Abstract
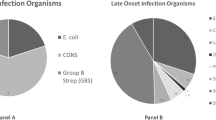
This study aimed to define the incidence, causative organisms and predisposing factors leading to infection related morbidity in newborns with gastroschisis. All gastroschisis patients admitted over the 5-year period (1999–2004) were retrospectively reviewed. Surveillance samples, wound, blood, urine and fecal cultures were analyzed. Duration of total parenteral nutrition, antibiotic therapy, feeding regimes and demographic data were also analyzed. Multiple logistic regression was employed using the SPSS system and p < 0.05 was considered as significant. Seventy-two neonates were identified with 53% having abnormal gut carriage mostly due to Enterobacter and Klebsiella. Wound infection occurred in 20% of cases. Abnormal gut carriage predisposed to the development of wound infection. Line sepsis occurred in 21% of neonates. Endogenous coagulase negative Staphylococcus caused 74% of septic episodes. There was no correlation between abnormal gut carriage and the development of line sepsis. Overall survival was 96%. The cause of infections in gastroschisis patients appears to be multifactorial. A multidisciplinary team can play an important role in reducing the incidence of infections. Strict aseptic protocols and auditing practice can be the invaluable tools in decreasing morbidity rates.
Similar content being viewed by others
References
Kilby DM (2006) The incidence of gastroschisis. BMJ 332:250–251. doi:10.1136/bmj.332.7536.250
Salihu HM, Emusu D, Aliyu ZY, Pierre-Louis BJ, Druschel CM, Kirby RS (2004) Mode of delivery and neonatal survival of infants with isolated gastroschisis. Obstet Gynecol 104:678–683
Sarginson RE, Taylor N, van Saene HFK (2001) Management of infections in the critically ill: glossary of terms and definitions. Curr Anaesth Crit Care 12:2–5. doi:10.1054/cacc.2001.0316
van Saene HFK, Damjanovic V, Alcock SR (2001) Management of infections in the critically ill: basics in microbiology for the patient requiring intensive care. Curr Anaesth Crit Care 12:6–17. doi:10.1054/cacc.2001.0317
Silvestri L, Mannucci F, van Saene HFK (2001) Selective decontamination of the digestive tract. J Hosp Infect 48(4):322–324. doi:10.1053/jhin.2001.0986
Tan KH, Kilby MD, Whittle MJ, Beattie BR, Booth IW, Botting BJ (1996) Congenital anterior abdominal wall defects in England and Wales 1987–1993: retrospective analysis of OPCS data. BMJ 313:903–906
Rankin J, Pattenden SW, Abramsky L et al (2005) Prevalence of congenital anomalies in five British regions. Arch Dis Child Fetal Neonatal Ed 5:F374–F379. doi:10.1136/adc.2003.047902
Sydorak RM, Nijagal A, Sbragia L et al (2002) Gastroschisis: small hole, big cost. J Pediatr Surg 37(12):1669–1672. doi:10.1053/jpsu.2002.36689
Driver CP, Bruce J, Bianchi A, Doig CM, Dickson AP, Bowen J (2000) The contemporary outcome of gastroschisis. J Pediatr Surg 35(12):1719–1723. doi:10.1053/jpsu.2000.19221
Molik KA, Gingalewski CA, West KW et al (2001) Gastroschisis: a plea for risk categorization. J Pediatr Surg 36(1):51–55. doi:10.1053/jpsu.2001.20004
Vilela PC, Ramos DMM, Falbo GH, Santos LC (2001) Risk factors for adverse outcome of newborns with gastroschisis in a Brazilian Hospital. J Pediatr Surg 36(4):559–564. doi:10.1053/jpsu.2001.22282
Snyder CL (2000) Outcome analysis for gastroschisis. J Pediatr Surg 35(2):398–399
Sakala EP, Erhard LN, White JJ (1993) Elective caesarian section improves outcomes of neonates with gastroschisis. Am J Obstet Gynecol 169(4):1050–1053
How HY, Harris BJ, Pietrantoni M et al (2000) Is vaginal delivery preferable to elective caesarean delivery in fetuses with a known ventral wall defect? Am J Obstet Gynecol 182(6):1527–1534. doi:10.1067/mob.2000.106852
van Saene HFK, Taylor N, Donnell SC et al (2003) Gut overgrowth with abnormal flora: the missing link in parenteral nutrition–related sepsis in surgical neonates. Eur J Clin Nutr 57:548–553. doi:10.1038/sj.ejcn.1601578
Donnell SC, Taylor N, van Saene HFK, Magnall VL, Pierro A, Lloyd DA (2002) Infection rates in surgical neonates and infants receiving parenteral nutrition: a five year prospective study. J Hosp Infect 52:273–280. doi:10.1053/jhin.2002.1318
Pierro A, van Saene HFK, Jones MO, Brown D, Nunn AJ, Lloyd DA (1998) Clinical impact of abnormal gut flora in infants receiving parenteral nutrition. Ann Surg 227(4):547–552. doi:10.1097/00000658-199804000-00016
Cruccetti A, Pierro A, Uronen H, Klein N (2003) Surgical infants on total parenteral nutrition have impaired cytokine responses to microbial challenge. J Pediatr Surg 38(1):138–142. doi:10.1053/jpsu.2003.50028
Singh SJ, Fraser A, Leditschke JF et al (2003) Gastroschisis: determinants of neonatal outcome. Pediatr Surg Int 19:260–265. doi:10.1007/s00383-002-0886-0
Okada Y, Klein N, van Saene HK, Pierro A (1998) Small volumes of enteral feedings normalise immune function in infants receiving parenteral nutrition. J Pediatr Surg 33(1):16–19. doi:10.1016/S0022-3468(98)90352-9
Roberts JP, Gollow IJ (1990) Central venous catheters in surgical neonates. J Pediatr Surg 25(6):632–634. doi:10.1016/0022-3468(90)90350-I
Tawil KA, Gilliam GL (1995) Gastroschisis: 13 years’ experience at RCH Melbourne. J Paediatr Child Health 31(6):553–556. doi:10.1111/j.1440-1754.1995.tb00883.x
Hall NJ, Hartley J, Ade Ajayi N et al (2005) Bacterial contamination of central venous catheters during insertion: a double blind randomised controlled trial. Pediatr Surg Int 21(7):507–511. doi:10.1007/s00383-005-1478-6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khalil, B.A., Baath, M.E., Baillie, C.T. et al. Infections in gastroschisis: organisms and factors. Pediatr Surg Int 24, 1031–1035 (2008). https://doi.org/10.1007/s00383-008-2210-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2210-0