Abstract
The COVID-19 pandemic has changed the way to manage the emergencies, as people faced fear of the hospitals, with possible delay in the diagnosis. Moreover, clinicians had to rearrange protocols for diagnosis and treatment. We aimed to assess whether COVID-19 pandemic influenced severity of inflammation, management, and outcomes of acute appendicitis (AA), when compared to the pre-COVID era. Using defined search strategy, two independent investigators identified those studies comparing pediatric AA during COVID-19 pandemic versus the pre-COVID-19 period. Meta-analysis was performed using RevMan 5.3. Data are mean ± SD. Of 528 abstracts, 36 comparative studies were included (32,704pts). Time from symptoms onset to surgery was longer during the pandemics compared to the pre-COVID-19 (1.6 ± 0.9 versus 1.4 ± 0.9 days; p < 0.00001). Minimally Invasive Surgery was similar during COVID-19 (70.4 ± 30.2%) versus control period (69.6 ± 25.3%; p = ns). Complicated appendicitis was increased during the pandemics (35.9 ± 14.8%) compared to control period (33.4 ± 17.2%; p < 0.0001). Post-operative complications were comparable between these two groups (7.7 ± 6.5% versus 9.1 ± 5.3%; p = ns). It seems that the COVID-19 pandemic influenced the time of diagnosis, severity of inflammation, and type of surgery. However, the number of post-operative complications was not different between the two groups, leading to the conclusion that the patients were correctly managed.
Level of Evidence
Level 3 Meta-analysis on Level 3 studies
Similar content being viewed by others
Introduction
Since the breakthrough of the Coronavirus-19 (COVID-19) pandemic, there have been a change and a rearrangement both in the society and in the worldwide healthcare [1,2,3].
During the lockdown, people were less prone to attend the emergency department (ED) due to the fear of contracting the COVID-19, leading to a delayed diagnosis of several diseases [1, 3,4,5,6,7].
Acute appendicitis (AA) is the most common pediatric surgical emergency, and its severity is strictly related to the time of diagnosis: a delayed diagnosis increases the risk of developing complications, such as abscess, peritonitis, sepsis, and wound infection [5, 8].
The gold standard of care for acute appendicitis is appendectomy (through a minimally invasive or open approach). Even if the non-operative management is a well-established procedure in adults, its use among children is not completely defined up to now [2, 8,9,10].
Although the COVID-19 affects adults more than children, the pandemic has also influenced the management of the pediatric surgical patient [2, 3, 11,12,13]. Coronavirus infection, in fact, can present with gastrointestinal symptoms in both adults and children, thus increasing the risk of misdiagnoses [2, 10, 14]. Moreover, during the lockdown, the surgical activity has been reduced to the sole emergency surgery and the conversion of peripheral hospitals into COVID hospitals has increased the risk of delayed diagnosis of acute appendicitis [2, 8, 11, 13].
The aim of our study was to assess whether the COVID-19 pandemic influenced the management of AA in children in:
-
Diagnosis (age at diagnosis, time from symptoms onset and hospital presentation)
-
Severity of inflammation
-
Management (non-operative management, minimally invasive surgery and/or open surgery)
-
Outcomes (length of hospital stay and post-operative complications).
Material and methods
Data sources and study selection
This study was registered on the international prospective register of systematic reviews PROSPERO (registration #CRD42022325941) (National institute for Health Research) [15]. The systematic review was drafted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [16].
