Abstract
Objective
To assess the patterns of hospitalizations among early-stage colon cancer patients receiving adjuvant chemotherapy and to identify high-risk groups that may benefit from more careful monitoring in a real-world, population-based context.
Methods
This is a population-based study using linked administrative databases from the province of Alberta, Canada. Any events of hospitalization among patients with non-metastatic colon cancer undergoing upfront surgery followed by adjuvant chemotherapy were reviewed. Multivariable logistic regression analysis was used to examine factors associated with risk of hospitalization, and the impact of hospitalization on overall survival was assessed through Kaplan–Meier estimates and Multivariable Cox regression analysis.
Results
A total of 2257 patients were considered eligible and were included in the current analysis, including 483 patients (21.4%) who were hospitalized within 6 months of the start of adjuvant chemotherapy, and 1774 patients (78.6%) who were not. The following factors were associated with a higher hospitalization risk: older age (OR: 1.02; 95% CI 1.01–1.03), higher comorbidity (OR: 1.48; 95% CI 1.31–1.67), women (OR for men versus women: 0.79; 95% CI 0.64–0.98), living in the North zone (OR for Edmonton zone versus North zone: 0.60; 95% CI 0.42–0.87), and CAPOX chemotherapy (OR for CAPOX versus FOLFOX: 1.50; 95% CI 1.12–2.00). Patients with a history of hospitalization during adjuvant chemotherapy had a worse overall survival compared to patients who were not hospitalized (P < 0.001).
Conclusion
In this study, one out of five colon cancer patients were hospitalized during adjuvant chemotherapy. Older individuals, women, those with higher comorbidity, and those receiving adjuvant CAPOX were more likely to be hospitalized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is one of the main causes of mortality and morbidity in Canada and the world [1,2,3,4]. While surgery plays the most important role in the management of non-metastatic disease, (neo)adjuvant treatment has been shown to improve oncological outcomes [5,6,7].
Although many real-world studies have evaluated the attrition, and outcomes of adjuvant chemotherapy in the setting of early-stage disease, assessment of serious side effects has been dependent on results from randomized controlled trials [8,9,10,11]. There is a well-known discordance between toxicities reported in randomized controlled trials versus those reported in population-based studies, with population-based studies more likely to report a higher incidence of side effects (because of generally older patient population and higher comorbidity) [12].
Population-based cancer registries are unable to track and record chemotherapy-induced toxicities accurately; therefore, we utilized events of hospitalization during chemotherapy as a surrogate indicator for the occurrence of serious adverse events. There is a paucity of data regarding hospitalizations during adjuvant therapy for colon cancer in a universal health care model in the real-world setting. Alberta is one of the largest Canadian provinces with a provincial single over-arching healthcare system (Alberta Health Services). We interrogated administrated datasets from this publicly funded, centralized healthcare system to evaluate real-world events of hospitalizations, including their reasons and timing, in relation to receipt of adjuvant chemotherapy.
The current study thus aims to assess the patterns of hospitalizations among early-stage colon cancer patients receiving adjuvant chemotherapy, and to identify high-risk groups that may benefit from more careful monitoring in a real-world, population-based context.
Methods
Data sources
This is a retrospective, population-based study based on linked administrative databases from the province of Alberta, Canada. Cancer care in Alberta is publicly funded and centrally managed through a provincial body “Cancer Care Alberta.” Selected demographic and clinicopathological information for all cancer patients in the province is reported to the Alberta Cancer Registry, cancer treatments are reported through the provincial electronic medical records, and hospital admissions are captured through the National Ambulatory Care Reporting System (NACRS), a national program with which Alberta is a collaborating partner. This study links information from all the above sources. Study datasets were extracted through Surveillance and Reporting team within Cancer Care Alberta and then delivered to the authors [13]. The authors did not do any chart reviews as part of this study. This study was approved by Health Research Ethics Board of Alberta (HREBA.CC-20–0215).
