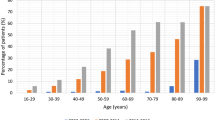
The mean patient age in 2019 was 49.7 (range 3.2–95.9, median 50.3, standard deviation 18.5) and in 2020 was 47.5 (range 2.7–93.8, median 46.7, standard deviation 18.3). Although patients seemed to be slightly younger in 2020, the difference was not statistically significant. In the UK, the youngest ages of patients were 16.3 and 14.0 years old in 2019 and 2020, respectively. In the Sweden, however, children as young as 3.2 and 2.7 had been imaged with CT. Otherwise, no difference could be observed between the countries and the years.
The female/male ratio was 52.5/47.5 in 2019 and 48.5/51.5 in 2019 and 2020, respectively, with no significant difference (p-value = 0.68).
Number of out-of-hours abdominopelvic CT scans with query appendicitis
Fewer out-of-hours abdominopelvic CT scans with query appendicitis were performed in 2020 compared to 2019, in both Sweden (6111 vs 6433, p-value < 0.001) and UK (5591 vs 7223, p-value < 0.001) (Fig. 2).
The final finding of appendicitis according to reporting scores is presented in Table 1.
Inter-rater agreement
The interobserver agreement (Fleiss’ Kappa) level for the presence of perforation and abscess were 0.64 and 0.77, respectively, which were considered a good agreement.
Sweden
The detailed results are shown in Table 2 and Figs. 3 and 4. On average, 91 patients were diagnosed with appendicitis each month in 2020, with the lowest number in April and the highest in June.
In 2020, both the mean proportion of appendicitis patients presenting with perforation and abscess (p values 0.02 and 0.02, respectively) as well as the mean prevalence (absolute number of patients) with perforation and abscess were significantly higher (p-value 0.004 and < 0.001, respectively) compared to 2019 (Fig. 4).
The UK
The detailed results are shown in Table 2 and Figs. 5 and 6. On average, 65 patients were diagnosed with appendicitis each month in 2020, with the lowest figure in April and the largest in July.
Unlike Sweden, when compared with 2019, the number of CT-diagnosed cases of appendicitis diagnoses in 2020 was lower in the UK (p < 0.001).
In 2020, both the mean proportion of appendicitis patients presenting with perforation and abscess (p values 0.02 and < 0.001, respectively) as well as the mean prevalence (absolute number of patients) with perforation and abscess were significantly different (p-value 0.007 and < 0.001, respectively) compared to 2019 (Fig. 6). However, unlike Sweden, these figures were initially lower but increased in July.
Discussion
This observational study demonstrates some similarities and differences between the UK and Swedish patterns in the number of diagnosed cases of appendicitis and its complications. In both countries, the COVID-19 outbreak started in January 2020, and in the present study, we can detect a much lower number of performed acute CT of the abdomen in April 2020 than the corresponding month in 2019. In the Sweden, there was an increase in the number and proportion of patients diagnosed with complicated CT-verified appendicitis (perforation/abscess) in May and June 2020 compared to April 2020.
In the UK, the results were not homogenous during the observation period. The decrease in number of abdominopelvic CTs persisted until July. Initially, both the number of cases with appendicitis and complications decreased and this trend continued for several months. The proportion of cases with complications were also initially lower in 2020; however, the number and proportion of patients with abscesses were dramatically increased in July 2020.
Our study illustrates some findings not previously shown. One is that figures and patterns from different countries might be different. This could well be due to public measures and is beyond the scope of this article. Another important point is the temporal course of complications. Especially looking at the data from the UK, one might get different results if different time intervals are chosen for the observation.
Several studies have published results showing an increased proportion of complicated cases in the COVID-era [2,3,4, 8,9,10]. However, some studies have found only reductions of uncomplicated cases [5, 11,12,13,14,15,16] or no change [17]. Several of these latter studies are registration studies having the advantage of having more data from more centres. They are prone to problems with registration studies however. It is conceivable that investigator/physician-initiated studies such as our own might be triggered by observed clinical trends. Our study has some points of strength not seen in prior studies. It is the largest study on actual cases and not registries. It is also the only study encompassing two countries and many hospitals. Additionally, our study is probably the only study where the date of examinations was blinded, thus less likely to bias.