A systematic review of the English literature was made using a defined search strategy (Table 1). Two investigators (MEM, GLa) independently searched scientific databases (PubMed, Cochrane Collaboration, Scopus, and Web of Science) looking for studies reporting on acute appendicitis during the COVID19 pandemic in children published up to September 2023. MeSH headings and terms used are “Acute appendicitis”, “Appendicitis”, “COVID-19”, “SARS-CoV-2”, ‘‘Pediatric”, and “Children” (Fig. 1). Reference lists were searched to identify relevant cross-references. Case reports, opinion articles, experimental studies, and case series with less than 10 patients were excluded. All grey literature publications (i.e. reports, theses, conference proceedings, bibliographies, commercial documentations, and official documents not published commercially) were excluded. Full text articles of potentially eligible studies were retrieved and independently assessed for suitability by two investigators (MEM, GLa). We included all studies (trials, cohort, and case–control) that reported at least one outcome of interest. Furthermore, we included in the meta-analysis only those studies comparing the management of acute appendicitis in children before and after the spreading of COVID19 pandemic. If two or more studies had overlapping patient cohorts, for each outcome measure we included only the article with the largest number of patients. Any disagreement over the eligibility of a specific study was resolved through the discussion with a third author (GLi).
Statistical analysis
Categorical variable frequencies were compared using Pearson’s chi-square test or the two-tailed Fisher exact probability test, as appropriate. When median and range were reported, mean ± SD were estimated, as previously reported [17]. Meta-analysis of comparative studies was conducted with RevMan 5.4 [18]. Data are presented as risk ratio (RR) for categorical variables, and mean differences (MD) for continuous variables, along with 95% confidence intervals (CI) using the random-effects model, with p values shown for Z test for overall significance and I2 statistic for heterogeneity. A p-value < 0.05 was considered statistically significant. Data are expressed as mean ± SD.
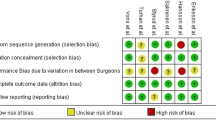
Quality assessment
Risk of bias for individual studies was assessed in duplicate (DDR and VC) using the methodological index for non-randomized studies (MINORS) [19]. Differences between the two reviewers (DDR and VC) were resolved through consensus and discussion with a third author (GLa). The total score for this 12-item instrument ranges 0–24 points with a validated “gold standard” cut-off of 19.8. We assessed the methodological quality for each outcome by grading the quality of evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology [20]. Quality of evidence was rated as high, moderate, low, and very low for each outcome. Observational studies start with a low quality of evidence. The quality of evidence was rated down in the presence of risk of bias, inconsistency, indirectness, imprecision, and publication bias. For assessment of risk of bias in observational studies, we used the MINORS instrument. Inconsistency was determined according to heterogeneity. We produced I2 values to assess heterogeneity. I2 value of 0–40, 30–60, 50–90, and 75–100% were considered as low, moderate, substantial, and considerable heterogeneity, respectively. Imprecision was assessed using optimal information size (OIS), which was based on 25% relative risk reduction, 0.05 of α error and 0.20 of β error [21].
Results
Of 528 title/abstract screened, 129 full-text articles were analyzed, 43 studies entered the qualitative analysis [1,2,3,4,5,6,7,8,9,10,11, 13, 14, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51], and 36 papers were included in the meta-analysis [1,2,3,4,5,6,7,8, 11, 13, 22, 23, 25,26,27,28, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44, 46,47,48,49,50] (32,704 pts, Fig. 2).
The age at presentation of symptoms was similar during COVID-19 pandemic (10.6 ± 1.2 years) when compared to the pre-COVID-19 era (10.7 ± 1.2 years; p = ns, MD -0.22, 95% confidence intervals (CI) [-0.49, 0.05], I2 = 95%; Fig. 3a). The mean time from symptoms onset to surgery was significantly lengthened in the COVID-19 period compared to the pre-pandemic era (1.6 ± 0.9 versus 1.4 ± 0.9 days, respectively; p < 0.00001, MD 0.24, 95% CI [0.16, 0.32], I2 = 95%; Fig. 3b).