Selection criteria for patients included in the current analysis are (1) diagnosis with non-metastatic colon adenocarcinoma, (2) upfront treatment with radical surgery (only those surgeries with lymph node assessments were considered to avoid inadvertent inclusion of patients undergoing palliative surgeries), and (3) adjuvant chemotherapy with one of the following adjuvant chemotherapy regimens (Capecitabine, 5FU/FA (5-fluorouracil and folinic acid), FOLFOX (infusional 5-fluorouracil, leucovorin and oxaliplatin), CAPOX (capecitabine and oxaliplatin), FLOX (5-fluorouracil, leucovorin and oxaliplatin)) started within 4 months of surgery. Patients with rectal primaries were not included, and patients who received postoperative radiotherapy (in addition to chemotherapy) were not included; this was done to limit the confounding effect of radiotherapy toxicity on the rates of hospitalization. In cases of two primary colon cancers, only the first diagnosed tumor was included (regardless of the time of the diagnosis of the subsequent cancer).
From a healthcare perspective, Alberta is divided into five health zones (North zone, Edmonton zone, Central zone, Calgary zone, and South zone). North zone has the lowest population/landmass ratio with limited access to tertiary healthcare facilities. Further demographic and health service differences between the five zones were provided elsewhere. The two main urban centers in Alberta are Edmonton and Calgary where the majority of tertiary healthcare centers are located.
Data collection
The following data were included (where available): age at diagnosis, sex, stage, primary site/side, Charlson comorbidity index, zone of residence, and adjuvant chemotherapy regimen. Hospital admissions (starting from the date of start of adjuvant chemotherapy until 6 months after chemotherapy receipt) were reviewed, including number, date, and admission diagnoses. Admission diagnoses were reported per the ICD coding system, and it is possible for patients to have more than one admission diagnosis. As this study utilized databases without chart reviews, we were not able to ascertain details regarding treatment discontinuation.
Statistical analysis
Descriptive statistics were initially used to examine the differences between individuals with or without any episode of hospitalizations through chi-squared testing for categorical variables and independent t-test for continuous variables. Further descriptive analyses were conducted for the following three admission diagnoses: infection: identified by ICD codes of A00-B99; digestive toxicities: identified by ICD codes of K00-K93; and circulatory disorders: identified by ICD codes of I00-I99. It has to be noted that many patients have more than one admission diagnosis (i.e., they are not mutually exclusive). Multivariable logistic regression analysis was then used to examine the association between some demographic and clinical variables and hospitalization risk. The following variables were included in this model: age, sex, side of primary, adjuvant chemotherapy regimen, Charlson comorbidity index, stage, and zone of residence.
In order to examine the impact of hospitalization on overall survival, Kaplan–Meier survival estimates and log-rank testing were used to compare overall survival between individuals who have any hospital admission versus those who have none while receiving adjuvant chemotherapy. Moreover, multivariable Cox regression analysis was conducted, and the model included age, sex, side of primary, type of adjuvant chemotherapy, Charlson comorbidity index, stage, hospitalization, and zone of residence. All analyses were conducted through SPSS statistical software (version 26.0, IBM, NY).
Results
Patients’ characteristics
Figure 1 provides an algorithm for the study selection process of included patients. A total of 2257 patients were considered eligible and were included in the current analysis, including 483 patients (21.4%) who were hospitalized within 6 months of the start of adjuvant chemotherapy and 1774 patients (78.6%) who were not. Comparing both groups together, patients who were hospitalized were likely to be older (P < 0.001), had a higher comorbidity (P < 0.001), lived in the North zone (P = 0.021), and received adjuvant CAPOX (P = 0.036) (Table 1). Percentage of patients on different regimens who were hospitalized (out of the total number of patients receiving this specific regimen) was as follows: FOLFOX: 18.9%; CAPOX: 24.8%; Capecitabine: 22%; 5FU/FA: 21.3%; FLOX: 0%. A total of 136 patients (6%) had an infection as one of their admission diagnoses, 272 patients (12.1%) had one of the digestive toxicities as one of their admission diagnoses, and 204 patients (9%) had circulatory disorders as one of their admission diagnoses. Figure 2 provides the distribution of the three admission diagnoses according to sex, sidedness, and adjuvant chemotherapy regimen. Women were more likely than men to experience infection as an admission diagnosis (P = 0.007), right-sided tumors were more likely than left-sided tumors to experience infection as an admission diagnosis (P = 0.041), and patients receiving CAPOX or capecitabine as an adjuvant treatment were more likely to experience digestive toxicities as one of the admission diagnoses (P < 0.001).