The results of our study are based on CT exams. CT is more accurate than any presurgical examination or test for diagnosis of appendicitis and detection of its complications. Although CT results are probably not as perfect as surgical exploration, surgical explorations are not always offered to all patients especially during COVID [18]. One caveat is that CT, similar to surgery, is not performed on every patient. In order to decrease this confounding factor, we chose to compare the same hospitals and countries during 2019 and 2020. We had access to other countries that were not the same in 2019 and 2020 and decided not include them. We cannot rule out that a higher percentage of patients suspected of appendicitis underwent CT during 2020 [19]. The use of teleradiology CT activity has been shown to correlate with COVID-19 epidemiology [20]. CT however provides another advantage not seen with surgery, i.e., the dates can be blinded and thus avoid some bias.
There are multiple reports of delay in diagnosis and treatment of patients with chronic diseases, including cancer [21, 22]. The increased mortality and morbidity from delay in diagnosis and treatment may only emerge at a later stage [23,24,25]. Ostensibly, emergency health care should be more dependant on the individual patient’s health and choice rather than on the pandemic. Evidence points out similar trends elsewhere. For instance, fewer acute coronary presentations but a higher proportion of severe cases [26].
Full and severe lockdown measures have not been associated with lower COVID-19 mortality [27]. One of the interesting aspects concerning Sweden was its rather different approach to lockdowns. The Swedish approach was somewhat different from many other countries. It relied more on the informed consent of its citizens rather than the use of coercion and mandates. It, therefore, implemented milder forms of lockdowns, in the hope that the population would show more compliance with healthcare measures in the long term. The UK adopted a similar approach initially but soon changed course. As with other observational studies, it is difficult, if not impossible, to evaluate causal relationships [28]. Although lockdowns should not in theory lead to fewer people being able to seek emergency health care, i.e., system delay (although some data as well anecdotal evidence suggest otherwise [16]), it may have led to increased anxiety and fear among patients [29] which in turn might have impacted patients seeking medical attention in time (patient delay).
Our study also demonstrates a different trend in appendicitis and its complications between the UK and Sweden. It is conceivable that in both countries patients with appendicitis sought medical attention later in 2020 than in 2019. However, the degree of delay was more pronounced in the UK. It could be that in the Sweden delays were in the order of hours and days, and thus, the rise of complication rate was evident early. In the UK, we suspect that patients were imaged much later, perhaps weeks later. This led to a significant drop in the number of diagnosed cases first, but as time progressed the complicated cases started coming in. Whatever the reason for such different patterns, it should be a reminder of the importance of timing of an observation.
Interestingly, the pattern in April 2020 is similar to 2019 in the UK. This might have been due to UK being hit by COVID-19 later than Sweden leading to initially very few diagnosed, largely uncomplicated cases.
Our observational study has some limitations; some of which have been addressed briefly above. One is that our studied period does not encompass the whole 24 h period. We were unable to retrieve data during normal working hours and therefore unable to include them. To mitigate this issue, we did study the same hours of operation in 2019 and 2020, but a potential bias can still remain. Another issue is reliance on CT and its reports. We did not have access to data from patients who did not have CT (i.e., who underwent ultrasound only or went directly to surgery). This coupled with reliance on CT reports—albeit blinded to date of exam—can create other potential biases.
Conclusion
In both countries, there was an increasing number and proportion of complications toward the end of the observation period; however, there was variation between observed time period and countries.
