Abstract
Purpose
To explore the influence of postoperative Hirschsprung-associated enterocolitis (post-HAEC) on long-term outcomes and to identify risk factors of post-HAEC.
Methods
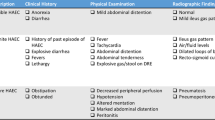
The medical records of 304 eligible patients diagnosed with Hirschsprung’s disease (HSCR) were reviewed. We analyzed the clinical characteristics of post-HAEC and its influence on long-term outcomes. Furthermore, risk factors for early and recurrent HAEC were identified separately.
Results
The overall incidence of post-HAEC was 29.9% (91/304). We categorized early HAEC as occurring within postoperative 3 months (n = 39) and recurrent HAEC as occurring ≥ 3 episodes within postoperative 6 months (n = 25). Patients with early HAEC were more likely to experience worse nutritional status, defecation function, and quality of life compared to those with late or no episodes (P < 0.05). Similarly, the adverse influences of recurrent HAEC on these outcomes were also significant (P < 0.05). The risk factors for early HAEC included preoperative undernutrition, long-segment HSCR, and postoperative Grade 3–4 complications within 30 days. For recurrent HAEC, risk factors were preoperative malnutrition, non-parental caregivers, long-segment HSCR, and postoperative Grade 3–4 complications within 30 days.
Conclusion
Classification of post-HAEC based on the first episode time and frequency was necessary. The earlier or more frequent episodes of post-HAEC have detrimental influences on long-term outcomes. Furthermore, risk factors for early and recurrent HAEC were different.





Similar content being viewed by others
Data availability
The data presented in this study are available on request from the corresponding author.
References
Montalva L, Cheng LS, Kapur R et al (2023) Hirschsprung disease. Nat Rev Dis Primers 9(1):54. https://doi.org/10.1038/s41572-023-00465-y
Beltman L, Labib H, Ahmed H et al (2023) Transition zone pull-through in patients with hirschsprung disease: is redo surgery beneficial for the long-term outcomes? J Pediatr Surg 58(10):1903–1909. https://doi.org/10.1016/j.jpedsurg.2023.02.043
More K, Rao S, McMichael J et al (2014) Growth and developmental outcomes of infants with hirschsprung disease presenting in the neonatal period: a retrospective study. J Pediatr 165(1):73-77.e2. https://doi.org/10.1016/j.jpeds.2014.02.062
Roorda D, Oosterlaan J, van Heurn E et al (2021) Risk factors for enterocolitis in patients with Hirschsprung disease: a retrospective observational study. J Pediatr Surg 56(10):1791–1798. https://doi.org/10.1016/j.jpedsurg.2021.04.020
Yan J, Sun J, Wu R et al (2020) Barium enema findings in total colonic aganglionosis: a single-center, retrospective study. BMC Pediatr 20(1):499. https://doi.org/10.1186/s12887-020-02403-3
Kyrklund K, Sloots C, de Blaauw I et al (2020) ERNICA guidelines for the management of rectosigmoid Hirschsprung’s disease. Orphanet J Rare Dis 15(1):164. https://doi.org/10.1186/s13023-020-01362-3
Wood RJ, Garrison AP (2022) Total colonic aganglionosis in hirschsprung disease. Semin Pediatr Surg 31(2):151165. https://doi.org/10.1016/j.sempedsurg.2022.151165
Li S, Zhang Y, Li K et al (2023) Update on the pathogenesis of the Hirschsprung-associated enterocolitis. Int J Mol Sci 24(5):4602. https://doi.org/10.3390/ijms24054602
Chantakhow S, Tepmalai K, Singhavejsakul J et al (2023) Prognostic factors of postoperative Hirschsprung-associated enterocolitis: a cohort study. Pediatr Surg Int 39(1):77. https://doi.org/10.1007/s00383-023-05364-7
