Abstract
Background
Pancreatoblastoma is a very rare malignant pancreatic tumor in children. Pancreatoblastoma is the most common pancreatic tumor in children less than 10 years of age, accounting for 25% of the pancreatic neoplasm. There were only a few published literatures about the standardized diagnostic and management protocol for PB in the last decade.
Objective
To summarize our experience in the management of pancreatoblastoma in children and adolescents with emphasis on the presentation, diagnosis, treatment, and outcomes. A management strategy will also be discussed.
Methods
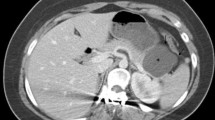
This was a retrospective case-series study of all pancreatoblastoma in patients < 18 years of age who were treated at Beijing children’s hospital (BCH) from January 2002–January 2015. The diagnoses of PB were confirmed by histopathology analysis of the resected specimen. The variables being analyzed included patient demographics, age at diagnosis, clinical presentation, tumor size, metastasis if present, tumor markers (AFP), type of surgery, length of follow-up, and outcome. The assessment of the tumor location, size, extent of the tumor, and distant metastasis was made by ultrasound (US), computed tomography (CT), and/or magnetic resonance imaging (MRI).
Result
21 patients with pancreatoblastoma were diagnosed at a median age of 4 years, 7 girls, and 14 boys. The diagnosis of pancreatoblastoma was identified by the histology examination. The most common syndrome was abdominal mass (n = 11), followed by abdominal pain (N = 10), elevated serum AFP levels were noted in almost all cases (17/18), 17 patients with disease initially unresectable on diagnosis accepted neo-adjuvant chemotherapy consisting of CDV, OPEC, PLADO, IEV, and AVCP. All patients underwent surgery, including pancreaticoduodenectomy (Whipple’s procedure), the Pylorus-preserving pancreaticoduodenectomy (traverse-Longmire procedure), Spleen-preserving distal pancreatectomy, and distal pancreatectomy with en bloc splenectomy, Roux-en-Y end-to-end pancreatojejunostomy. In all, 13 children were disease free with a median follow-up of 53 months (range 11–156 months).
Conclusions
The pancreatoblastoma in children and adolescents is a malignant tumor. Complete resection combined with chemotherapy is associated with long-term survival. For the unresectable tumor at diagnosis, preoperative chemotherapy was recommended to reduce tumor volume. AFP is critical for diagnosis and monitoring the disease as a tumors marker.
Similar content being viewed by others
References
Ellerkamp V, Warmann SW, Vorwerk P et al (2012) Exocrine pancreatic tumors in childhood in Germany. Pediatr Blood Cancer 58:366–371
Chun Y, Kim W, Park K et al (1997) Pancreatoblastoma. J Pediatr Surg 32:1612–1615
Perez EA, Gutierrez JC, Koniaris LG et al (2009) Malignant pancreatic tumors: incidence and outcome in 58 pediatric patients. J Pediatr Surg 44:197–203
Shorter NA, Glick RD, Klimstra DS et al (2002) Malignant pancreatic tumors in childhood and adolescence: the Memorial Sloan-Kettering experience, 1967 to present. J Pediatr Surg 37:887–892
Lee YJ, Hah JO (2007) Long-term survival of pancreatoblastoma in children. J Pediatr Hematol Oncol 29:845–847
Dhebri AR, Connor S, Campbell F et al (2004) Diagnosis, treatment and outcome of pancreatoblastoma. Pancreatology 4:452–453
Bien E, Godzinski J, Dall’Igna P et al (2011) Pancreatoblastoma: a report from the European cooperative study group for paediatric rare tumours (EXPeRT). Eur J Cancer 47:2347–2352
Becker WF (1957) Pancreatoduodenectomy for carcinoma of the pancreas in an infant; report of a case. Ann Surg 145:1601–1603