Abbreviations
- COVID-19:
-
2019 Novel coronavirus
- CT:
-
Computerized tomography
References
Cameron DB, Anandalwar SP, Graham DA, Melvin P, Serres SK, Dunlap JL, Kashtan M, Hall M, Saito JM, Barnhart DC, Kenney BD, Rangel SJ (2020) Development and implications of an evidence-based and public health-relevant definition of complicated appendicitis in children. Ann Surg 271(5):962–968
Scheijmans JCG, Borgstein ABJ, Puylaert CAJ, Bom WJ, Bachiri S, van Bodegraven EA, Brandsma ATA, Ter Brugge FM, de Castro SMM, Couvreur R, Franken LC, Gaspersz MP, de Graaff MR, Groenen H, Kleipool SC, Kuypers TJL, Martens MH, Mens DM, Orsini RG, Reneerkens NJMM, Schok T, Sedee WJA, Tavakoli Rad S, Volders JH, Weeder PD, Prins JM, Gietema HA, Stoker J, Gisbertz SS, Besselink MGH, Boermeester MA, SCOUT Collaboarative Study group (2021) Impact of the COVID-19 pandemic on incidence and severity of acute appendicitis: a comparison between 2019 and 2020. BMC Emerg Med 21(1):61. https://doi.org/10.1186/s12873-021-00454-y. PMID: 33980150; PMCID: PMC8114672
Schäfer FM, Meyer J, Kellnar S, Warmbrunn J, Schuster T, Simon S, Meyer T, Platzer J, Hubertus J, Seitz ST, Knorr C, Stehr M (2021) Increased incidence of perforated appendicitis in children during COVID-19 pandemic in a Bavarian multi-center study. Front Pediatr 7(9):683607. https://doi.org/10.3389/fped.2021.683607. PMID: 34026695; PMCID: PMC8138624
Lisi G, Campanelli M, Mastrangeli MR, Grande S, Viarengo MA, Garbarino GM, Vanni G, Grande M (2021) Acute appendicitis in elderly during COVID-19 pandemic. Int J Colorectal Dis 1–4. https://doi.org/10.1007/s00384-021-03959-x. Epub ahead of print. PMID: 34046696; PMCID: PMC8159028
Ceresoli M, Coccolini F, Magnone S, Lucianetti A, Bisagni P, Armao T, Ansaloni L, Zago M, Chiarugi M, Catena F, Braga M, Appendicitis-COVID study group (2021) The decrease of non-complicated acute appendicitis and the negative appendectomy rate during pandemic. Eur J Trauma Emerg Surg 1–7. https://doi.org/10.1007/s00068-021-01663-7. Epub ahead of print. PMID: 33844036; PMCID: PMC8040760
Aharoni M, Barash Y, Zager Y, Anteby R, Khalilieh S, Amiel I, Klang E, Goldes Y, Gutman M, Horesh N, Rosin D (2021) Management of acute appendicitis during the COVID-19 pandemic: a single tertiary center experience. Isr Med Assoc J 23(5):269–273. PMID: 34024041
Chang YJ, Chen LJ, Chang YJ (2022) Did the severity of appendicitis increase during the COVID-19 pandemic? PLoS ONE 17(2):e0263814. https://doi.org/10.1371/journal.pone.0263814. PMID: 35143582; PMCID: PMC8830628
Angeramo CA, Dreifuss NH, Schlottmann F, Rotholtz NA (2021) More severe presentations of acute appendicitis during COVID-19. J Gastrointest Surg 25(7):1902–1904. https://doi.org/10.1007/s11605-020-04892-0. Epub 2021 Jan 19. PMID: 33469887; PMCID: PMC7815199
Antakia R, Xanthis A, Georgiades F, Hudson V, Ashcroft J, Rooney S, Singh AA, O'Neill JR, Fearnhead N, Hardwick RH, Davies RJ, Bennett JMH (2021) Acute appendicitis management during the COVID-19 pandemic: a prospective cohort study from a large UK centre. Int J Surg 86:32–37. https://doi.org/10.1016/j.ijsu.2020.12.009. Epub 2021 Jan 16. PMID: 33465496; PMCID: PMC7985094
Bowen JM, Sheen JRC, Whitmore H, Wright C, Bowling K (2021) Acute appendicitis in the COVID-19 era: a complicated situation? Ann Med Surg (Lond) 67:102536. https://doi.org/10.1016/j.amsu.2021.102536. Epub 2021 Jul 2. PMID: 34230852; PMCID: PMC8252704
Hayatghaibi SE, Trout AT, Dillman JR, Callahan M, Iyer R, Nguyen H, Riedesel E, Ayyala RS (2021) Trends in pediatric appendicitis and imaging strategies during COVID-19 in the United States. Acad Radiol S1076–6332(21)00363–9. https://doi.org/10.1016/j.acra.2021.08.009. Epub ahead of print. PMID: 34493456; PMCID: PMC8390378