Liu J, Dong R, Chen G et al (2019) Risk factors and prognostic effects of cholangitis after kasai procedure in biliary atresia patients: a retrospective clinical study. J Pediatr Surg 54(12):2559–2564. https://doi.org/10.1016/j.jpedsurg.2019.08.026
Li Z, Bai B, Ji G et al (2018) Relationship between Clavien-Dindo classification and long-term survival outcomes after curative resection for gastric cancer: a propensity score-matched analysis. Int J Surg 60:67–73. https://doi.org/10.1016/j.ijsu.2018.10.044
Chung P, Yu M, Wong K et al (2019) Risk factors for the development of post-operative enterocolitis in short segment Hirschsprung’s disease. Pediatr Surg Int 35(2):187–191. https://doi.org/10.1007/s00383-018-4393-3
Huang SC, Chen JS, Cheng CN et al (2012) Hypoalbuminaemia is an independent predictor for hemophagocytic lymphohistiocytosis in childhood Epstein-Barr virus-associated infectious mononucleosis. Eur J Haematol 89(5):417–422. https://doi.org/10.1111/ejh.12006
McLean TW, Stewart RM, Curley TP et al (2020) Hypoalbuminemia in children with cancer treated with chemotherapy. Pediatr Blood Cancer 67(2):e28065. https://doi.org/10.1002/pbc.28065
Mertens A, Benjamin-Chung J, Colford JM Jr et al (2023) Child wasting and concurrent stunting in low- and middle-income countries. Nature 621(7979):558–567. https://doi.org/10.1038/s41586-023-06480-z
Monica Carissa T et al (2022) Long-term functional outcomes of patients with Hirschsprung disease following pull-through. BMC Pediatr 22(1):246. https://doi.org/10.1186/s12887-022-03301-6
Liu Z, Zhang Y, Li S et al (2023) Long-term bowel function after single-stage transanal endorectal pull-through in neonatal patients with Hirschsprung disease. Pediatr Surg Int 39(1):255. https://doi.org/10.1007/s00383-023-05517-8
Koo F, Chan M, King SK et al (2023) The early years: Hirschsprung disease and health-related quality of life. Qual Life Res 32(12):3327–3337. https://doi.org/10.1007/s11136-023-03482-2
Yamashita Y, Shirabe K, Tsuijita E et al (2013) Third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Surgery 154(5):1038–1045. https://doi.org/10.1016/j.surg.2013.04.046
Zhang X, Sun D, Xu Q et al (2023) Risk factors for Hirschsprung disease-associated enterocolitis: a systematic review and meta-analysis. Int J Surg 109(8):2509–2524. https://doi.org/10.1097/JS9.0000000000000473
Rosso M, Fremion E, Santoro SL et al (2020) Down syndrome disintegrative disorder: a clinical regression syndrome of increasing importance. Pediatrics 145(6):e20192939. https://doi.org/10.1542/peds.2019-2939
Wang D, Zhu T, Zhu L et al (2023) Screening of undernutrition in children with Hirschsprung disease using preoperative anthropometric parameters: a multicenter cross-sectional study. JPEN J Parenter Enteral Nutr 47(1):151–158. https://doi.org/10.1002/jpen.2440
Bechard LJ, Rothpletz-Puglia P, Touger-Decker R et al (2013) Influence of obesity on clinical outcomes in hospitalized children: a systematic review. JAMA Pediatr 167(5):476–482. https://doi.org/10.1001/jamapediatrics.2013.13
Conrey PE, Denu L, O’Boyle KC et al (2023) IgA deficiency destabilizes homeostasis toward intestinal microbes and increases systemic immune dysregulation. Sci Immunol. https://doi.org/10.1126/sciimmunol.ade2335
Sun H, Bi J, Lei Q et al (2018) Partial enteral nutrition increases intestinal sIgA levels in mice undergoing parenteral nutrition in a dose-dependent manner. Int J Surg 49:74–79. https://doi.org/10.1016/j.ijsu.2017.12.011
Jiao CL, Chen XY, Feng JX (2016) Novel insights into the pathogenesis of Hirschsprung’s-associated enterocolitis. Chin Med J (Engl) 129(12):1491–1497. https://doi.org/10.4103/0366-6999.183433