When reported, minimally invasive surgery (MIS) did not appear to be decreased during the pandemic (4,468/6,343 cases, 70.4 ± 30.2%) versus the control period (4,303/6,178 cases, 69.6 ± 25.3%; p = ns, RR 0.99, 95% CI [0.94, 1.03], I2 = 80%, Fig. 4a). However, the number of complicated appendicitis was significantly increased during the pandemic (5,311/14,808 children, 35.9 ± 14.8%) compared to the control period (5,885/17,603 children, 33.4 ± 17.2%; p < 0.0001, RR 1.29, 95% CI [1.14, 1.45], I2 = 90%; Fig. 4b). Also, the non-operative management (NOM) was significantly increased during the COVID-19 pandemic compared to the previous period (1,199/11,138 patients, 10.8 ± 16.5% versus 555/11,937 patients, 4.6 ± 3.3%, respectively; p = 0.02; RR 1.77, 95% CI [1.10, 2.87], I2 = 83%; Fig. 4c). Moreover, the incidence of negative appendicitis was significantly decreased during the pandemic (382/8,872 children, 4.3 ± 8.5%) compared to the control period (564/8,216 children, 6.9 ± 9.8%); p = 0.02, RR 0.58, 95% CI [0.36, 0.92], I2 = 89%; Fig. 4d).
Nonetheless, we did not find a statistically significant increase of post-operative complications during the COVID-19 pandemic (876/11,387 patients, 7.7 ± 6.5%) compared to the previous period (1,120/12,353 patients, 9.1 ± 5.3%; p = ns, RR 0.93, 95% CI [0.73, 1.18], I2 = 73%, Fig. 5a). Finally, the length of hospital stay (LOS) was similar between the pandemic period (3.4 ± 2.1 days) and the pre-COVID-19 era (3.8 ± 1.4 days; p = ns, MD 0.02, 95% CI [-0.29, 0.34], I2 = 95%; Fig. 5b).
Discussion
Acute appendicitis is the most common pediatric surgical emergency with up to 8% of children complaining of abdominal pain having a diagnosis of appendicitis [8].
The most common complication of AA is perforation, and its incidence is directly correlated with the duration of symptoms and age of the patient [5]. The higher rate of complicated appendicitis among very young children has to be referred to their difficulty to define their symptoms [5].
The increased rate of complicated appendicitis during the COVID-19 pandemic reported by several Authors was explained by the fear of contracting the virus in the hospitals, leading to a late referral to the emergency department and therefore to a delayed diagnosis [3, 5,6,7,8, 10, 12,13,14]. As a matter of fact, in our study we have found an overall increased time-lapse from symptoms onset to surgery that could be related to the finding of a significantly higher number of complicated appendicitis during the pandemic compared to the pre-pandemic era. Moreover, in our study the mean age at presentation was similar among the two study groups, thus removing any possible bias given by different age populations.
It has also been postulated that the COVID-19 infection itself could increase the rate of complicated appendicitis, due to the gastrointestinal manifestation of the disease and this assumption may also explain our results [6].
The management of children with AA during the pandemic is also controversial. Some Authors, in fact, postulated an increased risk of contagion during laparoscopy due to aerosolization of peritoneal fluids [2, 10, 22]. Therefore, the ESPES (European Society of Pediatric Endoscopic Surgeons) recommended the use of a closed system for CO2 insufflation and de-sufflation, limiting the use of the electrocautery [51]. When analyzing our data, in fact, we did not find a reduced use of the minimally invasive surgery (MIS) during the pandemic when compared to the pre-COVID-19 period. However, we did find fewer negative appendicitis during the pandemic when compared to the pre-COVID-19 period.
Another question raised during the COVID-19 era is the use of the NOM as the first-line treatment of the AA. Some surgeons, in fact, preferred to avoid the use of NOM to reduce the overall length of hospital stay and to avoid the risk of failure of NOM that may have led to an increased risk of complications, length of hospital stays, and readmissions [2, 5, 8, 12]. Some others, however, preferred the use of NOM to limit hospital access and to reduce the number of surgical procedures, and this was especially true during the strict lockdown [9, 52]. Moreover, the ESPES suggested to consider the use of NOM, whenever safe for the patient [51]. Indeed, in our study, we found an overall increased use of the NOM in children during the pandemic when compared to the same period pre-COVID-19.