Horie A, Yano Y, Kotoo Y et al (1977) Morphogenesis of pancreatoblastoma, infantile carcinoma of the pancreas: report of two cases. Cancer 39:247–254
Cao L, Liu D (2007) Diagnosis and treatment of pancreatoblastoma in China. Pancreas 34:92–95
Brecht IB, Schneider DT, Klöppel G et al (2011) Malignant pancreatic tumors in children and young adults: evaluation of 228 patients identified through the surveillance, epidemiology, and end result (SEER) database. Klinische Pädiatrie 223:341–345
Glick RD, Pashankar FD, Pappo A et al (2012) Management of pancreatoblastoma in children and young adults. J Pediatr Hematol Oncol 34(Suppl 2):S47–S50
Thorner P, Wesson DK, Filler RM et al (1992) A 20-year review of pediatric pancreatic tumors. J Pediatr Surg 27:1315–1317
Yang X, Wang X (2010) Imaging findings of pancreatoblastoma in 4 children including a case of ectopic pancreatoblastoma. Pediatr Radiol 40:1609–1614
Szerlip NJ, Fox E, Manosca F et al (2007) Pancreatoblastoma metastases to the brain. Case illustration. J Neurosurg 106:169
Montero M, Vázquez JL, Páramo C et al (2005) Pancreatoblastoma associated with incomplete Beckwith–Wiedemann syndrome: case report and review of the literature. J Pediatr Surg 40:1341–1344
Laje P, Palladino AA, Bhatti TR et al (2013) Pancreatic surgery in infants with Beckwith–Wiedemann syndrome and hyperinsulinism. J Pediatr Surg 48:2511–2516
Abraham SC, Wu TT, Klimstra DS et al (2001) Distinctive molecular genetic alterations in sporadic and familial adenomatous polyposis-associated pancreatoblastomas : frequent alterations in the APC/β-catenin pathway and chromosome 11p. Am J Pathol 159:1619–1627
Sorrentino S, Conte M, Nozza P et al (2010) Simultaneous occurrence of pancreatoblastoma and neuroblastoma in a newborn with Beckwith–Wiedemann syndrome. J Pediatr Hematol Oncol 32:e207–e209
Xu C, Zhong L, Wang Y, Wang W, Yang Z, Kang X, Wang C (2012) Clinical analysis of childhood pancreatoblastoma arising from the tail of the pancreas. J Pediatr Hematol Oncol 34(5):e177–e181. https://doi.org/10.1097/MPH.0b013e318253f0e1
Wood LD, Klimstra DS (2014) Pathology and genetics of pancreatic neoplasms with acinar differentiation. Semin Diagn Pathol 31:491–497
Vannier JP, Flamant F, Hemet J et al (1991) Pancreatoblastoma: response to chemotherapy. Pediatr Blood Cancer 19:187–191
Ogawa T, Okinaga K, Obana K et al (2000) Pancreatoblastoma treated by delayed operation after effective chemotherapy ☆. J Pediatr Surg 35:1663–1665
Yonekura T, Kosumi T, Hokim M et al (2006) Aggressive surgical and chemotherapeutic treatment of advanced pancreatoblastoma associated with tumor thrombus in portal vein. J Pediatr Surg 41:596–598
Défachelles AS, Martin DLE, Boutard P et al (2001) Pancreatoblastoma in childhood: clinical course and therapeutic management of seven patients. Pediatr Blood Cancer 37:47–52
Murakami T, Ueki K, Kawakami H et al (1996) Pancreatoblastoma: case report and review of treatment in the literature. Pediatr Blood Cancer 27:193–197
Barenboimstapleton L, Yang X, Tsokos M et al (2005) Pediatric pancreatoblastoma: histopathologic and cytogenetic characterization of tumor and derived cell line. Cancer Genet Cytogenet 157:109–117
Ohata R, Okazaki T, Ishizaki Y (2010) Pancreaticoduodenectomy for pancreatoblastoma: a case report and literature review. Pediatr Surg Int 26:447–450
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Y., Yang, W., Hu, J. et al. Diagnosis and treatment of pancreatoblastoma in children: a retrospective study in a single pediatric center. Pediatr Surg Int 35, 1231–1238 (2019). https://doi.org/10.1007/s00383-019-04524-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04524-y