Association between hospitalization risk and demographic/treatment characteristics
The following factors were associated with a higher hospitalization risk: older age (OR 1.02; 95% CI 1.01–1.03), higher comorbidity (OR 1.48; 95% CI 1.31–1.67), women (OR for men versus women 0.79; 95% CI 0.64–0.98), living in the North zone (OR for Edmonton zone versus North zone 0.60; 95% CI 0.42–0.87), CAPOX chemotherapy (OR for CAPOX versus FOLFOX 1.50; 95% CI 1.12–2.00) (Table 2).
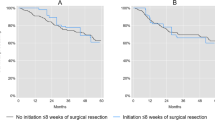
Impact of hospitalization on overall survival
Using Kaplan–Meier estimates, patients with a history of hospitalization during adjuvant chemotherapy had worse overall survival compared to patients who were not admitted to hospital (P < 0.001) (Fig. 3). Within a multivariable Cox regression analysis, history of hospitalization was also associated with worse overall survival (HR for no hospitalization versus hospitalization 0.70; 95% CI 0.58–0.85). Other factors associated with worse overall survival include older age (HR 1.02; 95% CI 1.01–1.03), men (HR 1.22; 95%CI 1.03–1.45), higher comorbidity (HR 1.14; 95% CI 1.04–1.24), higher stage (HR for stage II versus stage III 0.57; 95% CI 0.44–0.76), and proximal side of the primary (HR for distal versus proximal side : 0.74; 95% CI 0.62–0.89) (Table 3).
Discussion
The current study evaluates patterns of hospitalizations among patients with non-metastatic colon cancer within 6 months of starting adjuvant chemotherapy. It showed that within this study cohort, one out of five colon cancer patients were hospitalized during adjuvant chemotherapy. Older individuals, women, those with higher comorbidity, those living in the North zone (i.e. less urban areas), and those receiving adjuvant CAPOX are more likely to be hospitalized. This data can be relevant when counseling patients about the real-world risks associated with adjuvant chemotherapy in the setting of colon cancer.
Association of older age with higher hospitalization risk is in line with many prior studies (both randomized and population-based) highlighting the heightened toxicity risks associated with chemotherapy in older individuals [14, 15]. Although biological age (rather than chronological age) is the standard assessment tool for chemotherapy eligibility, elderly individuals are likely to have more comorbid conditions, and therefore, higher risks of side effects from chemotherapy. Likewise, prior studies have described sex-based differences in chemotherapy side effects in the setting of gastrointestinal cancers, with women having higher risks of hematologic and gastrointestinal side effects [16, 17]. Results from the current study are consistent with the findings from these other studies and suggests that further work on gender-based tailoring of treatment is warranted; this may require chemotherapy dosing based on lean body mass. In the interim, clinicians may choose to monitor women and older patients more closely for treatment-related toxicities. On the other hand, higher hospitalization risks among individuals living in the North zone can potentially be explained by limited access to specialist care in this area of the province. This could have led to patients presenting to emergency departments to discuss their health concerns instead of contacting their primary care providers and/or their specialist physicians.
Adjuvant CAPOX seems to be associated with a higher risk of hospitalizations compared to adjuvant FOLFOX. This is shown in the current study to be driven by a higher risk of digestive toxicities (likely driven by the capecitabine component of the regimen as capecitabine was also associated with a higher risk of digestive toxicities). It should be noted that most of the patients in the current study were treated before 2018 (i.e., before the publication of the IDEA trial results). Thus, it is not known if 3 months of CAPOX (the currently favored regimen for low-risk stage III patients) will be associated with the same higher risks of hospitalizations as the 6-month regimen. Nevertheless, this study suggests that if a 6-month regimen is indicated, FOLFOX has a lower risk of hospitalization, which should be considered when counselling patients. Electronic patient self-reporting of adverse events compared to usual care has not yet been shown to reduce hospitalizations for patients on adjuvant chemotherapy, but this is an area that should continue to be investigated [18]. Although the current study was in the pre-COVID-19 era, one important topic for health services research in the future is the potential impact of increasing use of virtual care in oncology practices on the risk of serious adverse events and subsequent hospitalizations among cancer patients receiving systemic therapy [19].
Prior studies have shown that a number of factors are linked to higher toxicity of adjuvant chemotherapy of colon cancer. These include decreased muscle mass, and Caucasian ethnicity (compared to African American ethnicity). Given the way the Alberta Cancer registry is organized and coded, these two factors could not be evaluated in the current study [20, 21].