Nonetheless, despite the higher incidence of complicated AA, we did not find an increased number of postoperative complications as well as a lengthened hospital stay, as demonstrated by other Authors, thus leading to the conclusion that children were appropriately treated [53].
Limitation of the study
We are aware of the limitations of our study, which rely on the quality of the studies and data available in the literature, as any other meta-analysis.
All the 36 studies included in the meta-analysis were retrospective observational studies [1,2,3,4,5,6,7,8, 11, 13, 22, 23, 25,26,27,28, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44, 46,47,48,49,50]. None of the papers provided sample size calculations. As expected, a blinded evaluation of objective endpoints was not possible and groups were not contemporary, because of different time-period between cases and controls. Moreover, none of the study have reported with regards to the loss to follow-up and there were a broad lack of data regards the length of follow-up. Therefore, in our meta-analysis, none of the studies reached the gold standard cut-off on MINORS of 19.8 out of 24 (Supplementary file 1).
According to the GRADE methodology, the quality of evidence of the meta-analysis was low with regards all the pre-operative data (age at presentation, time from symptoms onset to surgery), the management of AA (minimally invasive appendectomies, incidence of complicated appendicitis, percentage of NOM, and percentage of negative appendicitis) and post-operative outcomes (incidence of complication) (Table 2). Although the data were obtained from a considerable number of studies, their considerable heterogeneity could generate possible bias.
However, when independently assessed by two authors (DDR and VC) using A Measurement Tool to Assess Systematic Reviews (AMSTAR) [54], the present systematic review and meta-analysis received a decent score (Supplementary file 2).
The PRISMA checklist was then completed (Supplementary file 3).
Conclusions
The correct management of children with acute appendicitis during the COVID-19 pandemic is still debated.
The number of complicated appendicitis has increased during this period, and it seems to be directly related to the delayed referral to the hospital.
Up to now the use of laparoscopy is not contraindicated in the COVID-positive patients. As a matter of fact, the use of the MIS during the pandemic was not decreased when compared to the pre-pandemic era.
Even if the delayed diagnosis could influence the outcomes, the incidence of complications seems not to be increased during pandemic, thus leading to the conclusion that the choice of the surgical management (either open, MIS, or NOM) was still correct for each patient.
Data availability
All data supporting the findings of this systematic review and meta-analysis are available within the paper and its Supplementary files. Further data with regards results (e.g. list of excluded studies with reasons) are available from the corresponding author upon reasonable request.
Abbreviations
- AA:
-
Acute appendicitis
- MIS:
-
Minimally invasive surgery
- NOM:
-
Non-operative management
References
Ali S, Khan MA, Rehman IU et al (2020) Impact of covid 19 pandemic on presentation, treatment and outcome of paediatric surgical emergencies. J Ayub Med Coll Abbottabad 32:S621–S624 (PMID: 33754519)
Montalva L, Haffreingue A, Ali L et al (2020) The role of a pediatric tertiary care center in avoiding collateral damage for children with acute appendicitis during the COVID-19 outbreak. Pediatr Surg Int 36:1397–1405. https://doi.org/10.1007/s00383-020-04759-0
