Abstract
Purpose
The aim of the study was to compare and evaluate the utility of three different risk stratification scores for gastroschisis neonates; simple/complex gastroschisis, gastroschisis prognostic score and risk stratification index.
Methods
Data of neonates born with gastroschisis between the years 1993 and 2015 were collected. The national registers and patient records of four Finnish University Hospitals were retrospectively reviewed. Logistic and linear regression analysis were performed to identify independent predictors for adverse outcomes. The efficacy of these prognostic methods was further assessed using ROC-curves and DeLong (1988) test.
Results
Gastroschisis risk stratification index was an acceptable predictor of in-hospital mortality, AUC 0.70, 95% CI 0.48–0.91, p = 0.049. Complex gastroschisis and gastroschisis prognostic score were able to predict short bowel syndrome, AUC 0.80, 95% CI 0.58–1.00, p = 0.012 and AUC 0.80, 95% CI 0.59–1.00, p = 0.012, respectively.
Conclusion
There are three easily obtainable risk stratification scores for outcome prediction in gastroschisis patients, however, their predictive ability did not have a statistical difference in the present study. The Gastroschisis risk stratification index seemed to perform moderately well in mortality prediction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroschisis is a congenital defect of the anterior abdominal wall, characterized by prolapse of intestine and other abdominal organs outside the abdominal cavity. Surgical correction is required soon after delivery. The prevalence of gastroschisis is increasing worldwide and has been reported to be 1 to 5 in 10000 live births. [1,2,3]. Survival rates have been published to be greater than 90% [2, 4, 5]. The negative impact of additional intestinal anomalies or bowel compromise have described in the literature and division to simple and complex gastroschisis (complicated by atresia, perforation, necrosis and/or volvulus) is the most common categorization method [6, 7]. Cowan and colleagues introduced a Gastroschisis Prognostic Score (GPS) in 2012, which is a risk stratification method based on visual assessment of bowel appearance after delivery. It includes the following variables: matting, necrosis, atresia and perforation. [8]. Elevated scores have been shown to associate with increased length of stay, increased total time of parenteral nutrition, increased time to enteral feeds and mortality [8] in addition to complications [9]. Another risk score for gastroschisis is the Gastroschisis Risk Stratification Index (GRSI), which includes intestinal atresia, necrotizing enterocolitis, rare cardiac anomalies and lung hypoplasia to identify patients at greatest risk for mortality. This method was shown to successfully identify infants at a high risk for death. [10]. To our knowledge, studies comparing multiple risk assessment modalities for gastroschisis are scarce in the current literature. These scoring systems could provide valuable information to both clinicians and researchers.
The aim of the study was to compare and evaluate the utility of three different risk stratification scores for gastroschisis neonates; simple/complex gastroschisis, GPS and GRSI.
Materials and methods
Patients
We conducted a retrospective study of neonates born with gastroschisis and treated at the Pediatric Surgery Departments of four University hospitals, Tampere, Turku, Kuopio and Oulu, in Finland from 1993 to 2015. Unfortunately, we do not have data from the fifth university hospital Helsinki, which would have made the database nationwide. Gastroschisis patients were identified from the hospital registers based on the diagnoses according to International Classification of Diseases (ICD-9 code 756.73, after the year 1994 Q79.3 ICD-10 code). Data regarding maternal factors, prenatal observations, initial presentation at birth, surgical treatment, post-operative treatment, complications and short-term outcomes were collected from the patient files at each hospital, the Finnish Medical Birth Register and the Finnish Register of Congenital Malformations maintained by the Finnish Institution for Health and Welfare. The mean follow-up time of this database was 11 years. The institutional review boards of the participating hospitals and the Finnish Institution for Health and Welfare accepted the study. The need for patients’ written consent was waived.
Definitions
The birth weight z score was obtained using the contemporary Finnish Birth size reference [11]. Small for Gestational Age (SGA) was defined as birth weight below – 2 Standard deviation. Organ prolapse was defined as any intra-abdominal organ fully or partially protruding trough the fascial defect at birth, excluding small and large intestine. Patients with associated bowel atresia, bowel perforation, bowel necrosis or volvulus were defined to have a complex gastroschisis, as suggested by Molik and Abdullah [6, 12]. GRSI includes a scoring system for intestinal atresia, necrotizing enterocolitis, rare cardiac anomalies and pulmonary hypoplasia with range of 0–10 points. Atresia gives 1, NEC 2, rare cardiac anomalies 3 and pulmonary hypoplasia 4 points [10]. Rare cardiac anomalies were selected according to Arnold et al. Points of GPS range from 0 to 12 and variables are matting, atresia, perforation and necrosis [8, 9]. Descriptions of bowel injury were based on the study and instructions for use by Cowan et al. [13]. Points of matting are 0 for none, 1 for mild and 4 for severe. Absent atresia, perforation or necrosis values 0, suspected atresia 1, present atresia or perforation 2 and present necrosis 4.
