Abstract
Aim
The objective of the present study was to evaluate the diagnostic methods, concomitant organ injuries, factors affecting mortality and morbidity, treatment methods, and outcomes of patients treated for traumatic gastrointestinal (GI) perforation.
Materials and methods
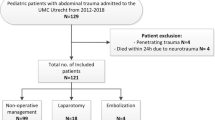
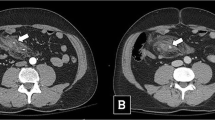
We conducted a retrospective review of the medical records of 96 patients who had been treated for GI perforation between January 2000 and October 2015. Data were collected and organised according to the following categories: general patient information, age, gender, hospitalisation period, trauma mechanisms, concomitant injuries, radiological assessment, diagnosis and treatment methods, treatment forms, and complications. The cases were divided into two groups, blunt and penetrating traumas, and the patients within each group were compared. Colorectal trauma cases were not included in this study. Patients suspected of a GI perforation were assessed by standing plain abdominal radiograph (SPAR) and ultrasound scan (US). Patients who had a normal SPAR, and showed free or viscous fluid in the abdomen on US underwent computed tomography (CT) scanning. Surgery was performed if patients displayed free air in the abdomen on a SPAR or CT scan, showed viscous fluid without any additional injury, provided normal radiological images but displayed signs of peritonitis, or were clinically unstable. The patients were scored according to the Injury Severity Score (ISS) system.
Results
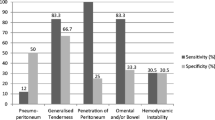
In total, 96 patients, with an average age of 10.3 ± 4 years (1–17 years) and diagnosed with a GI perforation, were reviewed retrospectively. The patients included 88 (91 %) males and 8 (9 %) females. The presence of free air on SPAR was detected in 42 (52 %) patients, whereas no free air was detected in 39 (48 %) patients. Non-specific significant findings were detected in 45 (76 %) out of 59 patients by USS, and in 78 % of patients by CT (viscous fluid, fluid, free air). The most affected organ was the ileum, which was detected in 37 (39 %) patients. Primary repair was performed on 71 (74 %) patients, while resection was performed on 22 (23 %); 3 (3 %) patients underwent an ostomy. Ten (10 %) patients experienced complications and five (5 %) patients died. The ISS scores for blunt and penetrating traumas were 14, 15 and no significant difference was detected between the scores (p > 0.05).
Conclusions
Although the complication rate for patients with penetrating trauma was higher than for those with blunt trauma, the rate of mortality increased in patients with blunt trauma. Free air may not be detected by SPAR even if a GI perforation exists. Since diagnostic challenges may increase the rate of mortality and morbidity in GI perforations, we believe that a combination of radiological imaging and rapid abdominal examination is important in cases where SPAR cannot detect free air.

Similar content being viewed by others
References
Baeza-Herrera C, García-Cabello LM, Gardida-Chavarria R et al (2000) Traumatic perforation of the small intestine in childhood. Gac Med Mex 136:547–553
Başaklar AC, Türkyılmaz Z (2006) Karın ve Göğüs Travması. In: Başaklar AC (ed) Bebek ve Çocukların Cerrahi ve Ürolojik Hastalıkları. Palme Yayıncılık, Ankara, pp 1015–1051
Berkgerden S, Aksöylek S, Ertekin C et al (1989) Çocuklarda künt karın travmaları. Pediatrik Cerrahi Dergisi 3:24–27
Duman L (2007) Abdominal trauma in children. J Ank Univ Fac Med 60(4):180–183
Bass BL, Eichelberger MR, Schisgall R et al (1984) Hazards of nonoperative therapy of hepatic injury in children. J Trauma 24:978–982
Letton RW Jr, Worrell V, Tuggle DW (2010) American pediatric surgical association committee on trauma blunt intestinal injury study group. Delay in diagnosis and treatment of blunt intestinal perforation does not adversely affect prognosis in the pediatric trauma patient. J Trauma 68:790–795
Grosfeld JL, Rescorla FJ, West KW et al (1989) Gastrointestinal injuries in childhood: analysis of 53 patients. J Pediatr Surg 24:580–583
Mukhopadhyay M (2009) Intestinal injury from blunt abdominal trauma: a study of 47 cases. Oman Med J 24:256–259
Jamieson DH, Babyn PS, Pearl R (1996) Imaging gastrointestinal perforation in pediatric blunt abdominal trauma. Pediatr Radiol 26:188–194
Oztürk H, Onen A, Otçu S et al (2003) Diagnostic delay increases morbidity in children with gastrointestinal perforation from blunt abdominal trauma. Surg Today 33:178–182
Beckmann KR, Nozicka CA (2000) Small bowel perforation: an unusual presentation for child abuse. J Am Osteopath Assoc 100:496–497
Bulas DI, Taylor GA, Eichelberger MR (1989) The value of CT in detecting bowel perforation in children after blunt abdominal trauma. AJR Am J Roentgenol 153:561–564
Maull KI, Reath DB (1984) Impact of early recognition on outcome in nonpenetrating wounds of the small bowel. South Med J 77:1075–1077
Ulman I, Avanoğlu A, Ozcan C et al (1996) Gastrointestinal perforations in children: a continuing challenge to nonoperative treatment of blunt abdominal trauma. J Trauma 41:110–113
Coppolino F, Gatta G, Di Grezia G (2013) Gastrointestinal perforation: ultrasonographic diagnosis. Crit Ultrasound J 15:5
Stengel D, Bauwens K, Sehouli J et al (2001) Systematic review and meta-analysis of emergency ultrasonography for blunt abdominal trauma. Br J Surg 88:901–912
Abbas SM, Upadhyay V (2007) Hollow viscus injury in children: starship Hospital experience. World J Emerg Surg 4(2):14
Hunt KE, Garrison RN, Fry DE (1980) Perforating injuries of the gastrointestinal tract following blunt abdominal trauma. Am Surg 46:100–104
Chirdan LB, Uba AF, Chirdan OO (2008) Gastrointestinal injuries following blunt abdominal trauma in children. Niger J Clin Pract 11:250–253
Baker SP, O’Neill B, Haddon W Jr, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Acknowledgments
The English in this document has been checked by at least two professional editors, both native speakers of English (Textcheck reference number: 16053002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Arslan, S., Okur, M.H., Arslan, M.S. et al. Management of gastrointestinal perforation from blunt and penetrating abdominal trauma in children: analysis of 96 patients. Pediatr Surg Int 32, 1067–1073 (2016). https://doi.org/10.1007/s00383-016-3963-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3963-5