Köhler F, Acar L, van den Berg A, Flemming S, Kastner C, Müller S, Diers J, Germer CT, Lock JF, L'hoest H, Marschall U, Wiegering A (2021) Impact of the COVID-19 pandemic on appendicitis treatment in Germany-a population-based analysis. Langenbecks Arch Surg 406(2):377–383. https://doi.org/10.1007/s00423-021-02081-4. Epub 2021 Jan 9. PMID: 33420517; PMCID: PMC7794073
La Pergola E, Sgrò A, Rebosio F, Vavassori D, Fava G, Codrich D, Montanaro B, Leva E, Schleef J, Cheli M, Pelizzo G, Gamba P, Alberti D, Betalli P (2020) Appendicitis in children in a large Italian COVID-19 pandemic area. Front Pediatr 9(8):600320. https://doi.org/10.3389/fped.2020.600320. PMID: 33363065; PMCID: PMC7755995
Neufeld MY, Bauerle W, Eriksson E, Azar FK, Evans HL, Johnson M, Lawless RA, Lottenberg L, Sanchez SE, Simianu VV, Thomas CS, Drake FT (2021) Where did the patients go? Changes in acute appendicitis presentation and severity of illness during the coronavirus disease 2019 pandemic: a retrospective cohort study. Surgery 169(4):808–815. https://doi.org/10.1016/j.surg.2020.10.035. Epub 2020 Dec 4. PMID: 33288212; PMCID: PMC7717883
Theodorou CM, Beres AL, Nguyen M, Castle SL, Faltermeier C, Shekherdimian S, Tung C, DeUgarte DA, Brown EG (2021) Statewide impact of the COVID pandemic on pediatric appendicitis in California: a multicenter study. J Surg Res 267:132–142. https://doi.org/10.1016/j.jss.2021.05.023. Epub ahead of print. PMID: 34147003
Willms AG, Oldhafer KJ, Conze S, Thasler WE, von Schassen C, Hauer T, Huber T, Germer CT, Günster S, Bulian DR, Hirche Z, Filser J, Stavrou GA, Reichert M, Malkomes P, Seyfried S, Ludwig T, Hillebrecht HC, Pantelis D, Brunner S, Rost W, Lock JF, CAMIN Study Group (2021) Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch Surg 406(2):367–375. https://doi.org/10.1007/s00423-021-02090-3. Epub 2021 Feb 7. PMID: 33550453; PMCID: PMC7867500
Sano K, Nakamura M, Ninomiya H, Kobayashi Y, Miyawaki A (2021) Large decrease in paediatric hospitalisations during the COVID-19 outbreak in Japan. BMJ Paediatr Open 5(1):e001013. https://doi.org/10.1136/bmjpo-2020-001013. PMID: 34192195; PMCID: PMC7956728
Lotfallah A, Aamery A, Moussa G, Manu M (2021) Surgical versus conservative management of acute appendicitis during the COVID-19 pandemic: a single-centre retrospective study. Cureus 13(3):e14095. https://doi.org/10.7759/cureus.14095. PMID: 33927917; PMCID: PMC8075754
Ielpo B, Podda M, Pellino G, Pata F, Caruso R, Gravante G, Di Saverio S, ACIE Appy Study Collaborative (2020) Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Appy Study. Br J Surg. https://doi.org/10.1002/bjs.11999. Epub ahead of print. PMID: 33030744; PMCID: PMC7675377
Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM (2017) Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol 208(6):W198–W207. https://doi.org/10.2214/AJR.16.17274. Epub 2017 Mar 16 PMID: 28301209
Crombé A, Lecomte JC, Banaste N, Tazarourte K, Seux M, Nivet H, Thomson V, Gorincour G (2021) Emergency teleradiological activity is an epidemiological estimator and predictor of the COVID-19 pandemic in mainland France. Insights Imaging 12(1):103. https://doi.org/10.1186/s13244-021-01040-3. PMID: 34292414; PMCID: PMC8295630
Decker KM, Lambert P, Feely A, Bucher O, Kim JO, Hebbard P, Thiessen M, Fatoye T, Pitz M, Koul R, Czaykowski P (2021) Evaluating the impact of the COVID-19 pandemic on new cancer diagnoses and oncology care in Manitoba. Curr Oncol 28(4):3081–3090. https://doi.org/10.3390/curroncol28040269. PMID: 34436035