Outcome endpoints
The primary endpoints of the present study were to compare and evaluate the function of three different risk stratification scores for gastroschisis neonates in Finland; simple/complex gastroschisis, GPS and GRSI. Our outcomes of interest were in-hospital mortality, short bowel syndrome, positive blood culture, intravenous nutrition time, in-hospital stay in days and a re-laparotomy for any of the following—perforation, ischemia or necrosis of the bowel.
Statistical analysis
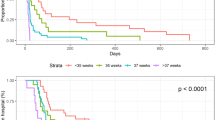
Statistical analysis was performed using SPSS software (version 25.0, IBM Corporation, New York, USA). No attempt to replace missing values was made. Categorical variables are reported as counts and percentages. Continuous variables are reported as means and standard deviations. Logistic and linear regression analysis were performed to identify independent predictors for adverse outcomes. The following variables were included in the multivariate models: gestational age, birth weight, Apgar score at 5 min of age, gender, hospital transfer after delivery, prenatal diagnose known, any organ prolapse other than bowel and twin status in addition to each risk stratification method individually. Receiver operating characteristic curves (ROC) were used to assess the discriminatory power of GPS, GRSI and simple/complex gastroschisis. ROC is a quantitative measure of the ability of a diagnostic tool to differentiate between dichotomous events. Area under the curve (AUC) values were calculated to compare these models in a free web-based application [14] with DeLong (1988) test [15]. All statistical tests were performed as two-tailed and a p value ≤ 0.05 represented statistical significance. AUC values depicting the accuracy of risk stratification were classified as fail (0.50–0.59), poor (0.60–0.69), moderate (0.70–0.79), good (0.80–0.89) and excellent (0.90–1.00).
Results
A total of 156 newborns with gastroschisis were born between January 1993 and December 2015. Thirteen neonates were excluded, one who received most of the treatment in a non-participating center, one with missing patient records and 11 not having all variables needed to measure the scores. Altogether 143 neonates were included in the study. Perinatal characteristics are summarized in Table 1. There were 79 male (55.2%) and 64 female infants. Gastroschisis was prenatally diagnosed in 123 cases (86.0%). Ten patients (7.0%) were born in a central hospital and required transfer to a University Hospital postnatally. The average birth weight and gestational age were 2530 ± 564 g and 36.7 ± 1.8 weeks, respectively. Vaginal delivery rate was 31.5 percent. Nine infants died before discharge from hospital (6.3%). Re-laparotomy for bowel perforation, ischemia or necrosis was performed for seven infants (4.9%). Short bowel syndrome was diagnosed in 6 cases (4.2%) and 21 infants had a positive blood culture (14.7%). The mean duration of parenteral nutrition and hospital stay were 55.3 ± 198.4 and 39.2 ± 50.0 days, respectively.
Numbers of infants classified into each risk prediction model are presented in Table 2. Comparison of risk prediction models in patients with gastroschisis are presented in Tables 3 and 4. ROC-curves were drawn for dichotomized variables. GPS was found to reliably predict short bowel syndrome, AUC 0.80, 95% CI 0.59–1.00, p = 0.012, as was also classification to complex gastroschisis, AUC 0.80, 95% CI 0.58–1.00, p = 0.012. GRSI was a moderate predictor of in-hospital mortality, AUC 0.70, 95% CI 0.48–0.91, p = 0.049. Furthermore, we conducted multivariate models adjusted for relevant perinatal variables and beforementioned risk scores. Gastroschisis prognostic score was found to be an independent predictor for short bowel syndrome, OR 1.63, 95% CI 1.07–2.50, p = 0.023. Gastroschisis risk stratification index was an independent predictor for re-laparotomy for perforation, ischemia, necrosis and also for in-hospital death, OR 4.27, 95% CI 1.40–13.07, p = 0.011 and OR 6.38 95% CI 1.66–24.51, p = 0.007, respectively. Complex gastroschisis was associated with increased length of stay, p = 0.000.