Bellini T, Rotulo GA, Carlucci M et al (2021) Complicated appendicitis due to diagnosis delay during lockdown period in Italy. Acta Paediatr 110(1959–60):1–2. https://doi.org/10.1111/apa.15756
MoratillaLapeña L, Delgado-Miguel C, Sarmiento Caldas MC et al (2021) Impact of SARS-CoV-2 pandemic on emergency department activity at the pediatric surgery unit of a third-level hospital. Cir Pediatr 1(34):85–89 (PMID: 33826261)
Gerall CD, DeFazio JR, Kahan AM et al (2021) Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg 56:905–910. https://doi.org/10.1016/j.jpedsurg.2020.10.008
Lee-Archer P, Blackall S, Campbell H et al (2020) Increased incidence of complicated appendicitis during the COVID-19 pandemic. J Paediatr Child Health 56:1313–1314. https://doi.org/10.1111/jpc.15058
Place R, Lee J, Howell J (2020) Rate of pediatric appendiceal perforation at a children’s hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw Open 1(3):e2027948. https://doi.org/10.1001/jamanetworkopen.2020.27948
Velayos M, Muñoz-Serrano AJ, Estefanía-Fernández K et al (2020) Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis. An Pediatr (Engl Ed) 93:118–122. https://doi.org/10.1016/j.anpede.2020.04.010
Kvasnovsky CL, Shi Y, Rich BS et al (2021) Limiting hospital resources for acute appendicitis in children: Lessons learned from the U.S. epicenter of the COVID-19 pandemic. J Pediatr Surg 56:900–904. https://doi.org/10.1016/j.jpedsurg.2020.06.024
Mehl SC, Loera JM, Shah SR et al (2021) Favorable postoperative outcomes for children with COVID-19 infection undergoing surgical intervention: experience at a free-standing children’s hospital. J Pediatr Surg 56:2078–2085. https://doi.org/10.1016/j.jpedsurg.2021.01.033
La Pergola E, Sgrò A, Rebosio F et al (2020) Appendicitis in children in a Large Italian COVID-19 pandemic area. Front Pediatr 9(8):600320. https://doi.org/10.3389/fped.2020.600320
Sheath C, Abdelrahman M, MacCormick A et al (2021) Paediatric appendicitis during the COVID-19 pandemic. J Paediatr Child Health 57(7):986–989. https://doi.org/10.1111/jpc.15359
Raffaele A, Cervone A, Ruffoli M et al (2020) Critical factors conditioning the management of appendicitis in children during COVID-19 pandemic: experience from the outbreak area of Lombardy, Italy. Br J Surg 107:e529. https://doi.org/10.1002/bjs.12004
Malhotra A, Sturgill M, Whitley-Williams P et al (2021) Pediatric COVID-19 and appendicitis: a gut reaction to SARS-CoV-2? Pediatr Infect Dis J 1(40):e49-55. https://doi.org/10.1097/INF.0000000000002998
PROSPERO international prospective register of systematic reviews. Available at: https://www.crd.york.ac.uk/prospero [on 25th Sep 2023]
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 21(6):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 20(5):13. https://doi.org/10.1186/1471-2288-5-13
(2014) Review Manager (RevMan). The Nordic Cochrane Centre. The Cochrane Collaboration, Copenhagen
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Dupont WD, Plummer WD (1990) Power and sample size calculations: a review and computer program. Control Clin Trials 11:116–128. https://doi.org/10.1016/0197-2456(90)90005-m
Bada-Bosch I, de Agustín JC, de la Torre M et al (2021) Pediatric surgical activity during the SARS-CoV-2 pandemic: experience at a tertiary hospital. Cir Pediatr 1(34):28–33 (PMID: 33507641)
Patel M, Thomas JJ, Sarwary H (2021) We can reduce negative paediatric appendicectomy rate: a cohort study. Ann Med Surg (Lond) 5(71):102901. https://doi.org/10.1016/j.amsu.2021.102901
Basnet AT, Singh S, Thapa B et al (2021) Management of acute appendicitis during COVID-19 pandemic in a tertiary care centre: a descriptive cross-sectional study. JNMA J Nepal Med Assoc. https://doi.org/10.31729/jnma.6307
