Abstract
Introduction
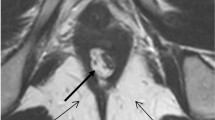
The levator ani (LA) complex in high-type imperforate anus (H-IA), low-type imperforate anus (L-IA), and Hirschsprung’s disease (HD) patients as controls were documented using magnetic resonance imaging (MRI) and compared for symmetry.
Materials and methods
Mean left:right LA thickness ratio (LA ratio), and deviation of the LA from the pubococcygeal line (PCL; LA angle) were calculated from thin-slice MRI images (axial 2 mm, coronal 2 mm, and sagittal 3 mm) of the puborectalis and pubococcygeus taken parallel to the PCL under sedation in H-IA (n=14), L-IA (n=16), and HD (n=9).
Results
MRI scans were performed between January 2018 and June 2021. LA were significantly thinner in H-IA (1.78±0.46 mm) compared with L-IA (2.97±0.55 mm) and controls (2.87±0.32 mm), p<0.0001. LA ratio was significantly lower in H-IA (0.71±0.15) compared with L-IA (0.93±0.04), and controls (0.91±0.06), p<0.0001. Mean LA-angle was significantly different in H-IA, 10.8° (range 6°–19°), versus L-IA and controls, both zero degrees (range 0°–5°), p<0.0001, respectively.
Conclusions
LA was confirmed to be significantly asymmetric in H-IA. Because outcome of surgical repair involving a midline incision, such as posterior sagittal anorectoplasty could be impaired, pediatric surgeons are advised to plan surgical intervention for H-IA carefully and appropriately.


Similar content being viewed by others
References
Nievelstein RA, Hartwig NG, Vermeij-Keers C, Valk J (1993) Embryonic development of the mammalian caudal neural tube. Teratology 48(1):21–31. https://doi.org/10.1002/tera.1420480106
Wijers CH, van Rooij IA, Marcelis CL, Brunner HG, de Blaauw I, Roeleveld N (2014) Genetic and nongenetic etiology of nonsyndromic anorectal malformations: a systematic review. Birth Defects Res C Embryo Today 102(4):382–400. https://doi.org/10.1002/bdrc.21068
Morandi A, Borzani I, Macchini F, Brisighelli G, Consonni D, Leva E (2016) Correlation between magnetic resonance imaging findings after posterior sagittal anorectoplasty for anorectal malformations and the clinical outcome: preliminary report. J Pediatr Surg 51(11):1859–63. https://doi.org/10.1016/j.jpedsurg.2016.07.009
Peña A (1986) Posterior sagittal approach for the correction of anorectal malformations. Adv Surg 19:69–100
Georgeson K (2007) Laparoscopic-assisted anorectal pull-through. Semin Pediatr Surg 16(4):266–9. https://doi.org/10.1053/j.sempedsurg.2007.06.009
Madhusmita GRG, Mittal MK, Bagga D (2018) Anorectal malformations: Role of MRI in preoperative evaluation. Indian J Radiol Imaging 28(2):187–94. https://doi.org/10.4103/ijri.ijri_113_17
Watanabe Y, Ando H, Seo T, Kaneko K, Katsuno S, Shinohara T et al (2003) Three-dimensional image reconstruction of an anorectal malformation with multidetector-row helical computed tomography technology. Pediatr Surg Int 19(3):167–71. https://doi.org/10.1007/s00383-002-0911-3
Watanabe Y, Takasu H, Sumida W, Mori K (2013) Wide variation in anal sphincter muscles in cases of high- and intermediate-type male anorectal malformation. Pediatr Surg Int 29(4):369–73. https://doi.org/10.1007/s00383-012-3250-z
Ueno S, Yokoyama S, Soeda J, Tajima T, Mitomi T, Suto Y et al (1995) Three-dimensional display of the pelvic structure of anorectal malformations based on CT and MR images. J Pediatr Surg 30(5):682–6. https://doi.org/10.1016/0022-3468(95)90690-8