We compared the areas under the ROC-curves of GPS, GRSI and complex gastroschisis with DeLong (1988) test. There were no significant differences between these risk stratification scores in any of the outcome endpoints (in-hospital mortality, re-laparotomy for perforation, ischemia, necrosis, short bowel syndrome, positive blood culture, intravenous nutrition time and in-hospital stay in days).
Discussion
The present study demonstrates the function of three different risk stratification scores. Our comparison analysis shows that their ability to predict specific outcome measures differed from each other. In our study cohort, only GRSI was an independent predictor for in-hospital mortality, but not the other studied outcome measures. Gastroschisis prognostic score and complex gastroschisis classifications were only able to predict reliably short bowel syndrome.
The literature has provided evidence that there are different types of gastroschisis with varying clinical outcomes of morbidity and mortality [6, 7, 16, 17]. Our results are in line with these studies.
Molik et al. and Arnold et al. showed in their studies with 103 and 4344 gastroschisis infants that cases with complex gastroschisis had decreased survival [6, 18]. Complex gastroschisis was significantly associated with death according to Arnold et al. (2007) [18]. Molik et al. reported 32 (31.0%) complex cases in their study. All deceased patients were classified as complex, which resulted in a mortality rate of 28.0% among this patient group [6]. The incidence of complex gastroschisis reported by Arnold et al. was 474 cases (10.9%) [18], which is similar to our finding of 20 complex cases out of 143 gastroschisis infants (14.0%). Their study reported that coexisting bronchopulmonary dysplasia had a higher prevalence in the complex group. Moreover, cardiac diseases were more common in this patient population. [18]. Furthermore, Laje et al. evaluated outcomes and complications during initial hospitalization of 125 simple and 58 complex gastroschisis cases. There was no neonatal mortality. [19]. Complex gastroschisis has been associated with longer mechanical ventilator time [6], parenteral nutrition time and in-hospital stay [6, 19].
GPS and complex gastroschisis classifications are based on bowel appearance after delivery [6,7,8, 18]. In the study by Cowan et al., the interobserver correlation with GPS risk score calculation was shown to be reliable between different surgeons [8]. On the contrary, utilization of the GRSI score requires additional examinations, such as ultrasound or additional postnatal imaging [10], which prevents the score from being used at bedside or immediately after birth.
Arnold et al. developed GRSI to predict death in gastroschisis using data consisting of 4310 patients with gastroschisis from 1988 to 2002. They divided the patients into two subgroups according to the risk of mortality. High-risk patients have scores greater or equal to 3 and low-risk patients fewer or equal to 2. Infants classified in the high-risk group had greater than a 10% risk of death compared to the low-risk group, with an overall mortality of 3.0% [18]. Interestingly, there was a statistically significant difference between mortality rates of high-risk group (GRSI) and complex gastroschisis group [7], 29.4% vs. 9.6%, respectively, p = 0.02.
Indeed, it could be speculated that the small number of patients and the relatively long follow-up period in this study could introduce a bias based on the improvement of care over time. However, the treating hospital or the time-frame of birth did not have an effect on mortality in a study by Tauriainen et al. (2021), which was based mostly on the same database [20]. On this basis, the results of the present study can be considered reliable.
The limitations of present study include the retrospectively collected data with some missing values and relatively small sample size. We speculate that the small number of patients in our high-risk groups might have prevented us from obtaining significant results. We do not have photographs of the appearance of protruding intestines or organs. The risk scoring was performed using only electronic and paper patient records. In addition to before mentioned scores, Score for Neonatal Acute Physiology, Version II (SNAP-II) and Score for Neonatal Acute Physiology, Perinatal Extension, Version II (SNAPPE-II), are also designed for measurement of illness severity for all neonates requiring intensive care. SNAP-II is based on six different vital signs and laboratory tests and SNAPPE-II adds to points for to birth weight, low Apgar score and small for gestational age (SGA) [21]. However, we were unable to utilize SNAP-II or SNAPPE-II scoring methods due to lack of data.
Conclusions
In conclusion, there are three easily obtainable risk stratification scores for outcome prediction in gastroschisis patients with different predictive profiles. However, their predictive ability did not have a statistical difference. The Gastroschisis risk stratification index performed moderately well in mortality prediction, whereas gastroschisis prognostic score and complex gastroschisis were able to identify reliably patients suffering from short bowel syndrome. Further studies with larger databases are needed to compare these risk scores in more detail.