Horst KK, Kolbe AB, McDonald JS et al (2021) Imaging pediatric acute appendicitis during the coronavirus disease 2019 (COVID-19) pandemic: collateral damage is variable. Pediatr Radiol 51:1991–1999. https://doi.org/10.1007/s00247-021-05128-2
Esparaz JR, Chen MK, Beierle EA et al (2021) Perforated appendicitis during a pandemic: the downstream effect of COVID-19 in children. J Surg Res 268:263–266. https://doi.org/10.1016/j.jss.2021.07.008
Percul C, Cruz M, Meza AC et al (2021) Impact of the COVID-19 pandemic on the pediatric population with acute appendicitis: experience at a general, tertiary care hospital. Arch Argent Pediatr 119:224–229. https://doi.org/10.5546/aap.2021.eng.224
Colvin D, Lawther S (2021) A surge in appendicitis: management of paediatric appendicitis during the COVID-19 surge in the royal belfast Hospital for sick children. Ulster Med J 90:86–89 (PMID: 34276086)
Yock-Corrales A, Lenzi J, Ulloa-Gutiérrez R et al (2021) Acute abdomen and appendicitis in 1010 pediatric patients with COVID-19 or MIS-C: a multinational experience from Latin America. Pediatr Infect Dis J 40(10):e364–e369. https://doi.org/10.1097/INF.0000000000003240
Theodorou CM, Beres AL, Nguyen M et al (2021) Statewide impact of the COVID pandemic on pediatric appendicitis in California: a multicenter study. J Surg Res 267:132–142. https://doi.org/10.1016/j.jss.2021.05.023
Schäfer FM, Meyer J, Kellnar S et al (2021) Increased incidence of perforated appendicitis in children during COVID-19 pandemic in a Bavarian multi-center study. Front Pediatr 9:683607. https://doi.org/10.3389/fped.2021.683607
Kanamori D, Kurobe M, Sugihara T et al (2022) Increase in pediatric complicated appendicitis during the COVID-19 pandemic: a multi-center retrospective study. Surg Today 52:1741–1745. https://doi.org/10.1007/s00595-022-02529-0
Bethell GS, Gosling T, Rees CM et al (2022) Impact of the COVID-19 pandemic on management and outcomes of children with appendicitis: the children with appendicitis during the coronavirus pandemic (CASCADE) study. J Pediatr Surg 57(10):380–385. https://doi.org/10.1016/j.jpedsurg.2022.03.029
Nassiri AM, Pruden RD, Holan CA et al (2022) Pediatric appendicitis in the time of the COVID-19 pandemic: a retrospective chart review. J Am Coll Emerg Physicians Open. https://doi.org/10.1002/emp2.12722
Collaborative ANZSCRAFT, Roberts K (2022) Impact of COVID-19 on appendicitis presentations in children in Australia and New Zealand. ANZ J Surg 92:736–741. https://doi.org/10.1111/ans.17566
Li C, Saleh A (2022) Effect of COVID-19 on pediatric appendicitis presentations and complications. J Pediatr Surg 57:861–865. https://doi.org/10.1016/j.jpedsurg.2021.12.047
Delgado-Miguel C, Garcia Urbán J, Del Monte FC et al (2022) Impact of the COVID-19 pandemic on acute appendicitis in children. J Health Qual Res 37:225–230. https://doi.org/10.1016/j.jhqr.2021.12.005
Pawelczyk A, Kowalska M, Tylicka M et al (2021) Impact of the SARS-CoV-2 pandemic on the course and treatment of appendicitis in the pediatric population. Sci Rep 14(11):23999. https://doi.org/10.1038/s41598-021-03409-2
van Amstel P, El Ghazzaoui A, Hall NJ et al (2022) Paediatric appendicitis: international study of management in the COVID-19 pandemic. Br J Surg 14(109):1044–1048. https://doi.org/10.1093/bjs/znac239
Hegde B, Garcia E, Hu A et al (2023) Management of pediatric appendicitis during the COVID-19 pandemic: a nationwide multicenter cohort study. J Pediatr Surg 58:1375–1382. https://doi.org/10.1016/j.jpedsurg.2022.08.005
Taşçı A, Gürünlüoğlu K, Yıldız T et al (2022) Impact of COVID-19 pandemic on pediatric appendicitis hospital admission time and length of hospital stay. Ulus Travma Acil Cerrahi Derg. https://doi.org/10.14744/tjtes.2021.06777. (English)
