Abstract
Purpose
Adequate lymphadenectomy is critical for accurate nodal staging and planning adjuvant therapy in colon cancer. However, the optimal lymph node (LN) yield for stage II right-sided colon cancer (RSCC) is still unclear. This population-based study aimed to determine the optimal LN yield associated with survival and LN positivity in patients with stage II RSCC.
Methods
All patients with stage II–III RSCC were identified from the Surveillance, Epidemiology, and End Results database over a 10-year interval (2006–2015). The optimal threshold for LN yield was explored using an outcome-oriented approach based on survival and LN positivity.
Results
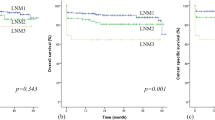
The median number of LNs examined for all 17,385 patients with stage II RSCC was 17 (IQR 12–23). Nineteen LNs were determined as the optimal cut-off point to maximize survival benefit from lymphadenectomy. Increased LN yield was associated with a gradual increase in the risk of node positivity, with no change after 19 nodes. Compared with patients with 19 or more LNs examined, the group with fewer LNs had a significantly poor cancer-specific survival (< 12 nodes: hazard ratio (HR) 2.26, P < 0.001; 12–18 nodes: HR 1.58, P < 0.001) and overall survival (< 12 nodes: HR 1.80, P < 0.001; 12–18 nodes: HR 1.31, P < 0.001). Similar survival results were found in the validation cohort. Patients with older age, small tumor size, and appendix and transverse colon cancer were more likely to receive inadequate LN harvest.
Conclusion
A minimum of 19 LNs is needed to be examined for optimal survival and adequate node staging in lymph node-negative RSCC.


Similar content being viewed by others
References
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67(3):177–193
Weiss JM, Pfau PR, O'Connor ES, King J, LoConte N, Kennedy G, Smith MA (2011) Mortality by stage for right- versus left-sided colon cancer: analysis of surveillance, epidemiology, and end results—Medicare data. J Clin Oncol 29(33):4401–4409
Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, Miedema B, Ota D, Sargent D, National Cancer Institute Expert P (2001) Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 93 (8):583–596
Choi HK, Law WL, Poon JT (2010) The optimal number of lymph nodes examined in stage II colorectal cancer and its impact of on outcomes. BMC Cancer 10:267
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
Del Paggio JC, Peng Y, Wei X, Nanji S, MacDonald PH, Krishnan Nair C, Booth CM (2017) Population-based study to re-evaluate optimal lymph node yield in colonic cancer. Br J Surg 104(8):1087–1096
Vather R, Sammour T, Kahokehr A, Connolly AB, Hill AG (2009) Lymph node evaluation and long-term survival in stage II and stage III colon cancer: a national study. Ann Surg Oncol 16(3):585–593
Peeples C, Shellnut J, Wasvary H, Riggs T, Sacksner J (2010) Predictive factors affecting survival in stage II colorectal cancer: is lymph node harvesting relevant? Dis Colon Rectum 53(11):1517–1523
Swanson RS, Compton CC, Stewart AK, Bland KI (2003) The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol 10(1):65–71
Tsai HL, Lu CY, Hsieh JS, Wu DC, Jan CM, Chai CY, Chu KS, Chan HM, Wang JY (2007) The prognostic significance of total lymph node harvest in patients with T2-4N0M0 colorectal cancer. J Gastrointest Surg 11(5):660–665
Vather R, Sammour T, Zargar-Shoshtari K, Metcalf P, Connolly A, Hill A (2009) Lymph node examination as a predictor of long-term outcome in Dukes B colon cancer. Int J Color Dis 24(3):283–288
Hashiguchi Y, Hase K, Ueno H, Mochizuki H, Kajiwara Y, Ichikura T, Yamamoto J (2010) Prognostic significance of the number of lymph nodes examined in colon cancer surgery: clinical application beyond simple measurement. Ann Surg 251(5):872–881
Chen SL, Bilchik AJ (2006) More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg 244(4):602–610
Stocchi L, Fazio VW, Lavery I, Hammel J (2011) Individual surgeon, pathologist, and other factors affecting lymph node harvest in stage II colon carcinoma. Is a minimum of 12 examined lymph nodes sufficient? Ann Surg Oncol 18(2):405–412
Sarli L, Bader G, Iusco D, Salvemini C, Mauro DD, Mazzeo A, Regina G, Roncoroni L (2005) Number of lymph nodes examined and prognosis of TNM stage II colorectal cancer. Eur J Cancer 41(2):272–279
Hsu CW, Lin CH, Wang JH, Wang HT, Ou WC, King TM (2009) Factors that influence 12 or more harvested lymph nodes in early-stage colorectal cancer. World J Surg 33(2):333–339
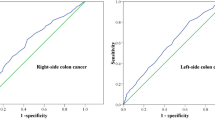
Guan X, Chen W, Liu Z, Jiang Z, Hu H, Zhao Z, Wang S, Chen Y, Wang G, Wang X (2016) Whether regional lymph nodes evaluation should be equally required for both right and left colon cancer. Oncotarget 7(37):59945–59956
Kanemitsu Y, Komori K, Ishiguro S, Watanabe T, Sugihara K (2012) The relationship of lymph node evaluation and colorectal cancer survival after curative resection: a multi-institutional study. Ann Surg Oncol 19(7):2169–2177
Noone AM HN, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA SEER Cancer Statistics Review, 1975-2015, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2015/. Based on November 2017 SEER data submission, posted to the SEER web site, April 2018
Surveillance, Epidemiology, and End Results (SEER) Program research data (1973–2015). National Cancer Institute. http://seer.cancer.gov. Based on November 2017 SEER data submission. Published April 2018.