References
Mastroiacovo P, Lisi A, Castilla EE (2006) The incidence of gastroschisis: research urgently needs resources. BMJ 7538:423–424
Raitio A, Lahtinen A, Syvänen J et al (2020) Gastroschisis in Finland 1993 to 2014 -increasing prevalence, high rates of abortion, and survival: a population-based study. Eur J Pediatr Surg 6:536–540. https://doi.org/10.1055/s-0039-3401797
Brebner A, Czuzoj-Shulman N, Abenhaim HA (2020) Prevalence and predictors of mortality in gastroschisis: a population-based study of 4803 cases in the USA. J Matern Fetal Neonatal Med 10:1725–1731
Raymond SL, Hawkins SB, St Peter SD et al (2020) Predicting morbidity and mortality in neonates born with gastroschisis. J Surg Res 245:217–224
Fullerton BS, Velazco CS, Sparks EA et al (2017) Contemporary outcomes of infants with gastroschisis in north America: a multicenter cohort study. J Pediatr 188:192–197
Molik KA, Gingalewski CA, West KW et al (2001) Gastroschisis: a plea for risk categorization. J Pediatr Surg 1:51–55
Caniano DA, Brokaw B, Ginn-Pease ME (1990) An individualized approach to the management of gastroschisis. J Pediatr Surg 3:297–300
Cowan KN, Puligandla PS, Laberge JM et al (2012) The gastroschisis prognostic score: reliable outcome prediction in gastroschisis. J Pediatr Surg 47:1111–1117
Puligandla PS, Baird R, Skarsgard ED et al (2017) Outcome prediction in gastroschisis-the gastroschisis prognostic score (GPS) revisited. J Pediatr Surg 5:718–721
Arnold MA, Chang DC, Nabaweesi R et al (2007) Development and validation of a risk stratification index to predict death in gastroschisis. J Pediatr Surg 6:950–955
Sankilampi U, Hannila M-L, Saari A et al (2013) New population-based references for birth weight, length, and head circumference in singletons and twins from 23 to 43 gestation weeks. Ann Med 5–6:446–454
Abdullah F, Arnold MA, Nabaweesi R et al (2007) Gastroschisis in United States 1988–2003: analysis and risk categorization of 4344 patients. J Perinatol 1:50–55
http://www.capsnetwork.org/portal/About/AboutCAPSNet.aspx, accessed on 29th of July, 2021.
http://www.biosoft.hacettepe.edu.tr/easyROC/. Accessed 23 May 2020
Goksuluk D, Korkmaz S, Zararsiz G, Karaagaoglu AE (2016) EasyROC: an interactive web-tool for ROC curve analysis using R language environment. R J 8(2):213–230
Snyder CL, Miller KA, Sharp RJ et al (2001) Management of intestinal atresia in patients with gastroschisis. J Pediatr Surg 10:1542–1545
Raymond SL, Hawkins RB, St Peter SD et al (2020) Predicting morbidity and mortality in neonates born with gastroschisis. J Surg Res 245:217–224
Arnold MA, Chang DC, Nabaweesi R et al (2007) Risk stratification of 4344 patients with gastroschisis into simple and complex categories. J Pediatr Surg 9:1520–1525
Laje P, Fraga MV, Peranteau WH et al (2018) Complex gastroschisis: clinical spectrum and neonatal outcomes at referral center. J Pediatr Surg 10:1904–1907
Tauriainen A, Hyvärinen A, Raitio A et al (2021) Different strategies, equivalent treatment approaches in terms of mortality in four university hospitals: a retrospective multicenter study of gastroschisis in Finland. Pediatr Surg Int 11:1521–1529
Richardson DK, Corcoran JD, Escobar GJ et al (2001) SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 138:92–100
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Contributions
AT- study design, drafting of the manuscript, data collection, acceptance of the final manuscript. AR- data collection, critical review of the manuscript, acceptance of the final manuscript. TT- study design, drafting of the manuscript, data collection, statistical analysis, acceptance of the final manuscript. KV- critical review of the manuscript, acceptance of the final manuscript. US- critical review of the manuscript, acceptance of the final manuscript. IH- critical review of the manuscript, acceptance of the final manuscript. AH- data collection, critical review of the manuscript, acceptance of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tauriainen, A., Raitio, A., Tauriainen, T. et al. Comparison of three risk stratification scores in gastroschisis neonates: gastroschisis prognostic score, gastroschisis risk stratification index and complex gastroschisis. Pediatr Surg Int 38, 1377–1383 (2022). https://doi.org/10.1007/s00383-022-05180-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05180-5