Abstract
Purpose
The role of preoperative carbohydrate antigen 19-9 (CA19-9) in colorectal cancer liver metastases (CRLM) patients is still unclear. The present study aimed to explore the prognostic significance of preoperative CA19-9 in those patients.
Methods
A total of 691 CRLM patients were included in this study. X-tile analyses were performed to determine the optimal cut-off values of CA19-9 and carcinoembryonic antigen (CEA). Prognostic predictors were identified by multivariate analyses.
Results
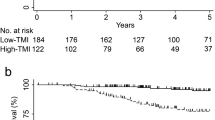
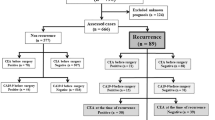
The optimal cut-off values of CA19-9 and CEA for 5-year recurrence-free survival (RFS) were 35.24 U/ml and 20.4 ng/ml, respectively. Patients with high-level CA19-9 had significantly worse RFS and overall survival (OS) than those with low-level CA19-9 (P = 0.001 and P = 0.002, respectively). In addition, patients with high-level CA19-9 had poor RFS and OS (P = 0.028 and P = 0.011, respectively) at low-level CEA. Multivariate analyses confirmed that preoperative CA19-9 was an independent predictor for RFS (hazard ratio [HR] 1.295; 95% confidence interval [CI] 1.043–1.607; P = 0.019) but not for OS (HR 1.213; 95% CI 0.902–1.631; P = 0.201).
Conclusion
CA19-9 is a promising predictor of recurrence for CRLM patients undergoing hepatectomy, and an effective supplement for patients with low-level CEA.




Similar content being viewed by others
Data availability
All data and material relevant to the study are available from the authors upon request.
References
Abe S, Kawai K, Ishihara S, Nozawa H, Hata K, Kiyomatsu T, Tanaka T, Watanabe T (2016) Prognostic impact of carcinoembryonic antigen and carbohydrate antigen 19-9 in stage IV colorectal cancer patients after R0 resection. J Surg Res 205(2):384–392. https://doi.org/10.1016/j.jss.2016.06.078
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, Giacchetti S, Paule B, Kunstlinger F, Ghémard O et al (2004) Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg 240(4):256–644. https://doi.org/10.1097/01.sla.0000141198.92114.f6
Andreou A, Aloia TA, Brouquet A, Dickson PV, Zimmitti G, Maru DM, Kopetz S, Loyer EM, Curley SA, Abdalla EK et al (2013) Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg 257(6):1079–1088. https://doi.org/10.1097/SLA.0b013e318283a4d1
Benson ABI, Venook AP, Al-Hawary MM, Cederquist L, Chen Y, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF et al (2018a) NCCN guidelines insights colon cancer, version 2.2018 featured updates to the NCCN guidelines. J Natl Compr Canc Netw 16(4):359–369. https://doi.org/10.6004/jnccn.2018.0021
Benson ABI, Venook AP, Al-Hawary MM, Cederquist L, Chen Y, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF et al (2018b) Rectal cancer, version 2.2018 clinical practice guidelines in oncology. J Natl Compr Canc Netw 16(7):874–901. https://doi.org/10.6004/jnccn.2018.0061
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Butte JM, Gönen M, Allen PJ, Peter Kingham T, Sofocleous CT, Dematteo RP, Fong Y, Kemeny NE, Jarnagin WR, D’Angelica MI (2015) Recurrence after partial hepatectomy for metastatic colorectal cancer: potentially curative role of salvage repeat resection. Ann Surg Oncol 22(8):2761–2771. https://doi.org/10.1245/s10434-015-4370-1
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 10(21):7252–7259. https://doi.org/10.1158/1078-0432.CCR-04-0713
Chen Y, Chang W, Ren L, Chen J, Tang W, Liu T, Jian M, Liu Y, Wei Y, Xu J (2020) Comprehensive evaluation of relapse risk (CERR) score for colorectal liver metastases: development and validation. The Oncologist 25(7):e1031–e1041. https://doi.org/10.1634/theoncologist.2019-0797
Clavien P, Petrowsky H, Deoliveira ML, Graf R (2007) Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 356(15):1545–1559. https://doi.org/10.1056/NEJMra065156
Creasy JM, Sadot E, Koerkamp BG, Chou JF, Gonen M, Kemeny NE, Balachandran VP, Kingham TP, Dematteo RP, Allen PJ et al (2018) Actual 10-year survival after hepatic resection of colorectal liver metastases: what factors preclude cure? Surgery 163(6):1238–1244. https://doi.org/10.1016/j.surg.2018.01.004