Raoof M, Nelson RA, Nfonsam VN, Warneke J, Krouse RS (2016) Prognostic significance of lymph node yield in ypN0 rectal cancer. Br J Surg 103(12):1731–1737
Smith DD, Schwarz RR, Schwarz RE (2005) Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol 23(28):7114–7124
Lemmens VE, van Lijnschoten I, Janssen-Heijnen ML, Rutten HJ, Verheij CD, Coebergh JW (2006) Pathology practice patterns affect lymph node evaluation and outcome of colon cancer: a population-based study. Ann Oncol 17(12):1803–1809
Elferink MA, Siesling S, Visser O, Rutten HJ, van Krieken JH, Tollenaar RA, Lemmens VE (2011) Large variation between hospitals and pathology laboratories in lymph node evaluation in colon cancer and its impact on survival, a nationwide population-based study in the Netherlands. Ann Oncol 22(1):110–117
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99(6):433–441
Prandi M, Lionetto R, Bini A, Francioni G, Accarpio G, Anfossi A, Ballario E, Becchi G, Bonilauri S, Carobbi A, Cavaliere P, Garcea D, Giuliani L, Morziani E, Mosca F, Mussa A, Pasqualini M, Poddie D, Tonetti F, Zardo L, Rosso R (2002) Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant trial. Ann Surg 235(4):458–463
McDonald JR, Renehan AG, O'Dwyer ST, Haboubi NY (2012) Lymph node harvest in colon and rectal cancer: current considerations. World J Gastrointest Surg 4(1):9–19
Hernanz F, Revuelta S, Redondo C, Madrazo C, Castillo J, Gomez-Fleitas M (1994) Colorectal adenocarcinoma: quality of the assessment of lymph node metastases. Dis Colon Rectum 37(4):373–376 discussion 376-377
van Erning FN, Crolla RM, Rutten HJ, Beerepoot LV, van Krieken JH, Lemmens VE (2014) No change in lymph node positivity rate despite increased lymph node yield and improved survival in colon cancer. Eur J Cancer 50(18):3221–3229
Ogino S, Nosho K, Irahara N, Shima K, Baba Y, Kirkner GJ, Mino-Kenudson M, Giovannucci EL, Meyerhardt JA, Fuchs CS (2010) Negative lymph node count is associated with survival of colorectal cancer patients, independent of tumoral molecular alterations and lymphocytic reaction. Am J Gastroenterol 105(2):420–433
Samdani T, Schultheis M, Stadler Z, Shia J, Fancher T, Misholy J, Weiser MR, Nash GM (2015) Lymph node yield after colectomy for cancer: is absence of mismatch repair a factor? Dis Colon Rectum 58(3):288–293
Parsons HM, Tuttle TM, Kuntz KM, Begun JW, McGovern PM, Virnig BA (2011) Association between lymph node evaluation for colon cancer and node positivity over the past 20 years. JAMA 306(10):1089–1097
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313(5795):1960–1964
George S, Primrose J, Talbot R, Smith J, Mullee M, Bailey D, du Boulay C, Jordan H, Wessex Colorectal Cancer Audit Working G (2006) Will Rogers revisited: prospective observational study of survival of 3592 patients with colorectal cancer according to number of nodes examined by pathologists. Br J Cancer 95 (7):841–847
Khan H, Olszewski AJ, Somasundar P (2014) Lymph node involvement in colon cancer patients decreases with age; a population based analysis. Eur J Surg Oncol 40(11):1474–1480
Tekkis PP, Smith JJ, Heriot AG, Darzi AW, Thompson MR, Stamatakis JD, Association of Coloproctology of Great B, Ireland (2006) A national study on lymph node retrieval in resectional surgery for colorectal cancer. Dis Colon Rectum 49 (11):1673–1683
