Abstract
Background
The aim of this study was to assess long-term outcomes of neonatal patients with Hirschsprung disease (HD) after single-stage transanal endorectal pull-through (TEPT) and to explore the predictive factors contributing to subnormal bowel function.
Methods
Patients aged > 3 years operated for HD with TEPT during neonatal period between 2007 and 2019 answered the bowel function score (BFS) questionnaire. The patients were retrospectively divided into two groups according to whether they had normal bowel function. The clinical variables were compared between the subnormal and normal BFS groups. Univariate and multivariable logistic regression analysis were performed to identify the predictive factors contributing to subnormal bowel function.
Results
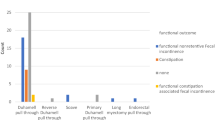
A total of 160 children (71.7%) were included in this study, with mean follow-up time of 7.3 years (range 3.0–15.1 years). The level of aganglionosis were determined to be the short-segment (124/160, 77.5%), long-segment (33/160, 20.6%), and TCA (3/160, 1.9%). One hundred and thirty-four patients (83.8%) had a BFS ≥ 17, and 26 patients (16.2%) with subnormal bowel function (BFS < 17). Univariate and multivariate logistic regression analysis showed that level of aganglionosis with long-segment or TCA and postoperative hospital stay > 8.5 days were independent risk factors with OR of 3.213 (1.252, 8.246) and 3.813 (1.371, 10.606) for subnormal BFS, respectively.
Conclusion
Most HD patients who underwent one-stage TEPT in the neonatal period have favorable long-term results, and the level of aganglionosis with long-segment or TCA and long postoperative hospital stay may be closely related to subnormal bowel function.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Tam PKH (2016) Hirschsprung’s disease: a bridge for science and surgery. J Pediatr Surg 51(1):18–22. https://doi.org/10.1016/j.jpedsurg.2015.10.021
Murakami J (2018) Clinical practice guidelines for allied disorders of Hirschsprung’s disease. Pediatr Int 60(5):399. https://doi.org/10.1111/ped.13585
De la Torre-Mondragón L, Ortega-Salgado J (1998) Transanal endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg 33(8):1283–1286. https://doi.org/10.1016/s0022-3468(98)90169-5
Mao Y-Z, Tang S-T, Li S (2018) Duhamel operation vs. transanal endorectal pull-through procedure for Hirschsprung disease: a systematic review and meta-analysis. J Pediatr Surg 53(9):1710–1715. https://doi.org/10.1016/j.jpedsurg.2017.10.047
Obata S et al (2019) The outcomes of transanal endorectal pull-through for Hirschsprung’s disease according to the mucosectomy-commencing points: a study based on the results of a nationwide survey in Japan. J Pediatr Surg 54(12):2546–2549. https://doi.org/10.1016/j.jpedsurg.2019.08.035
Teitelbaum D et al (2000) A decade of experience with the primary pull-through for Hirschsprung disease in the newborn period: a multicenter analysis of outcomes. Ann Surg 232(3):372–380. https://doi.org/10.1097/00000658-200009000-00009
Vũ P, Thien H, Hiep P (2010) Transanal one-stage endorectal pull-through for Hirschsprung disease: experiences with 51 newborn patients. Pediatr Surg Int 26(6):589–592. https://doi.org/10.1007/s00383-010-2599-0
Bjørnland K et al (2017) A Nordic multicenter survey of long-term bowel function after transanal endorectal pull-through in 200 patients with rectosigmoid Hirschsprung disease. J Pediatr Surg 52(9):1458–1464. https://doi.org/10.1016/j.jpedsurg.2017.01.001
Fosby MV, Stensrud KJ, Bjørnland K (2020) Bowel function after transanal endorectal pull-through for Hirschsprung disease—does outcome improve over time? J Pediatr Surg 55(11):2375–2378. https://doi.org/10.1016/j.jpedsurg.2020.04.010
Neuvonen MI et al (2017) Bowel function and quality of life after transanal endorectal pull-through for Hirschsprung disease: controlled outcomes up to adulthood. Ann Surg 265(3):622–629. https://doi.org/10.1097/sla.0000000000001695
Gunadi et al (2021) Functional outcomes of patients with short-segment Hirschsprung disease after transanal endorectal pull-through. BMC Gastroenterol 21(1):85. https://doi.org/10.1186/s12876-021-01668-x
Zhang Y et al (2022) One-stage transanal endorectal pull-through for Hirschsprung disease: experience with 229 neonates. Pediatr Surg Int 38(11):1533–1540. https://doi.org/10.1007/s00383-022-05198-9