Ten patients with stage I colon cancer were reported to have received adjuvant chemotherapy in the current dataset. This is not consistent with the current treatment guidelines for colon cancer in Alberta or elsewhere [22]. It is unclear if there were specific risk features and/or stage uncertainty for those individuals that required the use of adjuvant chemotherapy.
Hospitalizations during adjuvant chemotherapy have been shown to predict worse overall survival among included patients. There are a number of factors which may have contributed to this excess mortality, including the direct and/or indirect impact of toxicities, underlying hospitalizations, the fact that hospitalized patients are likely to have other adverse prognostic features (e.g., older age and higher comorbidity), possible dose reduction/treatment interruptions resulting from treatment-related hospitalizations, inability to administer effective salvage chemotherapy at the time of relapse (because of prior severe side effects experienced during adjuvant chemotherapy), or possibly to a combination of the above factors. Men were also shown to have worse overall survival compared to women in the current study. Prior studies have suggested that this difference is related to a possibly higher comorbidity burden among men versus women rather than to a particularly aggressive disease biology among men versus women [23]. This also adds to the body of literature highlighting gender-based differences in gastrointestinal cancer.
Some limitations of the current study need to be considered. First, hospitalizations in the current study were used as a surrogate indicator of treatment -emergent toxicities. However, it is possible that some of these hospitalizations were for non-treatment-related reasons (this is something that cannot be differentiated without a dedicated chart review which has not been done in the current study). It is possible also that hospitalization rates are affected by other non-medical issues (e.g., zone of residence and access to timely primary care). Second, some patients with significant toxicities might have presented with toxicities to their family physicians, oncologists, or other healthcare providers in a non-hospital setting. These events would not be captured in the current study unless they are associated with subsequent hospitalizations (which is not necessarily the case for every patient). Third, the evaluated datasets are only related to provincial administrative databases in Alberta. Thus, if a patient did have a treatment-related hospitalization in another jurisdiction (while they are receiving chemotherapy in an Alberta cancer center), this information will not have been captured in the current study. Fourth, despite our best efforts, there is a still a possibility of miscoded information in any of the accessed databases (and such miscoding can only be detected with a chart review which was not done in the current study). These limitations need to be weighed against the strengths of the current study, including the reliance on administrative datasets from a single-payer healthcare system where all patient encounters within this system are expected to be captured.
In conclusion, this study demonstrated that adjuvant chemotherapy for colon cancer can be associated with significant toxicities, with one in five patients requiring hospitalization. Individuals with older age, women, those with higher comorbidity, those living in the North zone (with potentially limited access to specialist care), and those receiving adjuvant CAPOX were more likely to be hospitalized. These risks should be taken into consideration when discussing adjuvant chemotherapy options with patients.
References
Kasi PM, Shahjehan F, Cochuyt JJ, Li Z, Colibaseanu DT, Merchea A (2019) Rising proportion of young individuals with rectal and colon cancer. Clin Colorectal Cancer 18(1):e87–e95
Doubeni CA (2019) Early-onset colorectal cancer: what reported statistics can and cannot tell us and their implications. Cancer 125(21):3706–3708
Abualkhair WH, Zhou M, Ahnen D, Yu Q, Wu XC, Karlitz JJ (2020) Trends in incidence of early-onset colorectal cancer in the United States among those approaching screening age. JAMA Netw Open 3(1):e1920407
Helsingen LM, Vandvik PO, Jodal HC, Agoritsas T, Lytvyn L, Anderson JC et al (2019) Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: a clinical practice guideline. BMJ 367:l5515
Virostko J, Capasso A, Yankeelov TE, Goodgame B (2019) Recent trends in the age at diagnosis of colorectal cancer in the US National Cancer Data Base, 2004–2015. Cancer 125(21):3828–3835