Hoshino N, Hasegawa S, Hida K, Kawada K, Sugihara K, Sakai Y (2016) Impact of age on the prognostic value of number of lymph nodes retrieved in patients with stage II colorectal cancer. Int J Color Dis 31(7):1307–1313
Weng NP (2006) Aging of the immune system: how much can the adaptive immune system adapt? Immunity 24(5):495–499
Wright FC, Law CH, Last L, Khalifa M, Arnaout A, Naseer Z, Klar N, Gallinger S, Smith AJ (2003) Lymph node retrieval and assessment in stage II colorectal cancer: a population-based study. Ann Surg Oncol 10(8):903–909
Bui L, Rempel E, Reeson D, Simunovic M (2006) Lymph node counts, rates of positive lymph nodes, and patient survival for colon cancer surgery in Ontario, Canada: a population-based study. J Surg Oncol 93(6):439–445
Nash GM, Row D, Weiss A, Shia J, Guillem JG, Paty PB, Gonen M, Weiser MR, Temple LK, Fitzmaurice G, Wong WD (2011) A predictive model for lymph node yield in colon cancer resection specimens. Ann Surg 253(2):318–322
Bertelsen CA, Neuenschwander AU, Jansen JE, Wilhelmsen M, Kirkegaard-Klitbo A, Tenma JR, Bols B, Ingeholm P, Rasmussen LA, Jepsen LV, Iversen ER, Kristensen B, Gogenur I, Danish Colorectal Cancer G (2015) Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 16(2):161–168
Bertelsen CA, Neuenschwander AU, Jansen JE, Kirkegaard-Klitbo A, Tenma JR, Wilhelmsen M, Rasmussen LA, Jepsen LV, Kristensen B, Gogenur I, Copenhagen Complete Mesocolic Excision S, Danish Colorectal Cancer G (2016) Short-term outcomes after complete mesocolic excision compared with ‘conventional’ colonic cancer surgery. Br J Surg 103 (5):581–589
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30(15):1763–1769
Fleischmann I, Warschkow R, Beutner U, Marti L, Schmied BM, Steffen T (2017) Improved survival after retrieval of 12 or more regional lymph nodes in appendiceal cancer. Eur J Surg Oncol 43(10):1876–1885
Reese JA, Hall C, Bowles K, Moesinger RC (2009) Colorectal surgical specimen lymph node harvest: improvement of lymph node yield with a pathology assistant. J Gastrointest Surg 13(8):1459–1463
Acknowledgements
We thank all the staff members of the National Cancer Institute who have participated in the Surveillance, Epidemiology, and End Results (SEER) program.
Funding
This study was supported in part by the Qianjiang Talent Project of Zhejiang Province (Grant/Award Numbers: 2013R10079).
Author information
Authors and Affiliations
Contributions
All authors meet the ICMJE authorship criteria and contributed substantially to the manuscript. X Zhu, HX Ju, and YB Cai designed the study conception. YB Cai, GP Cheng, and XG Lu finished the analysis and interpretation of data. YB Cai and X Zhu drafted the work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Fig. S1
Kaplan–Meier CSS curves for patients with stage II RSCC according to number of LNs examined (<12 vs. 12-18 vs. ≥ 19 nodes). A CSS in patients with older age. B CSS in patients with small tumor size. C, CSS in patients with appendix cancer. D, CSS in patients with transverse colon cancer. (TIF 4479 kb)
ESM2
(PNG 454 kb)
Rights and permissions
About this article
Cite this article
Cai, Y., Cheng, G., Lu, X. et al. The re-evaluation of optimal lymph node yield in stage II right-sided colon cancer: is a minimum of 12 lymph nodes adequate?. Int J Colorectal Dis 35, 623–631 (2020). https://doi.org/10.1007/s00384-019-03483-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03483-z