Zhan Y, Wang J, Guo WL (2019) Comparative effectiveness of imaging modalities for preoperative assessment of anorectal malformation in the pediatric population. J Pediatr Surg 54(12):2550–3. https://doi.org/10.1016/j.jpedsurg.2019.08.037
McHugh K (1998) The role of radiology in children with anorectal anomalies; with particular emphasis on MRI. Eur J Radiol 26(2):194–9. https://doi.org/10.1016/s0720-048x(97)00095-8
Aslam A, Grier DJ, Duncan AW, Spicer RD (1998) The role of magnetic resonance imaging in the preoperative assessment of anorectal anomalies. Pediatr Surg Int 14(1–2):71–3. https://doi.org/10.1007/s003830050439
Thomeer MG, Devos A, Lequin M, De Graaf N, Meeussen CJ, Meradji M et al (2015) High resolution MRI for preoperative work-up of neonates with an anorectal malformation: a direct comparison with distal pressure colostography/fistulography. Eur Radiol 25(12):3472–9. https://doi.org/10.1007/s00330-015-3786-0
Li L, Ren X, Xiao H, Wang C, Xu H, Ming A et al (2020) Normal anorectal musculatures and changes in anorectal malformation. Pediatr Surg Int 36(1):103–11. https://doi.org/10.1007/s00383-019-04583-1
Davies MC, Creighton SM, Wilcox DT (2004) Long-term outcomes of anorectal malformations. Pediatr Surg Int 20(8):567–72. https://doi.org/10.1007/s00383-004-1231-6
Yang J, Zhang W, Feng J, Guo X, Wang G, Weng Y et al (2009) Comparison of clinical outcomes and anorectal manometry in patients with congenital anorectal malformations treated with posterior sagittal anorectoplasty and laparoscopically assisted anorectal pull through. J Pediatr Surg 44(12):2380–3. https://doi.org/10.1016/j.jpedsurg.2009.07.064
Chung PHY, Wong CWY, Wong KKY, Tam PKH (2018) Assessing the long term manometric outcomes in patients with previous laparoscopic anorectoplasty (LARP) and posterior sagittal anorectoplasty (PSARP). J Pediatr Surg 53(10):1933–6. https://doi.org/10.1016/j.jpedsurg.2017.10.058
Tong QS, Tang ST, Pu JR, Mao YZ, Wang Y, Li SW et al (2011) Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: intermediate results. J Pediatr Surg 46(8):1578–86. https://doi.org/10.1016/j.jpedsurg.2011.04.059
Yazaki Y, Koga H, Ochi T, Okawada M, Doi T, Lane GJ et al (2016) Surgical management of recto-prostatic and recto-bulbar anorectal malformations. Pediatr Surg Int 32(10):939–944. https://doi.org/10.1007/s00383-016-3948-4
Desai SN, Choudhury H, Joshi P, Pargewar S (2018) Magnetic resonance imaging evaluation after anorectal pull-through surgery for anorectal malformations: a comprehensive review. Pol J Radiol 83:e348–e52. https://doi.org/10.5114/pjr.2018.77791
Frush DP, Donnelly LF, Rosen NS (2003) Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 112(4):951–7. https://doi.org/10.1542/peds.112.4.951
Brenner D, Elliston C, Hall E, Berdon W (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176(2):289–96. https://doi.org/10.2214/ajr.176.2.1760289
Rice HE, Frush DP, Farmer D, Waldhausen JH (2007) Review of radiation risks from computed tomography: essentials for the pediatric surgeon. J Pediatr Surg 42(4):603–7. https://doi.org/10.1016/j.jpedsurg.2006.12.009
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyake, Y., Ochi, T., Yamashiro, Y. et al. Levator ani asymmetry and deviation in high-type anorectal malformation evaluated by magnetic resonance imaging. Pediatr Surg Int 38, 749–753 (2022). https://doi.org/10.1007/s00383-022-05104-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05104-3