Dupré A, Jones RP, Diaz-Nieto R, Fenwick SW, Poston GJ, Malik HZ (2017) Curative-intent treatment of recurrent colorectal liver metastases: a comparison between ablation and resection. Eur J Surg Oncol 43(10):1901–1907. https://doi.org/10.1016/j.ejso.2017.08.008
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318, 318-321. https://doi.org/10.1097/00000658-199909000-00004
Hof J, Wertenbroek MWJL, Peeters PMJG, Widder J, Sieders E, de Jong KP (2016) Outcomes after resection and/or radiofrequency ablation for recurrence after treatment of colorectal liver metastases. Br J Surg 103(8):1055–1062. https://doi.org/10.1002/bjs.10162
Imai K, Allard MA, Benitez CC, Vibert E, Sa Cunha A, Cherqui D, Castaing D, Bismuth H, Baba H, Adam R (2016) Early recurrence after hepatectomy for colorectal liver metastases: what optimal definition and what predictive factors? Oncologist 21(7):887–894. https://doi.org/10.1634/theoncologist.2015-0468
Ito T, Sugiura T, Okamura Y, Yamamoto Y, Ashida R, Uesaka K (2019) The impact of posthepatectomy liver failure on long-term survival after hepatectomy for colorectal liver metastasis. HPB (Oxford). 21(9):1185–1193. https://doi.org/10.1016/j.hpb.2019.01.008
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey J, Nagorney DM, Mcwilliams RR (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27(22):3677–3683. https://doi.org/10.1200/JCO.2008.20.5278
Leung U, Gönen M, Allen PJ, Kingham TP, Dematteo RP, Jarnagin WR, D Angelica MI (2017) Colorectal cancer liver metastases and concurrent extrahepatic disease treated with resection. Ann Surg 265(1):158–165. https://doi.org/10.1097/SLA.0000000000001624
Louhimo J, Carpelan-Holmström M, Alfthan H, Stenman U, Järvinen HJ, Haglund C (2002) Serum HCGβ, CA 72-4 and CEA are independent prognostic factors in colorectal cancer. Int J Cancer 101(6):545–548. https://doi.org/10.1002/ijc.90009
Lu Z, Peng J, Wang Z, Pan Z, Yuan Y, Wan D, Li B (2016) High preoperative serum CA19-9 level is predictive of poor prognosis for patients with colorectal liver oligometastases undergoing hepatic resection. Med Oncol 33(11):121. https://doi.org/10.1007/s12032-016-0838-5
Marrelli D, Caruso S, Pedrazzani C, Neri A, Fernandes E, Marini M, Pinto E, Roviello F (2009) CA19-9 serum levels in obstructive jaundice: clinical value in benign and malignant conditions. Am J Surg 198(3):333–339. https://doi.org/10.1016/j.amjsurg.2008.12.031
Matsumoto T, Hasegawa S, Hida K, Kawada K, Sakai Y, Sugihara K (2019) Role of repeat resection in patients with metastatic colorectal cancer. Dis Colon Rectum 62(5):561–567. https://doi.org/10.1097/DCR.0000000000001311
Morita S, Nomura T, Fukushima Y, Morimoto T, Hiraoka N, Shibata N (2004) Does serum CA19-9 play a practical role in the management of patients with colorectal cancer? Dis Colon Rectum 47(2):227–232. https://doi.org/10.1007/s10350-003-0041-6
Moro A, Mehta R, Sahara K, Tsilimigras DI, Paredes AZ, Farooq A, Hyer JM, Endo I, Shen F, Guglielmi A et al (2020) The impact of preoperative CA19-9 and CEA on outcomes of patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. https://doi.org/10.1245/s10434-020-08350-8
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole ET, Finch-Jones M et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORCT intergroup trial 40983): a randomised controlled trial. Lancet 371(9617):1007–1016. https://doi.org/10.1016/S0140-6736(08)60455-9
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole ET, Finch-Jones M et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14(12):1208–1215. https://doi.org/10.1016/S1470-2045(13)70447-9
Nuzzo G, Giuliante F, Ardito F, Vellone M, Giovannini I, Federico B, Vecchio FM (2008) Influence of surgical margin on type of recurrence after liver resection for colorectal metastases: a single-center experience. Surgery 143(3):384–393. https://doi.org/10.1016/j.surg.2007.09.038