Mannucci A, Zuppardo RA, Rosati R, Leo MD, Perea J, Cavestro GM (2019) Colorectal cancer screening from 45 years of age: thesis, antithesis and synthesis. World J Gastroenterol 25(21):2565–2580
O’Sullivan DE, Hilsden RJ, Ruan Y, Forbes N, Heitman SJ, Brenner DR (2020) The incidence of young-onset colorectal cancer in Canada continues to increase. Cancer Epidemiol 69:101828
Abdel-Rahman O (2019) Outcomes of non-metastatic colon cancer patients in relationship to socioeconomic status: an analysis of SEER census tract-level socioeconomic database. Int J Clin Oncol 24(12):1582–1587
Giryes A, Oweira H, Mannhart M, Abdel-Rahman O (2018) Impact of primary tumor side on the outcomes of patients with non-metastatic colon cancer: a patient-level pooled analysis of two clinical trials. Expert Rev Gastroenterol Hepatol 12(8):843–848
Batra A, Rigo R, Sheka D, Cheung WY (2020) Real-world evidence on adjuvant chemotherapy in older adults with stage II/III colon cancer. World J Gastrointest Oncol 12(6):604–618
Batra A, Kong S, Cheung WY (2020) Eligibility of real-world patients with stage II and III colon cancer for adjuvant chemotherapy trials. Clin Colorectal Cancer 19(4):e226–e234
Andersson Y, Bergkvist L, Frisell J, de Boniface J (2019) Do clinical trials truly mirror their target population? an external validity analysis of national register versus trial data from the Swedish prospective SENOMIC trial on sentinel node micrometastases in breast cancer. Breast Cancer Res Treat 177(2):469–475
Surveillance & Reporting (2020) Alberta cancer registry/electronic medical records. cancer research & analytics, cancer care Alberta, Alberta health services
Abdel-Rahman O, Karachiwala H (2019) Impact of age on toxicity and efficacy of 5-FU-based combination chemotherapy among patients with metastatic colorectal cancer; a pooled analysis of five randomized trials. Int J Colorectal Dis 34(10):1741–1747
Abdel-Rahman O, Ahmed O (2019) Predictors of toxicity-related hospitalization in four randomized studies of 5-fluorouracil-based chemotherapy in metastatic colorectal cancer. Int J Colorectal Dis 34(4):675–680
Abdel-Rahman O (2019) Impact of sex on chemotherapy toxicity and efficacy among patients with metastatic colorectal cancer: pooled analysis of 5 randomized trials. Clin Colorectal Cancer 18(2):110–5.e2
Özdemir BC, Csajka C, Dotto GP, Wagner AD (2018) Sex differences in efficacy and toxicity of systemic treatments: an undervalued issue in the era of precision oncology. J Clin Oncol 36(26):2680–2683
Absolom K, Warrington L, Hudson E, Hewison J, Morris C, Holch P et al (2021) Phase III randomized controlled trial of eRAPID: eHealth intervention during chemotherapy. J Clin Oncol 39(7):734–747
Abdel-Rahman O (2021) Patient-related barriers to some virtual healthcare services among cancer patients in the USA: a population-based study. J Comp Eff Res 10(2):119–126
Jung HW, Kim JW, Kim JY, Kim SW, Yang HK, Lee JW et al (2015) Effect of muscle mass on toxicity and survival in patients with colon cancer undergoing adjuvant chemotherapy. Support Care Cancer 23(3):687–694
McCollum AD, Catalano PJ, Haller DG, Mayer RJ, Macdonald JS, Benson III AB et al (2002) Outcomes and toxicity in african-american and caucasian patients in a randomized adjuvant chemotherapy trial for colon cancer. J Natl Cancer Inst 94(15):1160–1167
https://www.albertahealthservices.ca/assets/info/hp/cancer/if-hp-cancer-guide-gi004-early-stage-colon.pdf. Last accessed on 13/2/2021
Cheung WY, Shi Q, O’Connell M, Cassidy J, Blanke CD, Kerr DJ et al (2013) The predictive and prognostic value of sex in early-stage colon cancer: a pooled analysis of 33,345 patients from the ACCENT database. Clin Colorectal Cancer 12(3):179–187
Acknowledgements
The authors would like to acknowledge the significant efforts of the analytical teams at Surveillance and reporting, Cancer Care Alberta, in data extraction for the current study dataset.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study has been approved by Health Research Ethics Board of Alberta (HREBA.CC-20–0215).
Conflict of interest
O.A.: Advisory board with Eisai Canada and Roche Canada. PT: Advisory boards with Roche Canada, Eisai Canada, Teva, Pfizer, Novartis Canada, BMS, Merch, Astrazeneca Canada. SK: None.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abdel-Rahman, O., Tang, P.A. & Koski, S. Hospitalizations among early-stage colon cancer patients receiving adjuvant chemotherapy: a real-world study. Int J Colorectal Dis 36, 1905–1913 (2021). https://doi.org/10.1007/s00384-021-03952-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03952-4