Jazieh AR, Akbulut H, Curigliano G, Rogado A, Alsharm AA, Razis ED, Mula-Hussain L, Errihani H, Khattak A, De Guzman RB, Mathias C, Alkaiyat MOF, Jradi H, Rolfo C, International Research Network on COVID-19 Impact on Cancer Care (2020) Impact of the COVID-19 pandemic on cancer care: a global collaborative study. JCO Glob Oncol 6:1428–1438. https://doi.org/10.1200/GO.20.00351. PMID: 32986516; PMCID: PMC7529504
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC (2020) Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on imaging case volumes. J Am Coll Radiol 17(7):865–872. https://doi.org/10.1016/j.jacr.2020.05.004. Epub 2020 May 16. PMID: 32425710; PMCID: PMC7229978
Alagoz O, Lowry KP, Kurian AW, Mandelblatt JS, Ergun MA, Huang H, Lee SJ, Schechter CB, Tosteson ANA, Miglioretti DL, Trentham-Dietz A, Nyante SJ, Kerlikowske K, Sprague BL, Stout NK (2021) Impact of the COVID-19 pandemic on breast cancer mortality in the US: estimates from collaborative simulation modeling. J Natl Cancer Inst djab097. https://doi.org/10.1093/jnci/djab097. Epub ahead of print. PMID: 34258611; PMCID: PMC8344930
Sutherland N, Dayawansa NH, Filipopoulos B, Vasanthakumar S, Narayan O, Ponnuthurai FA, van Gaal W (2021) Acute coronary syndrome in the COVID-19 pandemic: reduced cases and increased ischaemic time. Heart Lung Circ S1443–9506(21)01194-X. https://doi.org/10.1016/j.hlc.2021.07.023. Epub ahead of print. PMID: 34452843
Chaudhry R, Dranitsaris G, Mubashir T, Bartoszko J, Riazi S (2020) A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine 25:100464. https://doi.org/10.1016/j.eclinm.2020.100464. Epub 2020 Jul 21. PMID: 32838237; PMCID: PMC7372278
Boyko EJ (2013) Observational research--opportunities and limitations. J Diabetes Complications 27(6):642–8. https://doi.org/10.1016/j.jdiacomp.2013.07.007. Epub 2013 Sep 19. PMID: 24055326; PMCID: PMC3818421
Laufer A, Bitton-Shechory M (2021) Gender differences in the reaction to COVID-19. Women Health 1–11. https://doi.org/10.1080/03630242.2021.1970083. Epub ahead of print. PMID: 34445941
Acknowledgements
The authors would like to thank Ms. Ida Anderman PMO of Telemedicine Clinic and IT staff at Telemedicine Clinic for providing us with primary data for further analysis.
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
MRT: design of the study and collection, analysis, and interpretation of data and in writing the manuscript. AT: design of the study, analysis, and interpretation of data and in writing the manuscript. AC: design of the study, analysis, and interpretation of data and in writing the manuscript. MN: design of the study, analysis, and interpretation of data and in writing the manuscript. REA: design of the study, and interpretation of data and in writing the manuscript. FL: design of the study, analysis, and interpretation of data and in writing the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests/Conflict of interests
The authors declare no competing interests. The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• During the first months of COVID-19, rates of appendicitis and complications changed. In Sweden, the observed complication rate was however higher. In the United Kingdom, the number of appendicitis cases decreased significantly. The complication rate in the UK was variable during the observation period.
• Presumed COVID-19 impacts on appendicitis and its complications are variable and this might explain the variability in some published studies.
Rights and permissions
About this article
Cite this article
Torkzad, M.R., Thorisson, A., Chabok, A. et al. Impact of COVID-19 on the incidence of CT-diagnosed appendicitis and its complications in the UK and Sweden. Int J Colorectal Dis 37, 1375–1383 (2022). https://doi.org/10.1007/s00384-022-04181-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04181-z