Raoof M, Haye S, Ituarte PHG, Fong Y (2019) Liver resection improves survival in colorectal cancer patients. Ann Surg 270(4):692–700. https://doi.org/10.1097/SLA.0000000000003485
Reni M, Zanon S, Balzano G, Nobile S, Pircher CC, Chiaravalli M, Passoni P, Arcidiacono PG, Nicoletti R, Crippa S et al (2017) Selecting patients for resection after primary chemotherapy for non-metastatic pancreatic adenocarcinoma. Ann Oncol 28(11):2786–2792. https://doi.org/10.1093/annonc/mdx495
Sakamoto Y, Miyamoto Y, Beppu T, Nitta H, Imai K, Hayashi H, Baba Y, Yoshida N, Chikamoto A, Baba H (2015) Post-chemotherapeutic CEA and CA19-9 are prognostic factors in patients with colorectal liver metastases treated with hepatic resection after oxaliplatin-based chemotherapy. Anticancer Res. 35(4):2359–2368
Tan MCB, Butte JM, Gonen M, Kemeny N, Fong Y, Allen PJ, Kingham TP, Dematteo RP, Jarnagin WR, D’Angelica MI (2013) Prognostic significance of early recurrence: a conditional survival analysis in patients with resected colorectal liver metastasis. HPB 15(10):803–813. https://doi.org/10.1111/hpb.12136
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, Aranda Aguilar E, Bardelli A, Benson A, Bodoky G et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 27(8):1386–1422. https://doi.org/10.1093/annonc/mdw235
Wang Y, Liu Z, Xu D, Liu M, Wang K, Xing B (2019) Fibrinogen-albumin ratio index (FARI): a more promising inflammation-based prognostic marker for patients undergoing hepatectomy for colorectal liver metastases. Ann Surg Oncol 26(11):3682–3692. https://doi.org/10.1245/s10434-019-07586-3
Wu L, Huang P, Wang F, Li D, Xie E, Zhang Y, Pan S (2015) Relationship between serum CA19-9 and CEA levels and prognosis of pancreatic cancer. Ann Transl Med 3(21):328. https://doi.org/10.3978/j.issn.2305-5839.2015.11.17
Yang H, Wang J, Li Z, Yang Y, Yang L, Zhang Y, Shi Y, Cao Y, Zhou J, Wang Z et al (2019) Risk factors and outcomes of early relapse after curative resection of intrahepatic cholangiocarcinoma. Front Oncol 9:854. https://doi.org/10.3389/fonc.2019.00854
Zhou W, Yang F, Peng J, Wang F, Lin Y, Jiang W, Yang X, Li L, Lu Z, Wan D et al (2019) High pretreatment serum CA19-9 level predicts a poor prognosis for patients with stage III colon cancer after curative resection and adjuvant chemotherapy. J Cancer 10(16):3810–3818. https://doi.org/10.7150/jca.31375
Acknowledgments
The authors thank the National Natural Science Foundation of China (No. 81874143, No. 31971192) and Beijing Natural Science Foundation (No. 7192035) for providing financial support for the study. Special thanks go to Xiu-Jian Ma, MD, for critically revising this paper.
Funding
This study was supported by grants from the National Nature Science Foundation of China (No. 81874143, No. 31971192) and Beijing Natural Science Foundation (No. 7192035).
Author information
Authors and Affiliations
Contributions
Concept and design: Jia-Ming Liu, Bao-Cai Xing
Data acquisition: Jia-Ming Liu, Yan-Yan Wang, Da Xu, Kun Wang
Data analyses and interpretation: Jia-Ming Liu, Yan-Yan Wang, Wei Liu
Manuscript drafting: Jia-Ming Liu, Da Xu, Yan-Yan Wang
Critical revision of the manuscript for important intellectual content: Jia-Ming Liu, Kun Wang, Bao-Cai Xing
Supervision: Bao-Cai Xing
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The Ethics Committee of Peking University Cancer Hospital approved this study.
Consent to participate
All materials and data were obtained with agreement from patients and informed consent was signed.
Consent for publication
The approval for publication was given by all co-authors.
Code availability
X-tile software, SPSS 23, and GraphPad Prism 8.0.1 are applied for statistical analyses and figure plotting.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, JM., Wang, YY., Liu, W. et al. Preoperative CA19-9: a competitive predictor of recurrence in patients with colorectal cancer liver metastases after hepatectomy. Int J Colorectal Dis 36, 767–778 (2021). https://doi.org/10.1007/s00384-020-03828-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03828-z