Toro Rodríguez MG, Dore Reyes M, MartínezCastaño I et al (2022) Have acute appendicitis complications increased in children as a result of SARS-CoV-2? Cir Pediatr. https://doi.org/10.54847/cp.2022.03.16. (English, Spanish PMID: 35796085)
SenerOkur D, Memetoglu ME, Edirne Y (2022) Impact of the COVID-19 pandemic and the restrictions on pediatric appendicitis in Turkey: a single-center experience. Pediatr Int 64:e15272. https://doi.org/10.1111/ped.15272
Ayyıldız HN, Mirapoglu S, Yıldız ZA et al (2022) What has changed in children’s appendicitis during the COVID-19 pandemic? Ulus Travma Acil Cerrahi Derg 28:1674–1681. https://doi.org/10.14744/tjtes.2021.51000
Iantorno SE, Skarda DE, Bucher BT (2023) Concurrent SARS-COV-19 and acute appendicitis: management and outcomes across United States children’s hospitals. Surgery 173:936–943. https://doi.org/10.1016/j.surg.2022.12.004
Del Giorgio F, Habti M, Merckx J et al (2023) Investigating changes in incidence and severity of pediatric appendicitis during the COVID-19 pandemic in Canada- an interrupted time series analysis. World J Pediatr 19:288–292. https://doi.org/10.1007/s12519-022-00656-9
Quaglietta PR, Ramjist JK, Antwi J et al (2023) Unanticipated consequences of COVID-19 pandemic policies on pediatric acute appendicitis surgery. J Pediatr Surg 58:931–938. https://doi.org/10.1016/j.jpedsurg.2023.01.021
Öztaş T, Bilici S, Dursun A (2023) Has the frequency of complicated appendicitis changed in children in the first year of the COVID-19 pandemic? Ann Pediatr Surg 19:3. https://doi.org/10.1186/s43159-022-00235-7
Dass D, Hotonu S, McHoney M et al (2023) Prospective study of laparoscopic management of appendicitis during the COVID pandemic in a single paediatric centre. Afr J Paediatr Surg 20:40–45. https://doi.org/10.4103/ajps.ajps_181_21
Matava CT, Tighe NTG, Baertschiger R et al (2023) Patient and process outcomes among pediatric patients undergoing appendectomy during the COVID-19 pandemic: an international retrospective cohort study. Anesthesiology 139:35–48. https://doi.org/10.1097/ALN.0000000000004570
Pini Prato A, Conforti A, Almstrom M et al (2020) Management of COVID-19-positive pediatric patients undergoing minimally invasive surgical procedures: systematic review and recommendations of the board of European society of pediatric endoscopic surgeons. Front Pediatr 8:259. https://doi.org/10.3389/fped.2020.00259
Emile SH (2022) Finding a place for non-operative management of acute appendicitis: COVID-19 as an example. Am J Surg 223:605–606. https://doi.org/10.1016/j.amjsurg.2021.09.003
Head WT, Parrado RH, Cina RA (2023) Impact of the coronavirus (COVID-19) pandemic on the care of pediatric acute appendicitis. Am Surg 89:1527–1532. https://doi.org/10.1177/00031348211067995
Shea BJ, Grimshaw JM, Wells GA et al (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10. https://doi.org/10.1186/1471-2288-7-10
Funding
Open access funding provided by Università degli Studi G. D'Annunzio Chieti Pescara within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
MEM, GLa, GLi: Conception/design, analysis, and interpretation, participated in drafting, gave final approval. MEM, GLa: Data acquisition. GLa, DDR, VC: Quality assessment. DDR, VC: Participated in revision
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miscia, M.E., Lauriti, G., Di Renzo, D. et al. Management and outcomes of acute appendicitis in children during the COVID-19 pandemic: a systematic review and meta-analysis. Pediatr Surg Int 40, 11 (2024). https://doi.org/10.1007/s00383-023-05594-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05594-9