Zhang Y et al (2022) One-stage transanal endorectal pull-through for Hirschsprung disease: experience with 229 neonates. Pediatr Surg Int. https://doi.org/10.1007/s00383-022-05198-9
Kim S-H, Cho Y-H, Kim H-Y (2021) Assessment of defecation function beyond infantile period for transanal single-stage endorectal pull-through in Hirschsprung disease. Ann Surg Treat Res 101(4):231–239. https://doi.org/10.4174/astr.2021.101.4.231
Rintala RJ, Lindahl HG, Rasanen M (1997) Do children with repaired low anorectal malformations have normal bowel function? J Pediatr Surg 32(6):823–826. https://doi.org/10.1016/s0022-3468(97)90628-x
Kyrklund K et al (2012) Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4 to 26 years. Dis Colon Rectum 55(6):671–676. https://doi.org/10.1097/DCR.0b013e31824c77e4
Jarvi K et al (2010) Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg 252(6):977–981. https://doi.org/10.1097/SLA.0b013e3182018542
Conway SJ et al (2007) Early adult outcome of the Duhamel procedure for left-sided Hirschsprung disease—a prospective serial assessment study. J Pediatr Surg 42(8):1429–1432. https://doi.org/10.1016/j.jpedsurg.2007.03.046
Xiong X et al (2015) Long term quality of life in patients with Hirschsprung’s disease who underwent heart-shaped anastomosis during childhood: a twenty-year follow-up in China. J Pediatr Surg 50(12):2044–2047. https://doi.org/10.1016/j.jpedsurg.2015.08.027
Dai Y et al (2020) Long-term outcomes and quality of life of patients with Hirschsprung disease: a systematic review and meta-analysis. BMC Gastroenterol 20(1):67. https://doi.org/10.1186/s12876-020-01208-z
Granéli C et al (2017) Diagnosis, symptoms, and outcomes of Hirschsprung’s disease from the perspective of gender. Surg Res Pract 2017:9274940. https://doi.org/10.1155/2017/9274940
Prato AP et al (2008) Hirschsprung disease: do risk factors of poor surgical outcome exist? J Pediatr Surg 43(4):612–619. https://doi.org/10.1016/j.jpedsurg.2007.10.007
Chumpitazi BP, Nurko S (2011) Defecation disorders in children after surgery for Hirschsprung disease. J Pediatr Gastroenterol Nutr 53(1):75–79. https://doi.org/10.1097/MPG.0b013e318212eb53
Ludman L et al (2002) Hirschsprung’s disease: functional and psychological follow up comparing total colonic and rectosigmoid aganglionosis. Arch Dis Child 86(5):348–351. https://doi.org/10.1136/adc.86.5.348
Kawaguchi AL et al (2021) Management and outcomes for long-segment Hirschsprung disease: a systematic review from the APSA Outcomes and Evidence Based Practice Committee. J Pediatr Surg 56(9):1513–1523. https://doi.org/10.1016/j.jpedsurg.2021.03.046
Lu C et al (2023) Bowel function at preschool and early childhood age in children with long-segment Hirschsprung disease. Eur J Pediatr. https://doi.org/10.1007/s00431-023-04814-7
Chen Y et al (2013) Transanal endorectal pull-through versus transabdominal approach for Hirschsprung’s disease: a systematic review and meta-analysis. J Pediatr Surg 48(3):642–651. https://doi.org/10.1016/j.jpedsurg.2012.12.036
Ven TJVD et al (2013) Transanal endorectal pull-through for classic segment Hirschsprung’s disease: with or without laparoscopic mobilization of the rectosigmoid? J Pediatr Surg 48(9):1914–1918. https://doi.org/10.1016/j.jpedsurg.2013.04.025
Zhang Z et al (2023) Long-term Bowel function and pediatric health-related quality of life after transanal rectal mucosectomy and partial internal anal sphincterectomy pull-through for Hirschsprung disease. Front Pediatr 11:1099606. https://doi.org/10.3389/fped.2023.1099606
Acknowledgements
We thank all authors for their contributions to the article.
Funding
There is no fund.
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Medical Ethics Committee of the Beijing Children’s Hospital (2020-Z-082), and was performed according to the Declaration of Helsinki. The informed consent was waived by the Medical Ethics Committee of the Beijing Children’s Hospital due to the retrospective design of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Z., Zhang, Y., Li, S. et al. Long-term bowel function after single-stage transanal endorectal pull-through in neonatal patients with Hirschsprung disease. Pediatr Surg Int 39, 255 (2023). https://doi.org/10.1007/s00383-023-05517-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05517-8