Parahita IG, Makhmudi A, Gunadi. (2018) Comparison of Hirschsprung-associated enterocolitis following soave and Duhamel procedures. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2017.07.010
Xie C, Yan J, Zhang Z et al (2022) Risk factors for Hirschsprung-associated enterocolitis following soave: a retrospective study over a decade. BMC Pediatr 22(1):654. https://doi.org/10.1186/s12887-022-03692-6
Taylor MA, Bucher BT, Reeder RW et al (2021) Comparison of Hirschsprung disease characteristics between those with a history of postoperative enterocolitis and those without: results from the pediatric colorectal and pelvic learning consortium. Eur J Pediatr Surg 31(3):207–213. https://doi.org/10.1055/s-0040-1716876
Le-Nguyen A, Righini-Grunder F, Piché N et al (2019) Factors influencing the incidence of Hirschsprung associated enterocolitis (HAEC). J Pediatr Surg 54(5):959–963. https://doi.org/10.1016/j.jpedsurg.2019.01.026
Zhang GW, Lin JH, Qian JP et al (2014) Analyzing risk factors for early postoperative bile leakage based on Clavien classification in bile duct stones. Int J Surg 12(8):757–761. https://doi.org/10.1016/j.ijsu.2014.05.079
Rohit A, Kirkham R, McCarthy L et al (2021) Exploring differences in perceptions of child feeding practices between parents and health care professionals: a qualitative study. BMC Public Health 21(1):1449. https://doi.org/10.1186/s12889-021-11493-2
Harvey L, Bryant-Waugh R, Watkins B et al (2015) Parental perceptions of childhood feeding problems. J Child Health Care 19(3):392–401. https://doi.org/10.1177/1367493513509422
Knaus ME, Pendola G, Srinivas S et al (2023) Social determinants of health and Hirschsprung-associated enterocolitis. J Pediatr Surg 58(8):1458–1462. https://doi.org/10.1016/j.jpedsurg.2022.09.039
Lardner DR, Dick BD, Crawford S (2010) The effects of parental presence in the postanesthetic care unit on children’s postoperative behavior: a prospective, randomized, controlled study. Anesth Analg 110(4):1102–1108. https://doi.org/10.1213/ANE.0b013e3181cccba8
Pastor AC, Osman F, Teitelbaum DH et al (2009) Development of a standardized definition for Hirschsprung’s-associated enterocolitis: a Delphi analysis. J Pediatr Surg 44(1):251–256. https://doi.org/10.1016/j.jpedsurg.2008.10.052
Frykman PK, Kim S, Wester T et al (2018) Critical evaluation of the Hirschsprung-associated enterocolitis (HAEC) score: a multicenter study of 116 children with Hirschsprung disease. J Pediatr Surg 53(4):708–717. https://doi.org/10.1016/j.jpedsurg.2017.07.009
Funding
This study was supported by research grants from the National Clinical Research Center for Child Health and Disorders, Children’s Hospital of Chongqing Medical University (No.NCRCCHD-2022-GP-03) and Program for Youth Innovation in Future Medicine, Chongqing Medical University (No.W0125).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study’s conception and design. Data collection and analysis were performed by Wei Feng and Yi Wang. The first draft of the manuscript was written by Wei Feng and Linxiao Fan, and all the authors commented on previous versions of the manuscript. All the authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
The study was approved by the Institutional Research Ethics Board of Children’s Hospital affiliated Chongqing Medical University (Date: 2021/No: 391).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, W., Zhang, B., Fan, L. et al. Clinical characteristics and influence of postoperative Hirschsprung-associated enterocolitis: retrospective study at a tertiary children’s hospital. Pediatr Surg Int 40, 106 (2024). https://doi.org/10.1007/s00383-024-05688-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-024-05688-y